Abstract
Primary objective:
To investigate the nature and patterns of conversational topics discussed by individuals with severe TBI and familiar communication partners at 3 and 6 months post-injury, and to examine changes occurring in conversational topics during sub-acute recovery.
Research design:
Qualitative content analysis was used to explore the nature of topics and generate conversational themes. Topic analysis provided an understanding of conversational topic management by identifying patterns of topic initiation and maintenance.
Methods:
Twenty-two people with severe TBI and a familiar communication partner engaged in a 10-minute casual conversation on self-selected topics at 3 and 6 months post-injury.
Main outcomes and results:
Three main conversational themes were identified: connecting; re-engaging; and impacts of injury. The nature of topics related to these themes changed over time to reflect participants’ sub-acute rehabilitation experiences. Most conversational dyads maintained similar conversational and topic patterns during sub-acute recovery.
Conclusions:
Qualitative analysis provides a new insight into the conversational topics of individuals with severe TBI. Many participants engaged in appropriate conversations and discussed mutually important topics with familiar communication partners. Findings may inform speech-language pathology intervention in sub-acute recovery to improve conversational discourse abilities of individuals with severe TBI and support their communication partners.
Keywords: Traumatic brain injury, communication, conversation topics, content analysis, qualitative, recovery
Introduction
Casual conversations are the most frequent communication act in which adults engage, providing a way to make sense of everyday life, construct personal identity and establish and maintain relationships [1,2]. A casual conversation is ‘talk … for the sake of talking’ ([2], p. 6) and does not seek to achieve a pragmatic goal. Nonetheless, casual conversations may address social and interpersonal goals. Impaired ability to effectively engage in conversations is often experienced following traumatic brain injury (TBI) [3], resulting in loss of friendships [4], social isolation and barriers to re-engaging in work, academic, community and family life [5].
Recovery following traumatic brain injury
Individuals have a unique recovery experience following TBI [6]. Physical impairments may improve within 6 months post-injury; however, cognitive, psychosocial and communication impairments can persist for several years [7–10]. Stages of recovery following TBI include acute, sub-acute and chronic timeframes [11]. Individuals in sub-acute recovery are medically stable, yet require rehabilitation to facilitate recovery and transition from inpatient to community settings [12].
Recovery of conversational abilities during sub-acute recovery following TBI has not been empirically examined. Snow et al. [8] argue that research should focus on conversational discourse during this timeframe to identify early changes or impairments in conversational abilities. Early identification of these impairments may support speech-language pathology (SLP) intervention in sub-acute rehabilitation programmes. Targeted intervention can address maladaptive behaviours that contribute to the conversations of people with TBI being viewed as unrewarding and inappropriate [8,13].
Conversational and topic patterns following traumatic brain injury
Conversational discourse refers to interactive communication and encompasses patterns of conversational structure such as contributions of speakers and topic management (i.e. introducing and maintaining topics) [8,14–16]. People with TBI may demonstrate conversational discourse impairments, including reduced topic management skills and difficulty expressing content logically [3,17,18]. Two previous case-studies have explored the conversational and topic patterns of people with TBI. Mentis and Prutting [17] compared the topic management skills of a 24-year old male (4 years post-TBI), with a non-injured control during a 20-minute unstructured conversation with a familiar communication partner (unspecified relationship). Topic analysis revealed the participant with TBI demonstrated difficulty introducing and maintaining topics. Friedland and Miller [19] used conversation analysis to study social communication during 10-minute casual conversations of a 43-year old male, 9 months post-injury. Communication partners included an investigator, the participant’s mother and his wife. In contrast to Mentis and Prutting’s findings, the participant actively introduced and maintained topics. The conflicting findings may reflect different measures of analyses, time post-injury or length of conversation. Additionally, these are single case-studies of male participants in later stages of recovery.
Coelho et al. [3,20] investigated the conversational and topic patterns of individuals with TBI in two group studies. Participants with and without TBI engaged in a 15-minute, unguided conversation with an investigator. Participants with TBI introduced fewer topics than non-injured controls. However, both studies used investigators as conversational partners. The nature of the interpersonal relationship between dyads may have influenced the conversational behaviours of participants with TBI [3]. Additionally, most participants with TBI were in the chronic stage of recovery. Further studies are therefore required to understand the conversational and topic patterns of individuals in sub-acute recovery following severe TBI.
Nature of conversational topics
Conversational and topic patterns affect the structure and flow of interactions; however, the quality of a conversation is also linked to the nature of topics that are discussed. Talking about topics that are interesting to an individual may help them to establish, maintain and enjoy conversations. Furthermore, conversations may be negatively perceived when topics are not interesting or relevant to communication partners [13].
Sociolinguistic research findings suggest that people without communication impairments discuss topics about everyday activities, work, family and social issues [21–23]. This area has received scant attention in TBI research. Body and Parker [24] investigated topic repetitiveness in a 65-year old male with TBI who engaged in two 15-minute conversations with either his wife or a friend. Topics focused on issues that were personally relevant to the participant with TBI (e.g. gardening, family holiday). Time post-injury, severity of injury and method of analysis were not reported; hence, this is an area of conversational discourse requiring further investigation.
To date, no studies have used qualitative analysis to investigate conversational topics of people with TBI. Qualitative analysis offers a rich approach for exploring conversations by addressing how people with TBI use topics to express meaningful events during sub-acute recovery.
Influence of communication partners
Communication partners can influence the conversational abilities of people with TBI, particularly if there is a power imbalance [25–28]. Unfamiliar communication partners may excessively question people with TBI to check their comprehension, use slower speech and patronising comments or limit opportunities for them to participate in conversations [28]. However, the influence of communication partners on the nature of conversational topics is a neglected area of research in TBI literature. Investigating conversations with familiar communication partners will provide insights into how people with TBI communicate in their day-to-day lives and potentially identify targets for communication partner training, which can facilitate effective interactions between people with TBI and trained communication partners [29–31]. As sub-acute recovery is a time of major physical recovery and psychosocial change, such intervention may assist with navigating the recovery process by encouraging the discussion of particular topics with people in core social networks.
Aims
This qualitative study aimed to investigate casual conversations of individuals with severe TBI and familiar communication partners during sub-acute recovery. The following research questions were addressed:
What is the nature of conversational topics discussed by people with severe TBI and familiar communication partners at 3 and 6 months post-injury, and does the nature of these topics change during sub-acute recovery?
What are the conversational and topic patterns present in conversations between people with severe TBI and familiar communication partners at 3 and 6 months post-injury, and do these patterns change during sub-acute recovery?
Method
Data used in this study was collected for a longitudinal project investigating communication recovery following severe TBI [32]. Participants were recruited as an inception cohort and followed up over 2 years. The longitudinal project involved a comprehensive SLP assessment battery, including a casual conversation between participants with TBI and a familiar communication partner. This exploratory study presents conversational data collected at 3 and 6 months post-injury.
Research approach
A qualitative descriptive approach was adopted to investigate the nature and patterns of conversational topics discussed by people with severe TBI and familiar communication partners during sub-acute recovery. Located within an interpretive paradigm [33], qualitative description draws upon principles of naturalistic inquiry to examine real-world situations as they occur [34].
Sampling procedure
Purposive sampling was used to recruit participants for the longitudinal study from three metropolitan brain injury rehabilitation units (BIRUs) in Sydney, Australia. A staff member from each site approached suitable patients and requested permission for the project manager to contact them. Patients who met the following eligibility criteria were invited to participate:
aged 16–65 years at the time of injury;
diagnosis of severe TBI: Glasgow Coma Scale (GCS) score of 8 or less and/or period of post-traumatic amnesia (PTA) greater than 24 hours;
emerged from PTA and deemed medically fit to participate;
able to attempt SLP and cognitive neuropsychological assessments in English; and
nil history of neurological illness/injury or significant medical history (e.g. developmental delay; dementia; current substance abuse).
Participants from the longitudinal cohort were selected for the current study if they met two additional criteria:
consent was provided for conversations to be audio and/or video recorded; and
the same communication partner was available to participate at both 3 and 6 months post-injury.
Demographic profile of participants with TBI
Twenty-two adults with severe TBI participated in this study. Table I presents participants’ demographic information. There were 19 males and three females, reflecting the higher incidence rate of TBI in males [35,36]. Participants were aged between 16−59 years at the time of injury (mean = 36.5, SD = 13.8). Duration of PTA ranged from 3−122 days (mean = 52.8, SD = 32.6), consistent with severe TBI [37]. Motor vehicle accidents (MVAs) were the most frequent cause of injury. Pre-injury education ranged from 8−20 years (mean = 13.9, SD = 3.2). The highest level of education attained ranged from high school to tertiary levels. Participants were employed in diverse occupations or studying at the time of injury. Two participants were bilingual and one was multilingual. Participants sustained extensive brain injuries, as indicated on computed tomography (CT) brain scans. The majority had right hemisphere and/or frontal lobe damage. Underlying neuropathology for each participant is presented in Table I.
Table I.
Demographic profile of participants with TBI.
| PARa | Age at injury (years) | Gender | PTA (days) | Trauma type | Highest education attained | Occupation classificationb | Language status | CT scan |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Andrew | 42 | Male | 109 | Fall | TAFE | Machinery operators and drivers | Monolingual | Axonal shearing |
| Tony | 45 | Male | 122 | MVA | University | Professionals | Monolingual | (L) fontal contusion, axonal shearing, (R) basal ganglia |
| Emily | 16 | Female | 63 | MVA | ≤ Year 12 | Sales workers | Monolingual | Parietal SDH, (R) SAH, contusions fronto-temporal |
| Peter | 45 | Male | 13 | MVA | ≤ Year 10 | Machinery operators and drivers | Monolingual | (L) SAH and (L) cerebral contusions |
| Li | 28 | Male | 86 | MVA | University | Technicians and trade workers | Multilingual | DAI, SAH (R) frontal |
| Steven | 46 | Male | 47 | MVA | TAFE | Managers | Bilingual | (L) hemisphere contusions, SAH (L) frontal region |
| Mark | 54 | Male | 18 | MVA | ≤ Year 12 | Sales workers | Monolingual | SAH (R) frontal sulci, internal capsule haemorrhage |
| Amanthi | 33 | Female | 103 | MVA | ≤ Year 10 | Community and personal service workers | Bilingual | (L) hemisphere haemorrhage, basal ganglia, midbrain |
| Chris | 43 | Male | 3 | Assault | ≤ Year 10 | Labourers | Monolingual | SDH, SAH |
| Sharon | 56 | Female | 50 | MVA | University | Professionals | Monolingual | Contusions (R) posterior frontal region |
| Ben | 28 | Male | 64 | MVA | TAFE | Technicians and trade workers | Monolingual | (L) frontal/temporal, (R) frontal lobe |
| Scott | 40 | Male | 48 | Fall | TAFE | Labourers | Monolingual | Frontal lobe involvement |
| John | 59 | Male | 42 | Assault | ≤ Year 10 | Machinery operators and drivers | Monolingual | (L) SAH, (L) frontal lobe haemorrhage |
| Josh | 18 | Male | 47 | MVA | ≤ Year 12 | Technicians and trade workers | Monolingual | Punctate haemorrhage (R) frontal |
| Paul | 32 | Male | 34 | Assault | TAFE | Technicians and trade workers | Monolingual | Temporal contusion (L), SAH, parieto-temporal SDH |
| Jack | 17 | Male | 28 | MVA | ≤Year 10 | Machinery operators and drivers | Monolingual | Brainstem contusions, bilateral parieto-occipital SDH |
| James | 21 | Male | 62 | Fall | ≤Year 12 | Student | Monolingual | Fronto-temporal cerebellar injuries, (L) skull fracture |
| Daniel | 23 | Male | 90 | MVA | ≤Year 10 | Labourers | Monolingual | (R) SDH, traumatic SAH |
| Luke | 18 | Male | 48 | Fall | ≤Year 12 | Student | Monolingual | (L) fronto-temporal SDH/SAH, (L) frontal DAI |
| Greg | 53 | Male | 6 | Fall | TAFE | Technicians and trades workers | Monolingual | (R) occipital bone fracture |
| Michael | 38 | Male | 38 | MVA | University | Managers | Monolingual | (R) basal ganglia, midbrain, SAH (L) frontal, (R) parietal |
| Shane | 49 | Male | 41 | MVA | University | Managers | Monolingual | DAI, (L) intracranial haemorrhage, facial fractures |
PAR, participant with TBI; PTA, post-traumatic amnesia; TAFE, Technical and Further Education; MVA, motor vehicle accident; (L), Left; (R), Right; SDH, subdural haemorrhage; SAH, subarachnoid haemorrhage; DAI, diffuse axonal injury.
Pseudonyms were used to protect participants’ identity.
Classification according to Australian Bureau of Statistics [38].
Communication profile of participants with TBI
Participants completed a range of communication assessments for the longitudinal study. Fifteen participants were diagnosed with more than one communication impairment. An overview of participants’ communication ability at the initial data collection point for this study (i.e. 3 months post-injury) is available online as a supplemental file.
Thirteen participants were diagnosed with aphasia according to an aphasia quotient (AQ) of less than or equal to 93.8 on the Western Aphasia Battery-Revised (WAB-R) [39]. Twelve participants were diagnosed with mild anomia, while one was diagnosed with severe Broca’s aphasia. One participant was legally blind and could not complete the WAB-R. Twenty participants were diagnosed with dysarthria, indicated by a score of 7 or less on at least one item within the Frenchay Dysarthria Assessment-Second Edition (FDA-2) [40].
The La Trobe Communication Questionnaire (LCQ) [41] measured the perceived social communication skills of participants with TBI based on information provided by communication partners. Scores closer to 30 indicate perceptions of higher levels of social communication ability. Participant scores ranged from 31−104 (mean = 54.6, SD = 17.92), indicating large variation in participants’ perceived social communication. However, the mean score is within 1 SD of the mean of the LCQ norms for non-injured adults (mean = 47.17, SD = 9.93) [41].
Communication partners
Each participant with TBI selected a communication partner for the conversation component of this study. All participants selected a family member, with 10 parents, nine spouses, one sister and one daughter. There were 20 female and two male communication partners aged between 21–66 years (mean = 45.7, SD = 11.1). The length of relationship prior to injury ranged from 12−43 years (mean = 23.8, SD = 8.8). Further information about communication partners can be found online (supplemental file).
Data collection
The measure for this study was two 10-minute casual conversations between participants with TBI and their chosen communication partner. A 10-minute sample has been shown to reflect typical conversational content and patterns [42]. The first conversation took place at ~ 3 months post-injury. The second conversation occurred at least 3 months after the first, at ~ 6 months post-injury.
Conversations took place in BIRUs, transitional living units, external health services and participants’ homes. Most participants were inpatients at 3 months post-injury (n = 16), while all conversations were conducted in outpatient (n = 9) or community settings (n = 13) at 6 months post-injury. Conversations were audio and/or video recorded in a private setting (e.g. therapy room in a BIRU). Participants selected the audio only option if they were uncomfortable with video recordings. An investigator (author two or four) instructed participants, ‘I am going to leave the room for 10 minutes. I want you to have a chat while I am gone’. If participants asked what to talk about they were advised, ‘it can be about anything you would normally talk about with each other’. The investigator left the recording setting for the duration of the conversation. Participants were encouraged to continue if they exited the research room before 10 minutes.
Transcription
Recorded conversations were transcribed orthographically using CLAN software by the first author and an SLP research student who was independent to this study. Both were blinded to data collection point. Conversations were segmented into utterances according to: (1) syntax (a well formed question); (2) intonation (rising or falling); (3) pauses; and (4) semantics (speaker introduces new content) [43,44]. Data was transcribed in entirety with the exclusion of identifying information, task instructions or external interruptions (e.g. investigator entering the room). Internal interruptions (e.g. interruptions from non-communication partners), indicators of non-verbal communication and unintelligible speech were also transcribed. There were four steps for data transcription: (1) online transcription; (2) check completed transcription against audio/video sample; (3) review transcription discrepancies; and (4) re-check entire transcription.
Analysis
The first 10 minutes of each conversation were analysed with the exception of internal interruptions. Data analysis comprised two major stages: qualitative content analysis to describe the nature of topics, and topic analysis to explore conversational and topic patterns.
Content analysis
The first author analysed each transcript using qualitative content analysis [45]. Data collected at 3 months post-injury was analysed prior to data collected at 6 months post-injury. An inductive approach to content analysis was used [46]. No pre-existing categories were created to ensure the nature of topics discussed was derived from participants’ words [47,48]. Both manifest and latent content of the data were analysed [34,45]. Graneheim and Lundman [45] outlined five major stages of qualitative content analysis. Each is described below with an example from the data provided.
-
Identifying meaning units: A meaning unit is a group of words, sentences or paragraphs that relate to a central meaning through content and context [45]. For example, in the following exchange, the utterances of the participant with TBI (PAR) and his communication partner (COP) were linked to a discharge-related meaning unit:
PAR: When am I going home?
COP: I don’t know. Maybe this week.
-
Condensing meaning units: Meaning units were condensed and provided with a label that remained close to participants’ words. The meaning unit presented in step one was condensed to:
Participant might go home this week
-
Coding meaning units: Condensed meaning units were coded according to content. The condensed meaning unit in step two was coded:
Rehabilitation discharge
-
Creating categories: Categories were formed by grouping similar codes to describe what participants were discussing (i.e. manifest content) [45]. The following category included the code presented in step three:
Category: Discharge from rehabilitation
Included: Meaning units relating to discharge plans, wanting to be discharged from rehabilitation
-
Generating themes: Themes were generated by interpreting latent content and grouping categories with similar underlying meanings [34,45]. Group themes for each time point reflected themes that were evident in a minimum of 50% of conversations. When generating themes from data collected at 6 months post-injury, constant comparison occurred with themes generated from data collected at 3 months post-injury to examine consistency and change. The category in step four was included within the following theme:
Planning for re-engaging
Topic analysis
Topic analysis [17] was used to identify conversational and topic patterns as it is a sensitive and reliable method to evaluate topic management skills of people with and without TBI. Utterances in each conversation were identified as a topic, sub-topic or maintaining utterance. Mentis and Prutting [17] defined a topic as an idea presented in a clause or noun phrase that describes a series of utterances. A new topic occurred when an utterance did not relate to the main topic, nor contain content from a previous utterance. An utterance was coded as a sub-topic if it expanded on an aspect of a topic or contributed new information to a topic. Utterances were coded as maintaining moves if they expressed content related to a topic or sub-topic [17,49]. Maintaining utterances also included agreements, requests for clarification, ambiguous utterances and repetition of information [17]. An example of topic analysis is provided in the Appendix.
The following conversational and topic patterns were determined for each conversation: (1) the number of topics/ sub-topics introduced; (2) the proportion of topics/sub-topics introduced by participants with TBI; (3) the number of utterances produced; and (4) the proportion of utterances produced by participants with TBI. Including these statistically descriptive measures within qualitative studies supports findings and provides a numerical description of the object of study [50]. Coelho et al. [18] also note the importance of considering initiation of content when analysing conversational discourse abilities following TBI.
Rigour
Transcription reliability [34] was determined for 50% of transcripts completed by the SLP research student. The first author transcribed the data from audio/video recordings. Point-to-point agreement was calculated at 90.1%, based on a word-by-word basis.
Categories and themes were continually reviewed alongside original transcripts to enhance credibility, achieve coding consistency and ensure themes were represented across the data [51–53]. Initial codes assigned to meaning units were peer reviewed [51] for 20% of the data by the independent SLP research student. Disagreements were discussed and agreement was reached by consensus. Categories and themes were developed through author consensus [45]. The first author also maintained an audit trail of coding and decision-making [45,54].
Member checking was not logistically possible, as some participants had cognitive-communication difficulties. Additionally, as this study is part of a longitudinal study, providing feedback may have affected the veracity of findings obtained at subsequent data collection points. However, findings were presented to expert SLPs practicing in TBI to determine whether themes resonated with their experiences of conversations with people with severe TBI. The authors also adhered to guidelines for reporting qualitative research [48].
Dependability was enhanced by ensuring descriptive validity for topic analysis [34,50]. A trained SLP research student analysed 20% of the data using topic analysis. Point-to-point agreement with the first author’s original coding equalled 93.2%. Any disagreements were discussed and coded by consensus. The first author re-completed topic analysis ~ 3 weeks after the final transcript was analysed. Point-to-point agreement with the original coding equalled 93.4% for 20% of randomly selected transcripts.
Researchers
At the time of the study the first author was an undergraduate SLP student with theoretical knowledge of TBI and clinical experience with adults with acquired communication disorders, but not specifically TBI. The remaining authors were SLPs or psychologists forming part of a research team with expertise in communication disorders following TBI. In keeping with qualitative approaches, the authors remained attentive to the potential influence of professional experience upon interpretation and reporting. Methodological rigour was applied to ensure that findings reflected participant’s voices, rather than researcher bias or opinion based on perceived conversational issues or previous experience working with people with TBI.
Ethics
This research project was approved by the Human Research Ethics Committee of the University of Sydney and participating health service sites.
Results
Twenty-two participants with severe TBI engaged in a casual conversation with a chosen communication partner at 3 and 6 months post-injury. Conversations ranged from 7–10 minutes in length. Four conversations were less than 10 minutes due to interruptions from family members or disruption to the recording. These four conversations were included in the data set as 5-minute samples are considered representative for conversational analysis [42].
Nature of conversational topics at 3 months post-injury
The nature of topics discussed at 3 months post-injury focused on participants’ life in rehabilitation, impacts of injury and early recovery. Five main themes were identified along with categories underpinning each theme, as presented in Table II. Pseudonyms were used to protect participants’ identity.
Table II.
Themes and categories formed from topics introduced during conversation at 3 months post-injury.
| Theme | n | Categories |
|---|---|---|
|
| ||
| Connecting outside rehabilitation | 20 | Focus on people outside of rehabilitation Planning/discussing activities outside rehabilitation |
| Different ways of caring | 19 | Concern from COP Completing tasks for PAR Support and concern from friends Impact of caring on COP |
| What is happening in rehabilitation? | 19 | Therapy Visitors Medical appointments/meetings Daily activities Managing weekend/day leave Other patients |
| Early impacts and signs of recovery | 19 | Physical impacts Non-physical impacts Signs of recovery |
| Planning for re-engaging | 12 | Discharge from rehabilitation Plans after rehabilitation |
n, number of conversations in which the theme was present; COP, communication partner; PAR, participant with TBI.
Theme 1: Connecting outside of rehabilitation
Conversations at 3 months post-injury connected participants with TBI with what was happening outside BIRUs. Categories within this theme focused on connecting with people and planning activities outside rehabilitation settings.
Focus on people outside of rehabilitation.
‘Connecting’ topics focused upon what was happening in the lives of participants’ family and friends. These topics were typically introduced by communication partners. For example, James’ mother Debbie described her visit to the local hairdresser:
Debbie (COP): Um, I popped into Jane’s today.
James (PAR): Oh yeah.
Debbie (COP): Yes, and I wrote a little card to say thank you for cutting your hair.
Planning and discussing activities outside of rehabilitation.
‘Connecting’ topics also included activities that participants with TBI were planning during leave from rehabilitation settings. Many conversations focused upon organisational aspects of activities, including times and locations:
Mei (COP): Brad can bring you to go to Centennial Park next week on Sunday.
When participants with TBI introduced ‘connecting’ topics they requested information about upcoming plans. For example, Peter asked his wife about their night at the local club, while Sharon and her daughter discussed their forthcoming trip to an art gallery.
Theme 2: Different ways of caring
Conversations at 3 months post-injury reflected different ways of caring for participants with TBI. This theme was driven by communication partners and highlighted various ways people may support individuals with TBI during sub-acute recovery.
Concern from communication partner.
‘Caring’ topics were introduced when communication partners sought to ensure participants with TBI were being well cared for in rehabilitation units. For example, communication partners confirmed whether participants had received their medication (Susan, Jenny) or asked if they were in pain (Cheryl, Joanne, Lisa, Susan).
Completing tasks for participants with TBI.
Communication partners also introduced ‘caring’ topics when they reported completing tasks or responsibilities for participants with TBI (e.g. washing, bringing food) or asked whether they had any requests:
Jessica (COP): So is there anything you need … at the shops?
Support and concern from friends.
‘Caring’ topics also focused on care provided by friends. For example, James reflected upon his friend’s help with aphasia therapy tasks:
James (PAR): Every time I see Liam, or anyone who comes in to help me … I saw him help me of what they told him to do [sic].
Debbie (COP): I know, he really enjoys helping you and um, just watching you get better.
Impact of caring on close family members.
Some communication partners provided an insight into how caring for participants with TBI affected their daily lives. Nicole mentioned her new role as a ‘carer’, while Carol reported less time for herself since she was ‘either working or coming here to see [Chris]’.
Theme 3: What is happening in rehabilitation?
Life in rehabilitation was a major focus of conversations at 3 months post-injury. In contrast to theme one where topics connected participants with TBI to life outside BIRUs, this theme explored activities within rehabilitation settings. Topics provided communication partners with an insight into rehabilitation processes and procedures.
Therapy, visitors and medical appointments.
Topics focused on the nature and scheduling of therapy (e.g. physiotherapy, SLP), visitors and medical appointments. For example, Michael spoke about his physiotherapy session:
Michael (PAR): The physio worked me hard this morning … I did push ups … 10 minutes on the bike
Communication partners often introduced topics related to visiting hours. Lisa informed Tony about his afternoon visitor:
Lisa (COP): So Sam’s coming today at four.
Tony (PAR): Oh, good. Is Darren coming?
Lisa (COP): No, Darren’s not coming …
Additional ‘rehabilitation’ topics focused on ward activities (e.g. cooking, watching television), plans for weekend/ day leave and other patients within rehabilitation units.
Theme 4: Early impacts and signs of recovery
Topics concerning the early impacts of TBI and signs of recovery frequently occurred at 3 months post-injury.
Physical impacts.
Participants and communication partners identified physical impairments (e.g. reduced mobility, pain and burns), discussed ways to reduce disability (e.g. pain relief) or barriers to participation. John, whose mobility had been affected by his injury, declined a weekend outing:
Jessica (COP): You gonna come out … Or you gonna give it a miss?
John (PAR): I wouldn’t mind … but walking around in the city all day would take its toll.
Non-physical impacts.
Memory impairments were the most frequently discussed non-physical impact of TBI, as Greg explained:
Greg (PAR): As far as multi-tasking goes I tend to start one thing and then flip around to another … but then I forget what I’ve done … when I’m cooking it’s pretty disastrous.
Participants also identified communication impairments as a barrier to sharing information and feelings during sub-acute recovery. For Emily, aged 16 years, dysarthria affected her ability to express concerns with her mother:
Emily (PAR): I couldn’t tell you because I couldn’t talk … It was hard.
Other non-physical impacts included anger related to the cause of injury (Chris) and feeling mentally ‘restricted’ (Paul).
Signs of recovery.
Some participants with TBI actively identified signs of recovery at 3 months post-injury, while others reported perceived improvements in both physical and non-physical impacts of TBI. For example, Carol reassured her son Chris that his burns were healing:
Carol (COP): The burns … You know where it’s pale … That’s where it’s getting a bit better.
Communication partners also acknowledged signs of recovery. For example, James’ mother Debbie noted his communication had improved:
James (PAR): Every time, I keep getting better with what I say.
Debbie (COP): You are, every time. And every time I see you it’s quite exciting … I think ‘I wonder … what new words James is going to have …’
Theme 5: Planning for re-engaging
At 3 months post-injury, many conversations reflected a drive towards re-engaging and returning to life pre-injury.
Discharge from rehabilitation.
Discharge from rehabilitation was perceived as a major step to re-engaging in pre-injury activities. Some participants discussed discharge plans. For example, Ben’s father requested details about his discharge date, while Scott’s mother asked if he had ‘sorted accommodation’. Others indicated they looked forward to leaving BIRUs or hoped for an earlier discharge date. Scott, for example, expressed frustration with the constraints of being in rehabilitation:
Scott (PAR): I just hope I can be released soon because I’m getting a little bit stir crazy here.
Plans after rehabilitation.
‘Re-engaging’ topics included planning beyond discharge from rehabilitation. For example, Tony and his wife discussed plans for returning to work:
Tony (PAR): I haven’t spoken to Jim about what the plan is to go back to work, but I don’t know what it is, do you?
Lisa (COP): No … there’s no rush.
Nature of conversational topics at 6 months post-injury
The nature of topics introduced at 6 months post-injury remained focused on what was happening in the lives of participants with TBI. However, topics about communication partners, family and friends were discussed to a greater extent than at 3 months post-injury. Topics about the impacts of TBI were discussed less frequently. Three themes emerged from content analysis, as presented in Table III.
Table III.
Themes and categories formed from topics introduced during conversation at 6 months post-injury.
| Theme | n | Categories |
|---|---|---|
|
| ||
| Day-to-day life and re-engaging | 21 | Day-to-day and social plans Plans for re-engaging Barriers to re-engaging |
| Focusing on others | 19 | COP Family members Friends |
| Impacts are individual and changing | 13 | Physical/non-physical impacts of injury Therapy/injury-related appointments/plans Caring about impacts of injury Signs of recovery |
n, number of conversations in which the theme was present; COP, communication partner.
Theme 1: Day-to-day life and re-engaging
Planning and re-engaging in day-to-day life was a major theme present in conversations at 6 months post-injury. Related topics provided an insight into the lives of participants with TBI and their progress towards returning to life pre-injury.
Day-to-day and social plans.
All participants had been discharged from their respective BIRUs at 6 months post-injury. Many topics focused on daily and social plans. Communication partners were interested in the social activities of participants with TBI:
Lisa (COP): Alright, so on Monday you’re gonna see Alex again?
Tony (PAR): Yep … We’re gonna go to North Sydney oval and work out.
Other conversations included topics about forthcoming family plans. For example, John and his daughter Jessica discussed an upcoming birthday party:
John (PAR): Next weekend, Jasmine’s party hey?
Jessica (COP): Yeah, go to mum’s place and hopefully find out who rocks up there.
Plans for re-engaging.
‘Re-engaging’ topics included goals for resuming pre-morbid activities such as work, study or driving. James (21 years) planned to return to university:
James (PAR): I don’t need to do a whole year, I need to do half the year … Can’t wait to go back.
Theme 2: Focusing on others
Discussion about communication partners, other family members and friends occurred more frequently at 6 months post-injury compared with 3 months post-injury. Both participants with TBI and their communication partners asked questions or provided information about others’ work, holidays, health and social plans. For example, Scott asked his mother about her impending leave from work:
Scott (PAR): So when did you actually put in for your holidays? What day?
Cheryl (COP): Well it’s sort of changeable. Mid-December to mid-January.
Emily, a participant with TBI, introduced a topic about her brother:
Emily (PAR): Is Matt gonna be here or?
Tracey (COP): No Matt’s going back to uni so he’ll …
Emily (PAR): When will he be going?
Tracey (COP): Well I don’t know, probably Tuesday or Wednesday.
Theme 3: Impacts are individual and changing
Impacts of TBI still persisted for many participants at 6 months post-injury. These impacts were more individualised compared with those discussed at 3 months post-injury. Topics directed towards concern and support from communication partners occurred less frequently than at 3 months post-injury.
Physical/non-physical impacts of injury.
In contrast to conversations at 3 months post-injury, communication and physical impacts were discussed to a lesser extent at 6 months post-injury. Daniel was the only participant who introduced a topic about communication changes following his injury. He had acquired a voice disorder and explained, ‘I just want my old voice back’. Additional non-physical impacts reported by participants included memory impairments, fatigue and anxiety. Some participants mentioned they had difficulty managing these continuing impacts, including Tony:
Tony (PAR): The psychologist … she was the one I was telling I was a bit, bit scared about things and she was telling me, ‘Tony, it’s normal to be scared …’
Therapy/injury related appointments or plans.
Topics about continuing impacts of TBI reflected participants’ long-term commitment to rehabilitation. Some participants still attended therapy and medical appointments at 6 months post-injury. Topics within this category usually involved scheduling therapy sessions or appointments (e.g. physiotherapy, psychology, specialists):
Li (PAR): I will have assessment today again with Kerry right?
Mei (COP): Yep. For the physio.
Signs of recovery.
Topics were less focused on signs of recovery at 6 months post-injury compared with 3 months post-injury. However, some participants indicated positive feelings about recovery. Tony was happy he had ‘some memory at last’ when recalling the name of a therapist. Communication partners also introduced topics related to recovery. For example, Luke’s mother commented on his wound healing:
Anne (COP): That’s coming up really well isn’t it now. you know, the hair is growing over it.
Themes present in conversations have provided an insight into what some individuals with severe TBI may experience day-to-day during sub-acute recovery. Topics reflected the early impacts of TBI, rehabilitation processes and steps individuals may take to re-engage in pre-injury life.
Conversational and topic patterns
Topic analysis [17] was used to investigate patterns in topic introduction between participants with TBI and familiar communication partners. Descriptive statistics for topic analysis are presented in Table IV. In keeping with qualitative descriptive approaches, the data is intended to describe patterns of conversational and topic contributions.
Table IV.
Descriptive statistics for topic analysis.
| Measure | 3 months Mean; SD (range) | 6 months Mean; SD (range) | Mean change |
|---|---|---|---|
|
| |||
| Topics per conversation | 17.0; 8.29 (7–42) | 15.0; 7.68 (2–36) | −2 |
| Topics introduced by PAR (%) | 39.4; 23.77 (8.3–88.1) | 45.9; 25.11 (0–80.0) | +6.5 |
| Sub-topics per conversation | 44.0; 9.28 (27–61) | 46.0; 10.16 (27–60) | +2 |
| Sub-topics introduced by PAR (%) | 40.7; 19.42 (4.9–86.2) | 41.4; 17.68 (6.5–71.4) | +0.7 |
| Utterances per conversation | 275.0; 53.12 (179–396) | 257.0; 68.40 (129–401) | −18 |
| Utterances produced by PAR (%) | 45.2; 9.93 (29.9–69.0) | 45.3; 11.72 (12.4–68.2) | +0.1 |
PAR, participant with TBI.
A mean of 17 topics and 44 sub-topics were introduced in each conversation at 3 months post-injury. Participants with TBI introduced ~ 10% less topics and sub-topics than their communication partners. Most introduced topics were new or related, with only 9.9% of all topics classified as re-introduced. Conversations varied in utterance length and participants with TBI produced an average of 45% of utterances in each conversation.
No marked differences were observed in patterns of topic introduction and participants’ contributions to conversations at 6 months post-injury compared with 3 months post-injury. A mean of 15 topics and 46 sub-topics were introduced in each conversation at 6 months post-injury. Participants with TBI introduced fewer topics than their communication partners; however, the proportion was closer to 50%. Similar to 3 months post-injury, most topics were new or related to previously introduced topics and 10.9% were re-introduced. The number of utterances produced per conversation varied greatly between dyads. Participants with TBI continued to produce a mean of 45% of utterances per conversation.
Discussion
Sustaining a severe TBI is a sudden, life-changing event that significantly impacts on an individual’s life, as evident in topics discussed during conversations in sub-acute recovery. In this study, the nature of conversational topics changed subtly from 3 to 6 months post-injury, whereas conversational and topic patterns remained relatively stable.
Nature of conversational topics
Previous studies propose that conversations of people with TBI are often less rewarding and interesting than those of people without TBI, as people with TBI may adopt an egocentric approach and neglect communication partners’ interests [8,13]. However, the findings suggest that people with severe TBI and their family members discuss mutually interesting topics consistent with those discussed by people without TBI [19,21–23]. Another positive finding was a thread of optimism within topics, as participants and communication partners discussed signs of recovery and re-engaging in pre-injury life. Surprisingly, topics of an inappropriate nature were not identified, as reported in earlier studies [24,55]. This finding may be attributed to the sample of TBI participants or the role of communication partners in selecting topics that facilitate people with TBI’s participation, potentially masking issues that may occur in less supportive conversational environments.
Three main themes were central to conversations at 3 and 6 months post-injury: (1) connecting; (2) re-engaging; and (3) impacts of injury, as presented in Figure 1. Topics within these themes changed over time to reflect the recovery process. At 3 months post-injury, topics focused on aspects of recovery such as injury sequelae and rehabilitation procedures. While setting is one aspect of recovery that may have influenced conversational content, participants discussed these topics regardless of whether they were inpatients or had returned home. However, these topics may have been of greater prominence during conversations of inpatients.
Figure 1.
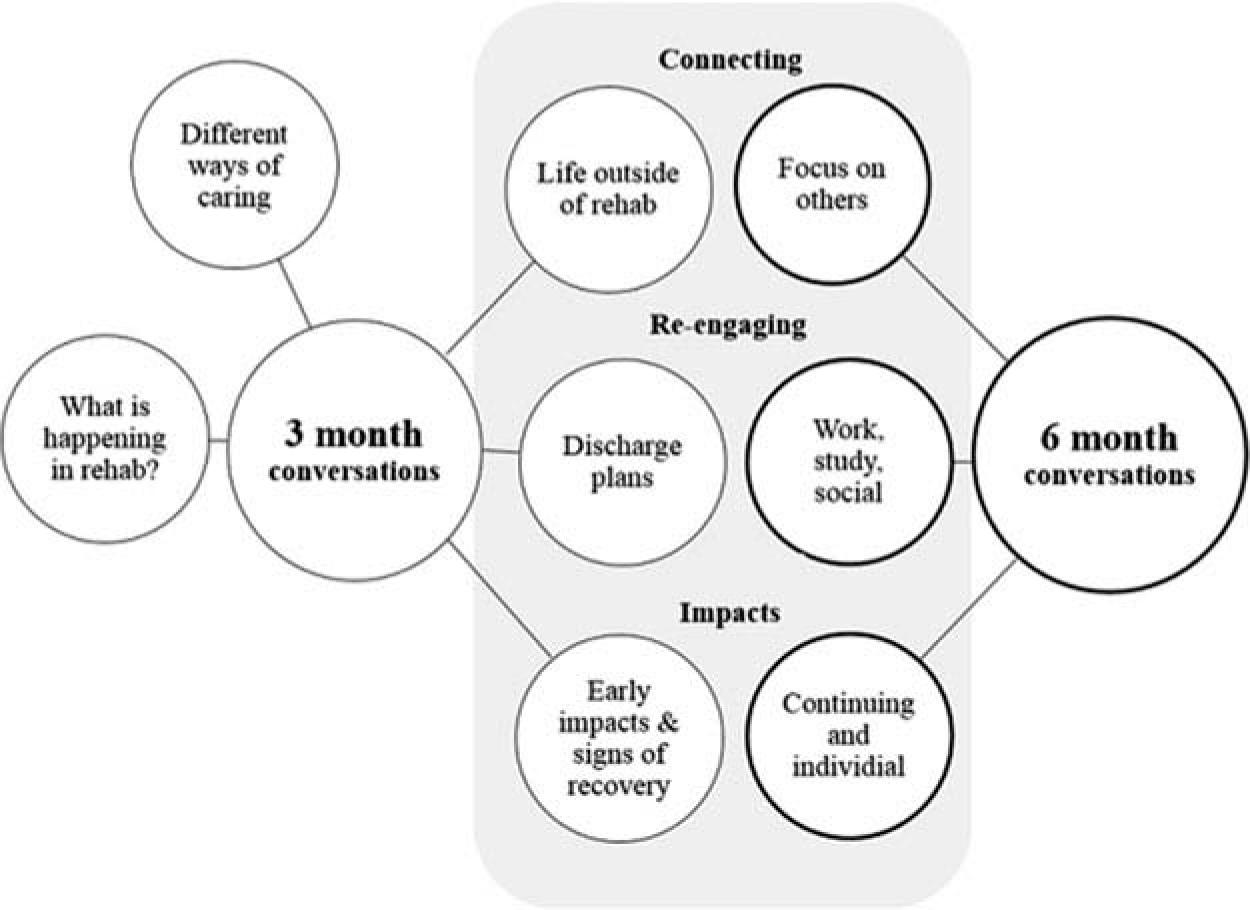
Themes derived from conversations at 3 and 6 months post-injury.
At 3 months post-injury, communication partners introduced topics that connected participants to life outside BIRUs. Participants with TBI introduced fewer topics within this theme, suggesting that family members have an important role in assisting people with TBI to connect with others and engage in non-rehabilitation activities. ‘Re-engaging’ topics revealed that leaving BIRUs was perceived as the first step towards resuming pre-injury life. Early impacts of TBI reported at 3 months post-injury included pain, reduced mobility and memory impairments, all of which frequently occur following severe TBI [56,57]. Participants also discussed the impact of communication impairments (e.g. aphasia, dysarthria), confirming the importance of addressing communication goals in sub-acute rehabilitation.
Topics discussed at 6 months post-injury reflected later recovery processes, whereby people with TBI have likely overcome major physical impairments and are focused on re-engaging with people and community activities. The nature of topics changed for participants who were outpatients at both 3 and 6 months post-injury, again indicating that setting is only one aspect of the recovery process.
In comparison to 3 month conversations, ‘connecting’ topics discussed at 6 months post-injury focused on communication partners, other family members and friends. Participants with TBI introduced more ‘connecting’ topics compared with 3 months post-injury, reflecting a less egocentric focus during conversations. Plans to re-engage were expressed in aspirations to return to social, vocational or educational activities, as participants with TBI had returned home. Physical impacts were rarely discussed at 6 months post-injury, consistent with previous research that suggests physical impairments often improve within 6 months, whereas non-physical impacts continue long-term [7,9,58,59]. Reports of various cognitive and psychosocial impacts confirmed that individuals with TBI have their own unique recovery experience [6].
Figure 1 illustrates that the themes ‘what is happening in rehabilitation?’ and ‘different ways of caring’ did not feature in conversations at 6 months post-injury. Several factors may have led to changing themes. At 3 months post-injury, communication partners acquired or provided information about rehabilitation programmes, demonstrating the importance of regular communication between family members and health professionals involved in the care of people with TBI. Some participants reported continuing rehabilitation involvement, yet programmes were not all-encompassing, as participants had returned home. Family members have an important role in caring for people with TBI in early sub-acute recovery. Topics introduced by communication partners revealed practical and psychosocial aspects of caring for participants at 3 months post-injury. The reduced occurrence of ‘caring’ topics at 6 months post-injury may indicate participants had regained independence with activities of daily living or reflect disconnection between family members and people with TBI with regards to care needs and burdens.
Conversational and topic patterns
Examining conversational patterns during sub-acute recovery provided an opportunity to identify improvements or developing maladaptive behaviours. However, group conversational and topic patterns remained similar at 3 and 6 months post-injury. Several factors may have influenced this finding. There appears to be less overt social communication deficits in this sample than typically reported in TBI literature. This may be attributed to the selection of participants via an inception cohort vs selecting on the basis of social or cognitive-communication disorders, which is common in many TBI studies. Although this study included participants with aphasia and dysarthria, communication partners’ perceptions placed most participants’ social communication abilities within a range typical for adults without TBI. Thus, there may have been less opportunity to observe changes or improvements.
The mean number of topics introduced per conversation remained stable over time, particularly within each dyad. Participants with TBI introduced an average of 45% of topics at both 3 and 6 months post-injury, suggesting that as a group they did not rely on communication partners to introduce topics, inconsistent with previous findings [3,17,20]. Overall, participants with severe TBI demonstrated similar patterns of topic introduction to those reported for people without TBI [17,20].
Another unexpected finding was that mean contributions to conversations were relatively balanced within individual dyads, as previous studies report that some people with TBI introduce shorter, but more frequent utterances [18,60]. However, communication partners in these earlier studies included investigators who were unknown to participants with TBI. The findings suggest that people with TBI can engage in balanced conversations with close family members, potentially reflecting the benefit of selecting communication partners where issues of unfamiliarity or power dynamics may not impact interactions.
However, group findings should be interpreted with caution as there was a large range in the proportion of topics and utterances introduced by individuals. Participants who introduced a greater proportion of topics also produced a greater proportion of utterances, as did participants at the lower end of ranges for each measure. Conversation measures were potentially sensitive to communication impairments, which could explain this variation. For example, dysarthria or low perceived social communication abilities may have contributed to participants producing a lower proportion of topics and utterances.
Limitations
This is the first qualitative study to investigate the nature and patterns of conversational topics discussed by people with severe TBI and familiar communication partners during sub-acute recovery. This study, however, is not without limitations. First, despite attempts to ensure the setting and nature of the task were as natural as possible, the presence of recording devices may have limited the discussion of sensitive or inappropriate topics. Second, participants were a self-selecting group who agreed to have their conversations recorded. Participants in the longitudinal study who declined recorded conversations may have experienced communication impairments or complex relationship issues that impacted their conversational behaviours.
Clinical implications
Findings from this study have important implications for SLPs involved in TBI rehabilitation. Content analysis identified a range of naturally occurring topics for discourse therapy and suggests that casual conversations provide a way for people with TBI to discuss issues pertinent to their injury, recovery and return to pre-morbid activities. Therefore, SLPs may consider focusing on conversational interventions to assist with navigating the recovery process. Additionally, words or phrases relevant to identified topics could be included when targeting intelligibility or word finding difficulties in individuals with dysarthria and aphasia, respectively.
These findings also support conversations as a tool to identify people with TBI who would benefit from support to increase topic introduction or engage in more balanced interactions. Identified topics may also provide extra conversational content for people with TBI who demonstrate impoverished conversations. Additionally, communication partners who may benefit from communication partner training could be identified by examining patterns of their topic introductions and responses. As most individual dyads demonstrated minimal spontaneous change in conversational and topics patterns between 3 and 6 months post-injury, any difficulties should be addressed in early recovery to prevent them from persisting long-term. Furthermore, variation between dyads’ conversational and topic patterns reflect the heterogeneity of conversations of people with TBI and the need for individually tailored intervention.
Multidisciplinary involvement is also recommended when implementing conversational interventions. Memory difficulties were frequently discussed, as were details about rehabilitation programmes. Memory support aids could be utilised during therapy with other professionals. For example, inpatients may benefit from taking notes about activities they participate in, which would support them when recounting their days in rehabilitation to communication partners.
Overall, topics comprised requesting or providing information. Few topics addressed sensitive issues or the psychosocial impacts of caring for individuals with TBI, perhaps indicating that topics of this nature may not be easy to discuss in sub-acute recovery. Accordingly, SLPs may consider additional multidisciplinary input during intervention.
Research implications
This study has important implications for future research. The minimum change in patterns of topic and utterance introduction by participants with TBI indicates that casual conversations could be a stable measure to investigate conversational discourse abilities of people with severe TBI over time and with the same communication partner. Content and topic analysis may provide additional information to complement standardised SLP assessments and offer insights into why the conversations of some individuals with TBI are perceived as unrewarding.
Conversational themes were derived from comparative analysis and reflect topics that occurred across the participant group. However, demographic variables may have influenced some of the content discussed within individual dyads, as the participants were from diverse demographic backgrounds (e.g. education, presence of communication impairment, gender, age, neuropathology, relationship between dyads). The influence of these variables on the nature of conversational topics could be addressed in future research. Additional themes and changes in topic patterns may also occur during conversations in later recovery. The findings may reflect a ‘honeymoon’ stage, whereby individuals with TBI have overcome life-threatening consequences of their injury and long-term psychosocial sequelae have not impacted their conversations. Further investigations may reveal additional clinical implications and, thus, could better support the timing and focus of SLP intervention to enhance the conversations of people with TBI.
Conclusion
Qualitative content analysis provides a meaningful insight into the nature of topics people with TBI may discuss in conversations with close family members during sub-acute recovery. Findings may inform clinical practice for SLPs and other health professionals involved in the early rehabilitation of people with severe TBI.
Acknowledgements
We thank all participants, their communication partners and participating health sites for their commitment to this study. We also thank An An Chia for assistance with transcription and completion of measures to enhance rigour.
Appendix: Example of topic analysis [17] from transcript of TBI participant, Michael, and his wife, Therese
| Speaker | Utterance | T/S/M |
|---|---|---|
|
| ||
| Michael | So you got a lot on for work? | T |
| Therese | Yeah. | M |
| Michael | It’s a bit boring isn’t it? | S |
| Therese | Yeah. | M |
| Michael | When’s, uh, you all prepped for the audit though? | S |
| Therese | No. | M |
| Michael | No? | M |
| Michael | Okay. | M |
T, topic; S, sub-topic; M, maintaining utterance.
Communication profile of participants with TBI
| PARa | Aphasia | Dysarthria | LCQ total |
|---|---|---|---|
|
| |||
| Andrew | Yes | Yes | 38 |
| Tony | Yes | Yes | 55 |
| Emily | No | Yes | 46 |
| Peter | No | Yes | 42 |
| Li | Yes | Yes | 56 |
| Steven | Yes | Yes | 34 |
| Mark | No | Yes | 41 |
| Amanthi | Yes | Yes | 77b |
| Chris | Yes | Yes | DNC |
| Sharon | Yes | Yes | 59b |
| Ben | Yes | Yes | 43 |
| Scott | No | No | 56 |
| John | UTC | Yes | 31 |
| Josh | Yes | Yes | 40 |
| Paul | No | Yes | 65b |
| Jack | Yes | Yes | 41 |
| James | Yes | Yes | 73b |
| Daniel | Yes | Yes | 80b |
| Luke | Yes | Yes | 62 |
| Greg | No | No | 104b |
| Michael | No | Yes | 58b |
| Shane | No | Yes | 45 |
PAR = participant with TBI
pseudonyms were used to protect participants’ identity; LCQ = La Trobe Communication Questionnaire
score > 1 SD of mean for normal population; DNC = did not complete; UTC = unable to complete.
Characteristics of communication partners
| PAR | COPa | Relationship to PAR | Age (years) | Length of relationship (years) |
|---|---|---|---|---|
|
| ||||
| Andrew | Kylie | Wife | 40 | 15 |
| Tony | Lisa | Wife | 44 | 18 |
| Emily | Tracey | Mother | 46 | 16 |
| Peter | Louise | Wife | 38 | 20 |
| Li | Mei | Sister | 27 | 27 |
| Steven | Joanne | Wife | 49 | 22 |
| Mark | Susan | Wife | 53 | 36 |
| Amanthi | Saman | Husband | 39 | 12 |
| Chris | Carol | Mother | 65 | 43 |
| Sharon | Michelle | Daughter | 39 | 39 |
| Ben | George | Father | 60 | 28 |
| Scott | Cheryl | Mother | 66 | 40 |
| John | Jessica | Daughter | 21 | 21 |
| Josh | Nicole | Mother | 42 | 19 |
| Paul | Kim | Mother | 56 | 32 |
| Jack | Karen | Mother | 49 | 17 |
| James | Debbie | Mother | 45 | 21 |
| Daniel | Jenny | Mother | 43 | 23 |
| Luke | Anne | Mother | 43 | 18 |
| Greg | Mary | Wife | 59 | 16 |
| Michael | Therese | Wife | 39 | 20 |
| Shane | Julie | Wife | 42 | 21 |
PAR = participant with TBI; COP = communication partner
pseudonyms were used to protect the identity of communication partners.
Footnotes
Declaration of interest
The authors alone are responsible for the writing of this paper. The data collected will form part of a longitudinal project investigating communication recovery following TBI that is funded by the National Health and Medical Research Council (NHMRC). The relationship between the research team and funding provider constitutes no conflicts of interest.
References
- 1.Ventola E. The structure of casual conversation in English. Journal of Pragmatics 1979;3:267–298. [Google Scholar]
- 2.Eggins S, Slade D. Analysing casual conversation. New York: Cassell; 1997. [Google Scholar]
- 3.Coelho CA, Youse K, Le K. Conversational discourse in closed-head-injured and non-brain-injured adults. Aphasiology 2002;16:659–672. [Google Scholar]
- 4.Shorland J, Douglas JM. Understanding the role of communication in maintaining and forming friendships following traumatic brain injury. Brain Injury 2010;24:569–580. [DOI] [PubMed] [Google Scholar]
- 5.Galski T, Tompkins C, Johnston MV. Competence in discourse as a measure of social integration and quality of life in persons with traumatic brain injury. Brain Injury 1998;12:769–782. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain DJ. The experience of surviving traumatic brain injury. Journal of Advanced Nursing 2006;54:407–417. [DOI] [PubMed] [Google Scholar]
- 7.Ponsford J. Understanding and managing traumatic brain injury. InPsych 2012;34. Available from http://www.psychology.org.au/publications/inpsych/2012/april/ponsford/.
- 8.Snow P, Douglas JM, Ponsford J. Conversational discourse abilities following severe traumatic brain injury: a follow up study. Brain Injury 1998;12:911–935. [DOI] [PubMed] [Google Scholar]
- 9.Konrad C, Geburek AJ, Rist F, Blumenroth H, Fischer B, Husstedt I, Arolt V, Schiffbauer H, Lohmann H. Long-term cognitive and emotional consequences of mild traumatic brain injury. Psychological Medicine 2011;41:1197–1211. [DOI] [PubMed] [Google Scholar]
- 10.Ismail S. Medical complications, physical function and communication skills in patients with traumatic brain injury: a single centre 5-year experience. Brain Injury 2008;22:733–739. [DOI] [PubMed] [Google Scholar]
- 11.Mazaux JM. Rehabilitation after traumatic brain injury in adults. Disability & Rehabilitation 1998;20:435–447. [DOI] [PubMed] [Google Scholar]
- 12.Turner-Stokes L, Disler PB, Nair A, Wade DT. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. The Cochrane Database Of Systematic Reviews 2005;3: CD004170. [DOI] [PubMed] [Google Scholar]
- 13.Bond F, Godfrey HPD. Conversation with traumatically brain injured individuals: a controlled study of behavioural changes and their impact. Brain Injury 1997;11:319–329. [DOI] [PubMed] [Google Scholar]
- 14.Mozeiko J, Lé K, Coelho CA. The handbook of language and speech disorders. Malden (MA): Wiley-Blackwell; 2010. [Google Scholar]
- 15.Snow P, Douglas JM, Ponsford J. Procedural discourse following traumatic brain injury. Aphasiology 1997;11:947–967. [Google Scholar]
- 16.Coelho CA, Youse K, Le K, Feinn R. Narrative and conversational discourse of adults with closed head injuries and non-brain-injured adults: a discriminant analysis. Aphasiology 2003;17:499–510. [Google Scholar]
- 17.Mentis M, Prutting CA. Analysis of topic as illustrated in a head-injured and a normal adult. Journal of Speech and Hearing Research 1991;34:583–595. [DOI] [PubMed] [Google Scholar]
- 18.Coelho C, Ylvisaker M, Turkstra LS. Nonstandardized assessment approaches for individuals with traumatic brain injuries. Seminars in Speech and Language 2005;26:223–241. [DOI] [PubMed] [Google Scholar]
- 19.Friedland D, Miller N. Conversation analysis of communication breakdown after closed head injury. Brain Injury 1998;12:1–14. [DOI] [PubMed] [Google Scholar]
- 20.Coelho CA, Liles BZ, Duffy RJ, Clarkson JV. Conversational patterns of aphasic, closed-head-injured, and normal speakers. Clinical Aphasiology 1993;21:183–192. [Google Scholar]
- 21.Haas A, Sherman M. Conversational topic as a function of role and gender. Psychological Reports 1982;51:453–454. [Google Scholar]
- 22.Aries EJ, Johnson FL. Close friendship in adulthood: conversational content between same-sex friends. Sex Roles 1983;9:1183–1196. [Google Scholar]
- 23.Sehulster J. Things we talk about, how frequently, and to whom: frequency of topics in everyday conversation as a function of gender, age, and marital status. The American Journal of Psychology 2006;119:407–432. [PubMed] [Google Scholar]
- 24.Body R, Parker M. Topic repetitiveness after traumatic brain injury: an emergent, jointly managed behaviour. Clinical Linguistics & Phonetics 2005;19:379–392. [DOI] [PubMed] [Google Scholar]
- 25.Togher L, Hand L, Code C. A new perspective on the relationship between communication impairment and disempowerment following head injury in information exchanges. Disability & Rehabilitation 1996;18:559–566. [DOI] [PubMed] [Google Scholar]
- 26.Togher L, Taylor C, Aird V, Grant S. The impact of varied speaker role and communication partner on the communicative interactions of a person with traumatic brain injury: a single case study using systemic functional linguistics. Brain Impairment 2006;7:190–201. [Google Scholar]
- 27.Tu LV, Togher L, Power E. The impact of communication partner and discourse task on a person with traumatic brain injury: the use of multiple perspectives. Brain Injury 2011;25:560–580. [DOI] [PubMed] [Google Scholar]
- 28.Togher L, Hand L, Code C. Analysing discourse in the traumatic brain injury population: telephone interactions with different communication partners. Brain Injury 1997;11:169–189. [DOI] [PubMed] [Google Scholar]
- 29.Behn N, Togher L, Power E, Heard R. Evaluating communication training for paid carers of people with traumatic brain injury. Brain Injury 2012;26:1702–1715. [DOI] [PubMed] [Google Scholar]
- 30.Togher L, McDonald S, Code C, Grant S. Training communication partners of people with traumatic brain injury: a randomised controlled trial. Aphasiology 2004;18:313–335. [Google Scholar]
- 31.Togher L, McDonald S, Tate R, Power E, Rietdijk R. Training communication partners of people with severe traumatic brain injury improves everyday conversations: a multicenter single blind clinical trial. Journal of Rehabilitation Medicine 2013;45:637–645. [DOI] [PubMed] [Google Scholar]
- 32.Togher L, Tate R, McDonald S, Turkstra L, Holland A, MacWhinney M. Longitudinal communication outcomes following traumatic brain injury 2010–2014.
- 33.Denzin NK, Lincoln YS. Handbook of qualitative research. Thousand Oaks (CA): Sage Publications; 2000. [Google Scholar]
- 34.Sandelowski M. Whatever happened to qualitative description? Research in Nursing and Health 2000;23:334–340. [DOI] [PubMed] [Google Scholar]
- 35.Myburgh JA, Cooper DJ, Finfer SR, Venkatesh B, Jones D, Higgins A, Bishop N, Higlett T. Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. The Journal of Trauma 2008;64:854–862. [DOI] [PubMed] [Google Scholar]
- 36.Helps YL, Henley G, Harrison JE. Hospital separations due to traumatic brain injury, Australia 2004–05. Injury research and statistics series number 45 (Cat no. INJCAT 116). Adelaide: Australian Institute of Health and Welfare (AIHW); 2008. [Google Scholar]
- 37.Russell WR, Smith A. Post-traumatic amnesia in closed head injury. Archives of Neurology 1961;5:4–17. [DOI] [PubMed] [Google Scholar]
- 38.Australian Bureau of Statistics. ANZSCO – Australian and New Zealand Standard Classification of Occupations, 2013, Version 1.2. [Internet]. 2013. [cited 2015 March]. Available from http://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/1220.0?OpenDocument.
- 39.Kertesz A. Western aphasia battery-revised. San Antonio (TX): Pearson; 2006. [Google Scholar]
- 40.Enderby P, Palmer R. Frenchay dysarthria assessment. 2nd ed. (FDA-2). Austin (TX): PRO-ED, Inc.; 2008. [Google Scholar]
- 41.Douglas JM, O’Flaherty CA, Snow PC. Measuring perception of communicative ability: the development and evaluation of the La Trobe communication questionnaire. Aphasiology 2000;14:251–268. [Google Scholar]
- 42.Boles L, Bombard T. Conversational discourse analysis: appropriate and useful sample sizes. Aphasiology 1998;12:547–560. [Google Scholar]
- 43.AphasiaBank. Chat Transcription Training Manual. [Internet]. [cited 2014 January]. Available from http://talkbank.org/APhasiaBank/manuals/training.pdf.
- 44.Saffran EM, Berndt RS, Schwartz MF. The quantitative analysis of agrammatic production: procedure and data. Brain and Language 1989;37:440–479. [DOI] [PubMed] [Google Scholar]
- 45.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today 2004;24:105–112. [DOI] [PubMed] [Google Scholar]
- 46.Elo S, Kyngäs H. The qualitative content analysis process. Journal of Advanced Nursing 2008;62:107–115. [DOI] [PubMed] [Google Scholar]
- 47.Sandelowski M. Theory unmasked: the uses and guises of theory in qualitative research. Research in Nursing & Health 1993; 16:213–218. [DOI] [PubMed] [Google Scholar]
- 48.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care 2007;19:349–357. [DOI] [PubMed] [Google Scholar]
- 49.Brinton B, Fujiki M. Development of topic manipulation skills in discourse. Journal of Speech and Hearing Research 1984; 27:350–358. [DOI] [PubMed] [Google Scholar]
- 50.Maxwell JA. Understanding and validity in qualitative research. Harvard Education Review 1992;62:279–300. [Google Scholar]
- 51.Milne J, Oberle K. Enhancing rigor in qualitative description: a case study. Journal of Wound, Ostomy, and Continence Nursing 2005;32:413–420. [DOI] [PubMed] [Google Scholar]
- 52.Weber RP. Basic content analysis. California: Sage Publications; 1990. [Google Scholar]
- 53.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks (CA): Sage Publications; 1994. [Google Scholar]
- 54.Carcary M. The research audit trial – enhancing trustworthiness in qualitative inquiry. Journal of Business Research Methods 2009;7:11–24. [Google Scholar]
- 55.Perkins MR, Body R, Parker M. Closed head injury: assessment and remediation of topic bias and repetitiveness. In: Perkins MR, Howard S, editors. Case studies in clinical linguistics. London: Whurr Publishers Ltd; 1995. [Google Scholar]
- 56.Vakil E. The effect of moderate to severe traumatic brain injury (TBI) on different aspects of memory: a selective review. Journal of Clinical and Experimental Neuropsychology 2005;27:977–1021. [DOI] [PubMed] [Google Scholar]
- 57.Gentleman D. Rehabilitation after traumatic brain injury. Trauma 2001;3:193–204. [Google Scholar]
- 58.Kersel DA, Marsh NV, Havill JH, Sleigh JW. Neuropsychological functioning during the year following severe traumatic brain injury. Brain Injury 2001;15:283–296. [DOI] [PubMed] [Google Scholar]
- 59.Dombovy ML, Olek AC. Recovery and rehabilitation following traumatic brain injury. Brain Injury 1997;11:305–318. [DOI] [PubMed] [Google Scholar]
- 60.Coelho CA. Management of discourse deficits following traumatic brain injury: progress, caveats, and needs. Seminars in Speech and Language 2007;28:122–135. [DOI] [PubMed] [Google Scholar]


