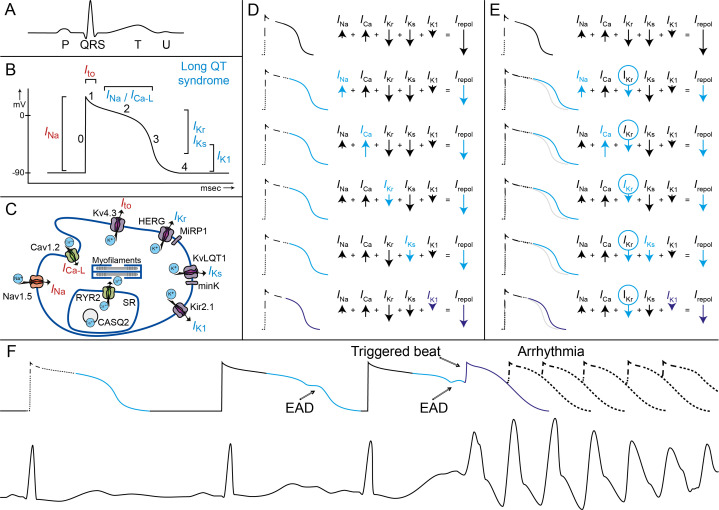
Figure 4.
Pathophysiological mechanisms underlying LQTS and associated arrhythmia. Figure parts A–C show the illustrations of (A) an ECG with a normal P-QRS-TU complex, (B) a corresponding ventricular action potential with the different cardiac ion currents (I) and (C) a cardiomyocyte with different ion channels, subunits and their currents. In long QT syndrome, the phase 2 late sodium inward current (I Na) the slow calcium inward current (I Ca-L), or the potassium rectifier currents during phase 3 and phase 4 (I Kr, I Ks, I K1) are involved. (D and E) In these illustrations, the action potential prolongation caused by a decrease in net repolarising current (I repol) by changes in one of the repolarising currents in blue is shown. (D) If any of the currents in repolarisation is altered (eg, by a LQT3 SCN5A mutation with more net I Na or a LQT1 KCNQ1 mutation with less net I Ks), the ventricular action potential (and the corresponding QT interval) will lengthen. (E) When a second hit on net repolarising current is introduced, for example, by (further) decrease of I Kr current due to the use of certain drugs, the ventricular action potentials and the QT interval will further lengthen. It can be appreciated that a loss of function of I K1 only has a minor effect on the action potential duration (purple). (F) In this illustration, the prolonged ventricular action potential durations correspond with prolonged QT intervals, which are further challenged by changes in heart rate and proceed to early after depolarisation (EAD). These EADs finally result in a triggered beat and the onset of malignant ventricular arrhythmia (Torsades de Pointes). LQTS, long QT syndrome.