Abstract
The global movement toward legalization of cannabis is resulting in an ever-increasing public perception that cannabis is safe. Cannabis is not the first drug to be available for nonmedical use, nor is it the first to have such an unfounded safety profile. The safety of long-term exposure to phytocannabinoids is misunderstood by, and under reported to, the general public. There is evidence to suggest that long-term use of recreational cannabis may be associated with an increased risk of undesirable side effects. This evidence warrants both appropriate caution from the general public and investment in further research by government and industry sectors that are profiting from the sale of these potent psychoactive agents. There is no doubt that these compounds have medical potential. However, in addition to the medical potential, we must also remain aware of the adverse health effects that are becoming synonymous with recreational cannabis use. This perspective highlights the privileged role that cannabis has as a perceived “safe drug” in society and summarizes some concerning side effects that are becoming associated with regular nonprescribed cannabis use.
Keywords: recreational cannabis use, nonmedical cannabis use, side effects, adverse health effects
Background
Cannabis is often considered to be one of the earliest plants used for medicinal purposes by humans.1 It is also arguably more infamous for its nonmedicinal use. As reported by the United Nations, cannabis is the most grown, transported, and sold controlled substance in the world.2 To tackle the sale of illegal cannabis, and to make medical cannabis more accessible to those who need it, several countries have legalized cannabis for medical purposes. Some countries have gone a step further and legalized cannabis for recreational use. For example, in late 2018, the sale of recreational cannabis became legal in Canada.
The Cannabis Act initially allowed for “the cultivation, production and sale of dried cannabis flower, oil tinctures and oil capsules.”3 One year postlegalization, the Cannabis Act was amended to allow for the sale of cannabis edibles, topicals, infused beverages, vapes, and concentrates.3 Since legalization in Canada, several other countries around the world have made significant strides to follow suit, including Germany, Mexico, and the United States.4–6 Cannabis is not the first drug to be legally available for nonmedical use. Tobacco, alcohol, and caffeine have been freely available to the public for recreational use for decades. However, none of these substances are risk free, and all have associated side effects. These vary in severity depending on the substance, frequency of use, and dose administered (Table 1).
Table 1.
List of Common Substances/Drugs Available for Recreational Use, and their Corresponding Side Effects
| Drug/Substance | References | |
|---|---|---|
| Select side effects associated with overconsumption/long-term use | ||
| Alcohol | • Certain types of cancer | 90 |
| • High blood pressure, heart disease, stroke, and liver disease | ||
| • Mental health problems | ||
| • Dependency | ||
| Caffeine | • Nausea | 91 |
| • Dysphoria | ||
| • Insomnia | ||
| • Headache | ||
| Tobacco | • Lung, esophageal, larynx, and oral cavity cancers | 92 |
| • Various lung diseases | ||
| • Coronary heart disease | ||
| • Gum disease and tooth loss | ||
While a lethal overdose of cannabis seems unlikely in humans,7 this is perhaps not the best barometer to assess the safety of cannabis or its principle psychoactive component, Δ9-tetrahydrocannabinol (Δ9-THC). Afterall, smoking tobacco is unlikely to lead to a lethal nicotine overdose, yet this does not mean that tobacco is risk free. There is popular misconception regarding the safety of cannabis, and as academics interested in the clinical potential of cannabinoids, we feel duty bound to highlight these issues. Our motivation in writing this article is to stress that just because nonmedical cannabis use is becoming legal in many parts of the world doesn't mean it is safe.
Educating the Public and Breaking the Stigma
The safety profiles of recreational drugs are notoriously difficult to establish. It took 60 years for the damaging health effects of tobacco smoking to become mainstream knowledge.8 As the link between smoking and lung cancer was being established knowledge mobilization remained a challenge. This is in part due to the addictive nature of cigarette smoking and a consequence of the powerful marketing campaigns run by tobacco companies to influence the public (Fig. 1). In the case of cannabis, we now see extraordinary health and safety claims for this once controlled substance. These claims are usually spread via online forums and through social media, with only so-called “anecdotal evidence” offered for validation. The fact that cannabis is a natural substance and its use is becoming permissible across the globe should not be sufficient for people to think it is harmless. In reality there is very little evidence for many of the safety and medical claims that are made regarding cannabis. As researchers working in this space it is difficult to navigate the current landscape that is often littered with misinformation. In addition to this we must battle the stigma that is associated with researching these compounds. Our interest, along with that of many other researchers entering this space, stems from the potential of these exogenous cannabinoids to modulate the processes influenced by the human endocannabinoid system (ECS). These processes include appetite and energy balance, cardiovascular functions, cell apoptosis, neuronal development, immune modulation, neuronal plasticity, and reproductive functions.1
FIG. 1.
Posters from the early 1900s, taken from the collection of Stanford Research Into the Impact of Tobacco Advertising (tobacco.stanford.edu). Color images are available online.
Several exogenous cannabinoids have been shown to bind to human cannabinoid receptor 1 (CB1) and/or human cannabinoid receptor 2 (CB2). These cannabinoid receptors are ubiquitously expressed in almost every part of the human body. CB1 receptors are mainly located within the central nervous system,9 while CB2 receptors are found primarily on cells of the hematopoietic and immune systems.10–12 Interactions between certain exogenous cannabinoids and the human ECS also result in the sought-after recreational effects of cannabis. Despite the potential for abuse, there is growing evidence to support the clinical application of exogenous cannabinoids in certain disease states. This is exemplified by the FDAs recent approval of the plant-derived cannabidiol (CBD) formulation, Epidiolex® (GW Pharmaceuticals). Epidiolex is currently approved in the United States and Europe for the treatment of two rare forms of childhood epilepsy (Lennox-Gastaut Syndrome and Dravet Syndrome).
Even with the advances that have been made in the science of cannabinoids, there is still much we do not know about these compounds. Of concern, is the lack of safety data available for long-term exposure to these compounds (particularly in children and adolescents).
Cannabis Use and Mental Health
The question of how cannabis use affects mental health is of significant interest to both researchers and society. The harmful effects related to cannabis use may be amplified by both the degree of exposure and the age of initiation.13 As such, there is considerable concern that cannabis use among adolescents, young adults, and vulnerable individuals, may contribute to the development of mental health conditions, including anxiety and depressive disorders, use disorder, and psychosis.14
For younger adults and adolescents, it is postulated that this increased risk may be due to the interference of phytocannabinoids, particularly Δ9-THC, with ongoing brain development.15 Conversely, 16–24 year olds may be found to be most at risk because they comprise the portion of the population most likely to consume cannabis,2,16 and therefore the population most likely to experience the associated side effects.13,17–19 In addition, some vulnerable individuals may be more susceptible to developing various mental health disorders, regardless of cannabis consumption, but rather due to certain biological and sociological factors.20
Despite these confounding factors, there is growing evidence to suggest that cannabis use may have an impact on normal brain function and consequently may have a negative impact on mental health.
Cognitive impairment
Δ9-THC activates CB1 receptors in the brain to elicit its intoxicating effects. These effects tend to vary between individuals for several reasons including differential rates of Δ9-THC absorption and different levels of tolerance to Δ9-THC. Although not itself lethal, the impaired motor and cognitive function arising due to cannabis intoxication (i.e., Δ9-THC intoxication) is often associated with poor decision making and an increased risk of personal injury.
There is experimental evidence, from driving simulators, to suggest that cannabis intoxication impairs several cognitive skills related to driving ability.21 Despite this experimental evidence, the findings from epidemiological studies are not as clear, largely due to confounding factors such as multiple substance use, in particular concurrent consumption of cannabis and alcohol.21–23
However, overall the effects of cannabis intoxication have been linked with an increased risk of motor vehicle crash.24 Some studies conducted in the United States and Europe have suggested that crash risk may increase twofold to threefold due to cannabis intoxication.21,23,25 Although significant, the effects of alcohol intoxication are more substantial, and estimated to increase crash risk between 6- and 15-fold.25 Unsurprisingly, concurrent consumption of both cannabis and alcohol increases the risk of car accidents substantially more than consumption of either substance alone.21,23–25
Use disorder/addiction
Regular cannabis use can develop into an addiction in much the same way that addiction develops to other substances, such as opioids or tobacco. For example, the typical “high” felt by users yields the desire for repeated use, and for some cannabis users this desire can develop into cannabis use disorder (CUD).26 Cannabis users with earlier initiation times, that is, who begin their cannabis use earlier in life, and cannabis users with more exposure (i.e., more heavy cannabis use), are widely considered more at risk of developing CUD.
Some epidemiological studies have concluded that CUD has been one of the most common addictions, after alcohol and tobacco, over the past 20 years in Australia, Canada, and the United States.25 It is estimated that CUD affects 1–2% of adults who have used cannabis in the past year and 4–8% of adults who have used cannabis in their lifetimes.25,27,28 Overall, compared to other drugs of misuse (nicotine [32%]; heroin [23%]; cocaine [17%]; alcohol [15%]; and stimulants [11%]25,29,30), the rate of dependence on cannabis is relatively low (9–10%).25,28,31 Additionally, there is evidence that the “adverse health and social consequences associated with cannabis dependence are less severe than those associated with alcohol or opioids.”32
However, this does not mean that CUD should be regarded as a trivial illness. The majority of individuals who suffer from CUD seek professional attention to overcome this addiction. In the past two decades there has been a steady increase in the number of cannabis users seeking assistance to control or quit cannabis use in Europe, Australia, and the United States.25 In North American jurisdictions that have implemented new cannabis laws, there is potential for CUD rates to increase in the near future due to increased availability of cannabis. It has been estimated that there are almost 1 million and 10 million daily or near-daily users of cannabis in Canada and the United States, respectively.2 A recent study that tracked the rates of CUD following recreational legalization of cannabis in certain U.S. states, from 2008 to 2016, showed an increase in the risk of CUD in 12–17 year olds, and increased rates of CUD in adults over 26 years of age.32
The effects of cannabis legalization on rates of CUD in Canada have not yet been reported.
Psychosis
Several studies across different ethnic groups have shown that cannabis users with younger initiation times are more likely to have psychotic symptoms during adulthood.13,20,33–36 A recent multicenter case–control study suggests that daily high potency cannabis use (≥10% Δ9-THC) can result in an almost fivefold increase in the likelihood of being diagnosed with psychosis, compared with individuals who have never used cannabis.17 While other studies, that looked primarily at populations from the United States, Australia, New Zealand, and Europe, have suggested a two and four fold increase in risk of developing psychosis, for regular cannabis and heavy cannabis users, respectively.20,37,38 However, despite the findings from these studies, there is currently insufficient evidence to support an association between cannabis use and psychosis. Most psychosis patients have never used cannabis, and many cannabis users do not develop psychosis.25,34,39
In summary, initiation time and regular cannabis use may be connected to a higher risk of psychotic episodes; however, current evidence implies that cannabis use is just one factor in a complex collection of factors that can contribute to the development of psychosis.34,39 Other risk factors include age, in addition to, genetic and sociological factors.13,17–20
Anxiety disorders
In a 2017 survey of Canadians, over 50% of respondents declared that cannabis use improved their anxiety.40 However, current research does not align well with these survey results.
Data from the “Netherlands Mental Health Survey and Incidence Study” and the “National Epidemiological Survey on Alcohol and Related Conditions” (NESARC) in the United States identified cannabis as a potential causal factor in developing anxiety disorders, or in exacerbating symptoms in people who suffer from anxiety disorders.41–44 Other studies, confined to residents of Miami and Seattle, reported correlations with only certain types of anxiety disorders.45,46 While, studies on populations from Australia, the United Kingdom, Sweden, and the United States, wherein confounding factors such as childhood experience and cigarette use were controlled for, found no such associations.47–51 Preclinical and clinical research has suggested that the duration and dose of Δ9-THC administered may be correlated with anxiolytic and/or anxiogenic responses.52–54
Overall, more research is necessary to investigate the potential relationships between cannabis use and anxiety disorders.20
Depressive disorders
Similarly, some studies suggest that cannabis use can be correlated with the likelihood of being diagnosed with a depressive disorder. One long-term cohort study, namely, the “Cambridge Study in Delinquent Development,” reported that cannabis use, in particular with early initiation, increased the risk of being diagnosed with depression.55 Studies conducted on Australians, Swiss, and Canadians (Nova Scotians) reported this correlation to be more prominent in chronic cannabis users56,57; yet, with weekly cannabis use being enough to cause a depressive disorder.56,58 However, as is the case with anxiety, when controlling for confounding factors such as use of other substances, early childhood experience, and education, other studies conducted on Australians, Danes, and Americans (NESARC) reported no clear association between depression and cannabis use.47,59,60
Cannabis Use and Physical Health
Cannabinoids have been linked to a plethora of other side effects related to physical health. The majority of these are not yet well established and require further research. For example, the recent clinical approval of Epidiolex by the U.S. FDA included a request for nine additional clinical trials to better understand the impact of long-term CBD exposure on healthy volunteers.61 Given the extent to which the ECS is thought to regulate homeostasis, the side effects associated with phytocannabinoids, and in particular Δ9-THC, may be quite far reaching.
Vascular health
A recent review by Pacher et al., summarizes the effects of cannabis on cardiovascular health.62 Δ9-THC is a partial agonist of the CB1 receptor. The cardiovascular effects of recreational cannabis use can vary depending on Δ9-THC content of the product and the route of administration, that is, the effects of Δ9-THC are believed to be dose dependent.62 High doses of Δ9-THC have been shown to exert CB1 receptor mediated proinflammatory, pro-oxidant, and profibrotic effects. At low doses, Δ9-THC may exert CB2 receptor mediated tissue protective and anti-inflammatory effects.62 In rare cases acute exposure to Δ9-THC can result in life-threatening cardiovascular effects, such as myocardial infarction and ischemia.62 Some studies suggest these risks are higher in older adults.25 However, there have been numerous reports of adverse cardiovascular events in healthy young cannabis smokers.63–66 While more research is needed to fully determine the effect of cannabis and Δ9-THC on cardiovascular health, the preliminary evidence certainly warrants caution.
Gastrointestinal health
The ECS functions in the brain and the GI tract to help regulate energy balance and food intake. Δ9-THC can increase food uptake and inhibit gastric motor activity via CB1 receptor activation.67,68 Homeostasis in the gastrointestinal tract can be interrupted by chronic cannabis use. For example, cannabinoid hyperemesis syndrome is a rare condition that involves cyclic nausea and vomiting, which can be induced by long-term and intense cannabis use.67 The discovery that cannabinoid receptor agonists can influence gastrointestinal motility has made the ECS a possible target for the treatment of some gastrointestinal diseases such as Crohn's disease and ulcerative colitis. However, a major limitation for such cannabinoid-based gastrointestinal therapies is their potential side effects.67
Cancer risk
Given the established link between tobacco smoking and oncogenesis,69 it is reasonable to assume that comparable consequences may be associated with cannabis smoking, as both involve the burning and inhalation of dried plant material. Several studies conducted in North African, North American, European and Australian populations examined a possible link between cannabis smoking and oncogenesis.70–75
These data are summarized in a recent systematic review and meta-analysis by Ghasemiesfe et al.71 Briefly, for the majority of cancer types investigated, there is currently no strong evidence to support any association between cannabis smoking and oncogenesis.71 However, there is emerging evidence to suggest that daily use of cannabis is associated with an increased risk of developing testicular germ cell tumors.71 Three separate case–control studies suggest that the resulting increased risk could be up to twofold.76–78
In summary, long-term studies of cannabis only smokers are necessary to improve our understanding of any possible associations that might exist between cannabis use and certain types of cancer, in particular lung and oral cancers, which are commonly associated with tobacco smoking.71
Reproductive function
There is limited in vivo evidence to suggest that cannabis can negatively affect testosterone production and sperm mobility in men.79,80 In rats, the administration of “high levels of Δ9-THC has been shown to inhibit ovulation.”81,82 A recently published study has suggested that long-term exposure to Δ9-THC may result in infertility in men.83 Despite these potential links between cannabis use and impaired fertility, we currently lack concrete clinical evidence to understand the degree of risk. However, it is likely advisable for both men and women to avoid cannabis use when trying to conceive.
Outlook
In the past few decades the amount of Δ9-THC present in cannabis plants has been steadily increasing. In samples confiscated by the U.S. DEA the average potency of Δ9-THC has increased more than fourfold, from 4% (1995) to 17% (2017).84,85 This trend is not confined to the United States, nor to dried cannabis flower. Data from the United Nations show that black market cannabis concentrates and edibles typically contain up to 69% Δ9-THC, and in recent years there has been a five fold increase in the number of such products with greater than 75% Δ9-THC content.2
In Canada, licenced dispensaries are now stocking dried cannabis flowers that contain up to 30% Δ9-THC; High Tide Kade's Kush is available on the Alberta Cannabis website with a reported potency of 17–30% Δ9-THC.86 The Canadian government's recent approval of cannabis concentrates, cannabis edibles, cannabis beverages, and cannabis vape devices, is likely to lead to more offerings of high Δ9-THC potency products in 2020. This increase in availability of high Δ9-THC cannabis products in North America, along with the large numbers of daily or near-daily users,2,32 may exacerbate the number, type, and severity of cannabis-related side effects reported in the coming years.
One of the most common myths associated with cannabis is that it must be safe because it is a natural product and has been used for thousands of years. This misconception is reinforced through internet forums and social media, where cannabis is often described as a “panacea” for a wide range of medical conditions with only “anecdotal evidence” provided for support. The astrophysicist Carl Sagan once said that “extraordinary claims require extraordinary evidence.” In the current climate of increasing cannabis legality there appears to be no end to the “extraordinary claims” that people are willing to make regarding the safety and efficacy of this plant. However, we are nowhere near the “extraordinary evidence” necessary to back these claims, and while the evidence for the cannabis “panacea” may be lacking, the evidence for side effects associated with cannabis use is certainly not.
Contradicting these widespread health claims and educating the public on the risks of cannabis use are not easy tasks. Academic researchers and health care professionals have called for more to be done to change the public's attitude toward cannabis. As a scientific community we need to significantly increase our understanding of both the potential benefits and harms associated with acute and long-term exposure to cannabis and cannabinoids.
There is a fear that today's misconceptions regarding the safety of cannabis use may be judged by future generations in the same way that our generation now critiques the tobacco smoking era.
These fears extend beyond Δ9-THC. Perhaps one of the most concerning trends has been the recent use of cannabinoid products during pregnancy. Often these are CBD oils that are used as a “natural” remedy for nausea experienced during pregnancy.87 CBD and other cannabinoids have been shown to cross the blood-placenta barrier.88 Children who are prenatally exposed to cannabinoids are more likely to experience several developmental disorders, such as inattention, lower IQ scores, and academic underachievement.31 A recent preclinical study reported that cannabinoid exposure via lactation, “can delay a milestone of early childhood development, the trajectory of GABAs polarity transition,” which can impact early-life communication.89
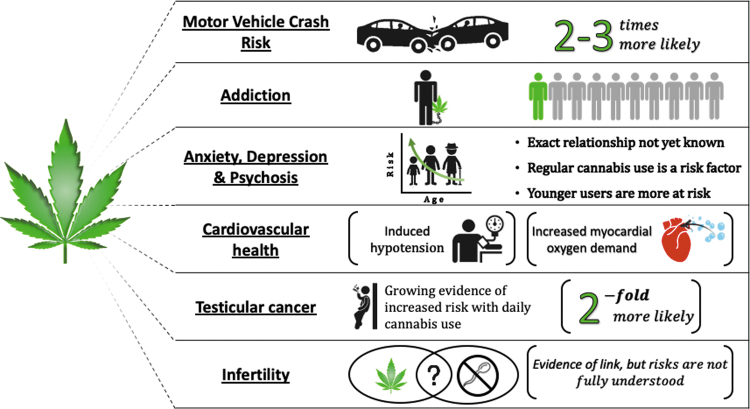
In summary, there is a growing body of evidence to suggest that regular cannabis use may have long-term health implications; these may include physical dependency and/or addiction, cognitive impairment, psychosis, anxiety and depressive disorders, cardiovascular issues, infertility, and possibly an increased risk of certain types of cancer (Fig. 2). However, even when the scientific literature on the health implications of cannabis use is examined (rather than internet forums, blogs, news headlines, etc.) contradictory data are found. It is clear that significantly more research is needed to fully understand the impact that recreational cannabis use has on our mental and physical health. The cannabis companies and governing authorities who are profiting from the legalization and sale of cannabis products to the general public should reinvest a portion of these funds into long-term safety studies of these compounds.
FIG. 2.
Diagram depicting some of the significant consequences and adverse effects that have been associated with recreational cannabis use. Color images are available online.
Abbreviations Used
Authors' Contributions
The article was written by all authors. All authors approved the final version of the article.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the opinions or position of Avicanna, Inc.
Author Disclosure Statement
C.A.'s research group at the University of Toronto has a sponsored research agreement with Avicanna, Inc., P.B. has an independent consulting agreement with Avicanna, Inc. For J.C.E., no competing financial interests exist.
Funding Information
C.A. has a sponsored research agreement with Avicanna Inc.
Cite this article as: Bannigan P, Evans JC, Allen C (2022) Shifting the paradigm on cannabis safety, Cannabis and Cannabinoid Research 7:1, 3–10, DOI: 10.1089/can.2020.0003.
References
- 1. Lu D, Potter DE. Cannabinoids and the cannabinoid receptors: an overview. In: Preedy VR, ed. Handbook of Cannabis and Related Pathologies. Elsevier: Cambridge, MA, 2017, pp. 553–563. [Google Scholar]
- 2. UNODC. World Drug Report 2019. UN, 2019. [Google Scholar]
- 3. Health Canada. The Cannabis Act. 2018. [Google Scholar]
- 4. Lovelace BJ. House committee approves landmark bill legalizing marijuana at the federal level. CNBC NEWS: Health and Science. November 20, 2019. [Google Scholar]
- 5. Williams S. Mexico Just Missed Its Deadline to Legalize Marijuana—Now What? 2019. Available at: Nasdaq.com (Accessed November 03, 2019).
- 6. Krishnan M. As Canadian Weed Companies Ramp Up in Germany, Patients Suffer. 2019. Available at: Vice.com (Accessed November 08, 2019).
- 7. Hall W, Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111:1764–1773. [DOI] [PubMed] [Google Scholar]
- 8. Proctor RN. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll: Table 1. Tob Control. 2012;21:87–91. [DOI] [PubMed] [Google Scholar]
- 9. Mackie K. Distribution of cannabinoid receptors in the central and peripheral nervous system. Handb Exp Pharmacol. 2005;168:299–325. [DOI] [PubMed] [Google Scholar]
- 10. Galiegue S, Mary S, Marchand J, et al. . Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem. 1995;232:54–61. [DOI] [PubMed] [Google Scholar]
- 11. Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61–65. [DOI] [PubMed] [Google Scholar]
- 12. Schatz AR, Lee M, Condie RB, et al. . Cannabinoid receptors CB1 and CB2: a characterization of expression and adenylate cyclase modulation within the immune system. Toxicol Appl Pharmacol. 1997;142:278–287. [DOI] [PubMed] [Google Scholar]
- 13. Casadio P, Fernandes C, Murray RM, et al. . Cannabis use in young people: the risk for schizophrenia. Neurosci Biobehav Rev. 2011;35:1779–1787. [DOI] [PubMed] [Google Scholar]
- 14. Hall W, Hoch E, Lorenzetti V. Cannabis use and mental health: risks and benefits. Eur Arch Psychiatry Clin Neurosci. 2019;269:1–3. [DOI] [PubMed] [Google Scholar]
- 15. Pope HG, Gruber AJ, Hudson JI, et al. . Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug Alcohol Depend. 2003;69:303–310. [DOI] [PubMed] [Google Scholar]
- 16. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). European Drug Report 2019: Trends and Developments. Publications Office of the European Union: Luxembourg, 2019. [Google Scholar]
- 17. Di Forti M, Quattrone D, Freeman TP, et al. . The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry. 2019;6:427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Murray RM, Englund A, Abi-Dargham A, et al. . Cannabis-associated psychosis: Neural substrate and clinical impact. Neuropharmacology. 2017;124:89–104. [DOI] [PubMed] [Google Scholar]
- 19. Mokrysz C, Freeman TP, Korkki S, et al. . Are adolescents more vulnerable to the harmful effects of cannabis than adults? A placebo-controlled study in human males. Transl Psychiatry. 2016;6:e961–e961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lowe DJE, Sasiadek JD, Coles AS, et al. . Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci. 2019;269:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sewell RA, Poling J, Sofuoglu M. The effect of cannabis compared with alcohol on driving. Am J Addict. 2009;18:185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Calabria B, Degenhardt L, Hall W, et al. . Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010;29:318–330. [DOI] [PubMed] [Google Scholar]
- 23. Dubois S, Mullen N, Weaver B, et al. . The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forensic Sci Int. 2015;248:94–100. [DOI] [PubMed] [Google Scholar]
- 24. Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction. 2016;111:1348–1359. [DOI] [PubMed] [Google Scholar]
- 25. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110:19–35. [DOI] [PubMed] [Google Scholar]
- 26. Budney AJ, Sofis MJ, Borodovsky JT. An update on cannabis use disorder with comment on the impact of policy related to therapeutic and recreational cannabis use. Eur Arch Psychiatry Clin Neurosci. 2019;269:73–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hall W, Pacula RL. Cannabis use and dependence: public health and public policy. Cambridge University Press: Cambridge, 2003. [Google Scholar]
- 28. Roffman R, Stephens RS. eds. Cannabis dependence: its nature, consequences and treatment. Cambridge University Press: Cambridge, 2006. [Google Scholar]
- 29. Hall W, Teesson M, Lynskey M, et al. . The 12-month prevalence of substance use and ICD-10 substance use disorders in Australian adults: findings from the National Survey of Mental Health and Well-Being. Addiction. 1999;94:1541–1550. [PubMed] [Google Scholar]
- 30. Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol. 1994;2:244–268. [Google Scholar]
- 31. Memedovich KA, Dowsett LE, Spackman E, et al. . The adverse health effects and harms related to marijuana use: an overview review. CMAJ Open. 2018;6: E339–E346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cerdá M, Mauro C, Hamilton A, et al. . Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol Med. 2003;33:15–21. [DOI] [PubMed] [Google Scholar]
- 34. Arseneault L, Cannon M, Witton J, et al. . Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry. 2004;184:110–117. [DOI] [PubMed] [Google Scholar]
- 35. Stefanis NCDelespaul P, Henquet C, et al. . Early adolescent cannabis exposure and positive and negative dimensions of psychosis. Addiction. 2004;99:1333–1341. [DOI] [PubMed] [Google Scholar]
- 36. Konings M, Henquet C, Maharajh HD, et al. . Early exposure to cannabis and risk for psychosis in young adolescents in Trinidad. Acta Psychiatr Scand. 2008;118:209–213. [DOI] [PubMed] [Google Scholar]
- 37. Di Forti M, Morgan C, Dazzan P, et al. . High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009;195:488–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marconi A, Di Forti M, Lewis CM, et al. . Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42:1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. D'Souza DC, Sewell RA, Ranganathan M. Cannabis and psychosis/schizophrenia: human studies. Eur Arch Psychiatry Clin Neurosci. 2009;259:413–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Government of Canada. Canadian cannabis survey 2017—summary. 2017. Available at: https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/canadian-cannabissurvey-2017-summary.html (Accessed November 10, 2019).
- 41. Cougle JR, Hakes JK, Macatee RJ, et al. . Quality of life and risk of psychiatric disorders among regular users of alcohol, nicotine, and cannabis: an analysis of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). J Psychiatr Res. 2015;66–67:135–141. [DOI] [PubMed] [Google Scholar]
- 42. Feingold D, Weiser M, Rehm J, et al. . The association between cannabis use and anxiety disorders: results from a population-based representative sample. Eur Neuropsychopharmacol. 2016;26:493–505. [DOI] [PubMed] [Google Scholar]
- 43. Tournier M, Sorbara F, Gindre C, et al. . Cannabis use and anxiety in daily life: a naturalistic investigation in a non-clinical population. Psychiatry Res. 2003;118:1–8. [DOI] [PubMed] [Google Scholar]
- 44. van Laar M, van Dorsselaer S, Monshouwer K, et al. . Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population? Addiction. 2007;102:1251–1260. [DOI] [PubMed] [Google Scholar]
- 45. Guttmannova K, Kosterman R, White HR, et al. . The association between regular marijuana use and adult mental health outcomes. Drug Alcohol Depend. 2017;179:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Duperrouzel J, Hawes SW, Lopez-Quintero C, et al. . The association between adolescent cannabis use and anxiety: a parallel process analysis. Addict Behav. 2018;78:107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Degenhardt L, Hall W, Lynskey M. The relationship between cannabis use, depression and anxiety among Australian adults: findings from the National Survey of Mental Health and Well-Being. Soc Psychiatry Psychiatr Epidemiol. 2001;36:219–227. [DOI] [PubMed] [Google Scholar]
- 48. Danielsson A-K, Lundin A, Agardh E, et al. . Cannabis use, depression and anxiety: a 3-year prospective population-based study. J Affect Disord. 2016;193:103–108. [DOI] [PubMed] [Google Scholar]
- 49. Gage SH, Hickman M, Heron J, et al. . Associations of cannabis and cigarette use with depression and anxiety at age 18: findings from the Avon longitudinal study of parents and children. PLoS One. 2015;10:e0122896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Scholes-Balog KE, Hemphill SA, Evans-Whipp TJ, et al. . Developmental trajectories of adolescent cannabis use and their relationship to young adult social and behavioural adjustment: a longitudinal study of Australian youth. Addict Behav. 2016;53:11–18. [DOI] [PubMed] [Google Scholar]
- 51. Zvolensky MJ, Lewinsohn P, Bernstein A, et al. . Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. J Psychiatr Res. 2008;42:1017–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Harte-Hargrove LC, Dow-Edwards DL. Withdrawal from THC during adolescence: sex differences in locomotor activity and anxiety. Behav Brain Res. 2012;231: 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bhattacharyya S, Egerton A, Kim E, et al. . Acute induction of anxiety in humans by delta-9-tetrahydrocannabinol related to amygdalar cannabinoid-1 (CB1) receptors. Sci Rep. 2017;7:15025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kasten CR, Zhang Y, Boehm SL. Acute and long-term effects of Δ9-tetrahydrocannabinol on object recognition and anxiety-like activity are age- and strain-dependent in mice. Pharmacol Biochem Behav. 2017;163:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Schoeler T, Theobald D, Pingault J-B, et al. . Developmental sensitivity to cannabis use patterns and risk for major depressive disorder in mid-life: findings from 40 years of follow-up. Psychol Med. 2018;48:2169–2176. [DOI] [PubMed] [Google Scholar]
- 56. Horwood LJ, Fergusson DM, Coffey C, et al. . Cannabis and depression: an integrative data analysis of four Australasian cohorts. Drug Alcohol Depend. 2012;126:369–378. [DOI] [PubMed] [Google Scholar]
- 57. Rasic D, Weerasinghe S, Asbridge M, et al. . Longitudinal associations of cannabis and illicit drug use with depression, suicidal ideation and suicidal attempts among Nova Scotia high school students. Drug Alcohol Depend. 2013;129:49–53. [DOI] [PubMed] [Google Scholar]
- 58. Baggio S, N'Goran AA, Deline S, et al. . Patterns of cannabis use and prospective associations with health issues among young males. Addiction. 2014;109:937–945. [DOI] [PubMed] [Google Scholar]
- 59. Feingold D, Weiser M, Rehm J, et al. . The association between cannabis use and mood disorders: a longitudinal study. J Affect Disord. 2015;172:211–218. [DOI] [PubMed] [Google Scholar]
- 60. Østergaard MLD, Nordentoft M, et al. . Associations between substance use disorders and suicide or suicide attempts in people with mental illness: a Danish nation-wide, prospective, register-based study of patients diagnosed with schizophrenia, bipolar disorder, unipolar depression or personal. Addiction. 2017;112:1250–1259. [DOI] [PubMed] [Google Scholar]
- 61. U.S. Food and Drug Administration. Clinical Pharmacology and Biopharmaceutics Review(s). Centre for Drug Evaluation and Research, 2017. [Google Scholar]
- 62. Pacher P, Steffens S, Haskó G, et al. . Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol. 2018;15:151–166. [DOI] [PubMed] [Google Scholar]
- 63. Jouanjus E, Leymarie F, Tubery M, et al. . Cannabis-related hospitalizations: unexpected serious events identified through hospital databases. Br J Clin Pharmacol. 2011;71:758–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hartung B, Kauferstein S, Ritz-Timme S, et al. . Sudden unexpected death under acute influence of cannabis. Forensic Sci Int. 2014;237:e11–e13. [DOI] [PubMed] [Google Scholar]
- 65. Mostofsky E, Maclure M, Sherwood JB, et al. . Risk of acute myocardial infarction after the death of a significant person in one's life. Circulation. 2012;125:491–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sánchez Artiles AE, Awan A, Karl M, et al. . Cardiovascular effects of cannabis (marijuana): a timely update. Phyther Res. 2019;33:1592–1594. [DOI] [PubMed] [Google Scholar]
- 67. Sałaga M, Abalo R, Fichna J. Cannabis and cannabinoids and the effects on gastrointestinal function: an overview. In: Preedy VR, ed. Handbook of Cannabis and Related Pathologies. Elsevier: Cambridge, MA, 2017, pp. 471–480. [Google Scholar]
- 68. Krowicki ZK, Moerschbaecher JM, Winsauer PJ, et al. . Δ9-Tetrahydrocannabinol inhibits gastric motility in the rat through cannabinoid CB1 receptors. Eur J Pharmacol. 1999;371:187–196. [DOI] [PubMed] [Google Scholar]
- 69. Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45:S3–S9. [DOI] [PubMed] [Google Scholar]
- 70. Hashibe M, Straif K, Tashkin DP, et al. . Epidemiologic review of marijuana use and cancer risk. Alcohol. 2005;35:265–275. [DOI] [PubMed] [Google Scholar]
- 71. Ghasemiesfe M, Barrow B, Leonard S, et al. . Association between marijuana use and risk of cancer. JAMA Netw Open. 2019;2:e1916318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Aldington S, Harwood M, Cox B, et al. . Cannabis use and risk of lung cancer: a case-control study. Eur Respir J. 2008;31:280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Berthiller J, Straif K, Boniol M, et al. . Cannabis smoking and risk of lung cancer in men: a pooled analysis of three studies in Maghreb. J Thorac Oncol. 2008;3:1398–1403. [DOI] [PubMed] [Google Scholar]
- 74. Zhang LR, Morgenstern H, Greenland S, et al. . Cannabis smoking and lung cancer risk: pooled analysis in the International Lung Cancer Consortium. Int J Cancer. 2015;136:894–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Jett J. IBS11.03 cannabis and lung cancer. J Thorac Oncol. 2019;14:S102. [Google Scholar]
- 76. Daling JR, Doody DR, Sun X, et al. . Association of marijuana use and the incidence of testicular germ cell tumors. Cancer. 2009;115:1215–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lacson JCA, Carroll JD, Tuazon E, et al. . Population-based case-control study of recreational drug use and testis cancer risk confirms an association between marijuana use and nonseminoma risk. Cancer. 2012;118:5374–5383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Trabert B, Sigurdson AJ, Sweeney AM, et al. . Marijuana use and testicular germ cell tumors. Cancer. 2011;117:848–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Barnett G, Chiang C-WN, Licko V. Effects of marijuana on testosterone in male subjects. J Theor Biol. 1983;104:685–692. [DOI] [PubMed] [Google Scholar]
- 80. Kolodny RC, Masters WH, Kolodner RM, et al Depression of plasma testosterone levels after chronic intensive marihuana use. N Engl J Med. 1974;290:872–874. [DOI] [PubMed] [Google Scholar]
- 81. Treinen KA, Sneeden JL, Heindel JJ. Specific inhibition of FSH-stimulated cAMP accumulation by Δ9-tetrahydrocannabinol in cultured rat granulosa cells. Toxicol Appl Pharmacol. 1993;118:53–57. [DOI] [PubMed] [Google Scholar]
- 82. Walker OS, Holloway AC, Raha S. The role of the endocannabinoid system in female reproductive tissues. J Ovarian Res. 2019;12:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Nielsen JE, Rolland AD, Rajpert-De Meyts E, et al. . Characterisation and localisation of the endocannabinoid system components in the adult human testis. Sci Rep. 2019;9:12866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. ElSohly MA, Mehmedic Z, Foster S, et al. . Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiatry. 2016;79:613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Chandra S, Radwan MM, Majumdar CG, et al. . New trends in cannabis potency in USA and Europe during the last decade (2008–2017). Eur Arch Psychiatry Clin Neurosci. 2019;269:5–15. [DOI] [PubMed] [Google Scholar]
- 86. Alberta Gaming, Liquor and Cannabis. Available at: https://albertacannabis.org (Accessed November 10, 2019).
- 87. Young-Wolff KC, Sarovar V, Tucker LY, et al. . Association of nausea and vomiting in pregnancy with prenatal marijuana use. JAMA Intern Med. 2018;178:1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Grant KS, Petroff R, Isoherranen N, et al. . Cannabis use during pregnancy: pharmacokinetics and effects on child development. Pharmacol Ther. 2018;182:133–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Scheyer AF, Borsoi M, Wager-Miller J, et al. . Cannabinoid exposure via lactation in rats disrupts perinatal programming of the gamma-aminobutyric acid trajectory and select early-life behaviors. Biol Psychiatry. 2020;87:666–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Centers for Disease Control and Prevention (CDC). Alcohol and Public Health. 2018. Available at: https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm (Accessed November 15, 2019).
- 91. U.S. Food and Drug Administration, “Spilling the Beans: How Much Caffeine is Too Much?” 2018. Available at: https://www.fda.gov/consumers/consumer-updates/spilling-beans-how-much-caffeine-too-much (Accessed November 15, 2019).
- 92. Centers for Disease Control and Prevention (CDC). Smoking and Tobacco Use. 2018. Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/tobacco_industry/cigars/index.htm#effects (Accessed November 15, 2019).