Abstract
Background:
Timely rehabilitation in patients with Breast Cancer (BC) has a great impact on improving their physical and mental conditions. Thus, the appropriate follow-up method is essential especially during the Covid-19 pandemic. The aim of this study was to review the different technology-assisted interventions for improving physical activity in BC patients.
Materials And Methods:
In this systematic review, the original studies were extracted from the beginning of indexing in databases including PubMed, Scopus, Google Scholar, and Web of Science until 2019. Finally, 45 papers were included in this study based on the inclusion criteria for before the Covid-19 pandemic and 3 articles extracted for the Covid-19 period.
Results:
The most widely used technologies for BC patients were in the United States (46.67%). Telephone, mobile application, and web with 28.89%, 15.56%, and 8.89% frequencies were the most common technologies, respectively. Although the majority of the participants were satisfied with the intervention method, in some cases, the patients were unsatisfied due to the complexity of the technology. These technologies were used for various purposes, such as physical activity and functions, control of pain severity, fitness, quality of life, diet behavior, fatigue, muscle strength, cardio-respiratory capacity, as well as arm and shoulder exercises.
Conclusions:
In conclusion, virtual communication can improve the health of BC patients and also increases patients' desire and hope to continue treatment. It is worth noting that in the Covid-19 pandemic, with the strengthening of virtual communication infrastructure, more attention was paid to BC patients due to their sensitive conditions.
Keywords: Breast neoplasms, Covid-19, exercise, telemedicine, telerehabilitation
Introduction
The incidence and mortality of Breast Cancer (BC) have increased in recent decades. According to the latest GLOBOCAN statistics, BC is the second most common cancer in the world (11.6%). In women, it is the leading cause of cancer deaths with 6.6%.[1] Appropriate policy and solution should be considered in order to the early detection, diagnosis, treatment, and follow-up of these patients.[2]
The follow-up is performed either by direct contact with healthcare providers or through the review of medical records or technology-based methods. BC patients have many problems in hand-grip strength, physical activity, social interactions, and Quality of Life (QoL), especially after surgery.[3] Studies have shown that physical activity in these patients can be improved by rehabilitation programs and interventions. Conventional healthcare due to time constraints, distance restrictions, high cost, and even disease transmission in the current situation imposes some limitations in the follow-up of BC patients. On the other hand, Covid-19 has a greater effect on vulnerable groups such as cancer patients. According to categorizing BC patients into priority levels (A, B, C) for emergency care, patients in priority C can receive some services at home.[4]
Actually, the increasing availability of technology and smart-phone make the opportunity to create real-time virtual communication between health care providers, especially nurses and patients. This leads to increased access to health care services when there are problems in face-to-face communication. Assistive technologies, such as telehealth are suitable and convenient solutions for providing care, regardless of time and distance constraints to improve the physical activity and functional capacity of BC patients.[5] It is important to note that, Covid-19 has also disrupted the provision of health care services to most patients, especially BC patients. Actually, they are at high risk of infection and have a complication, thus some patient cancels the face-to-face appointments due to the fear of infection and travel restrictions. The use of technology in special situations such as the Covid-19 pandemic has increased significantly due to its many benefits for managing different diseases especially cancer.[6] Telerehabilitation can be applying to help breast cancer patients, due to the high risk of face-to-face appointments. Therefore, the purpose of this study was to review the different Telerehabilitation technologies and the results of their interventions that are associated with physical activities and the quality of life of BC patients. All types of Telerehabilitation technologies were included in this study such as telephone, internet, videoconferencing, and other approaches. Authors review technology type and purpose, population, and result of the intervention.
Material and Methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). Figure 1 displays the process of PRISMA for data collection and analysis. The papers were searched from the following databases including PubMed, Scopus, Google Scholar, and Web of Science from the beginning of the activity of databases to 2019. The Population (P), Intervention (I), Comparison (C), and Outcome (O) (PICO) criteria were used to define the search string. The population was BC patients. Interventions had to be designed to improve physical activity, fitness, exercise, weight loss, and diet. The employed technologies included mobile application, telephone, web, email, smartwatch, pedometer, social media, tele-video, internet, and wearable device. In comparison criteria, groups without any intervention were compared with groups with technology-based interventions. In the outcome, the health status of BC patients' was reported. The search string was: “breast cancer” OR “breast neoplasms” OR “mastectomy” AND “exercise” OR “exercise therapy” OR “physical fitness” AND “blog” OR “telephone” OR “telemedicine” OR “social media” OR “internet” OR “wearable technology”. Moreover, search for studies after Covid-19 was conducted separately with a time limit of 2019-2020. In addition to the keywords listed above, these words were also added in the manual search including (Covid-19 OR Coronavirus 2019 OR SARS-CoV-2 infection OR COVID-19 pandemic OR Coronavirus disease 2019 OR COVID-19 virus infection).
Figure 1.
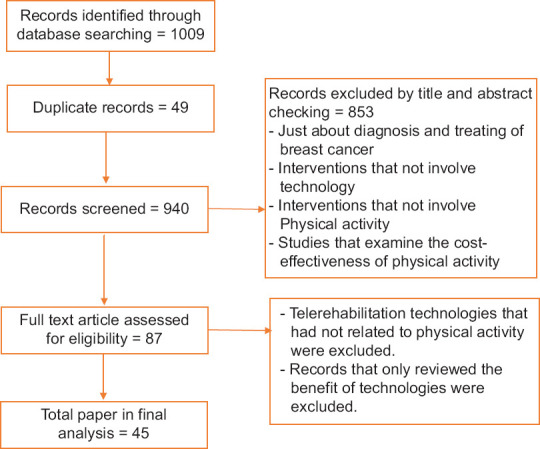
The process of preferred reporting items for systematic reviews and meta-analysis for data collection and analysis
The selection process was done in 4 stages. Firstly, the papers were screened based on the title by two reviewers. The screened articles were divided into three groups; i.e., zero groups did not have inclusion criteria. Another group that definitely had the inclusion criteria was assigned the number 1. The last group was assigned the number 2; reviewers were skeptical about selecting it. Moreover, the reviewers discussed papers that did not receive the same number and decided about them. All the papers which receive the same number (one or two) were included for the next phase. Finally, the full text of the included papers was obtained for the second-stage screening and then assessed by two reviewers. Then, variables were extracted in order to answer the research questions. These variables were the population, type of technology, time and type of intervention, their purposes, and the result of improvement.
This review responds to the following research questions: RQ 1: Which results have been reported after applying different technologies for these patients? RQ 2: For which countries, states, or cities, physical rehabilitation technology in order to physical activity have been designed? RQ 3: Which technological interventions have been used to promote the health of BC patients? RQ 4: What are the main purposes of using the technology in this disease?
RQ 5: Which research methods have been used for representing technological interventions among BC patients? RQ 6: What was the duration of each intervention?
Ethical Considerations
In this study, all relevant ethical codes have been observed. The author conducted a comprehensive search that identifies all eligible studies in this area. The content review has been done without bias. The principle of fidelity and the rights of authors in the use of the content have been observed.
Results
Pre-Covid-19 period
A total of 45 articles were extracted for the pre-Covid-19 period according to the criteria mentioned in the method section. The six variables including population, type of technology, time and type of intervention, their purposes, and the result of the intervention of the selected papers are presented in Table 1.
Table 1.
Some examples of studies about applying telehealth technologies to follow-up of breast cancer patient
| Author/year | Setting/population | Purpose of intervention | Type of intervention | Intervention in control group | Method/time | Results |
|---|---|---|---|---|---|---|
| Vallance et al. (2019)[7] | Alberta/Canada | Physical activity, fatigue and QoL* | Wearable device (Actigraph® and activPALTM accelerometers**) | Non | RCT***/4 M**** | The fatigue profile was improved. But effect not seen in QoL. |
| Lynch et al. (2019)[8] | Australia | Physical activity (PA) | Wearable technology*****, telephone counseling | Non | RCT/12W****** | Increase of PA******* was proved. |
| Kokts-Porietis et al. (2019)[9] | Canada | PA | Wearable technology (Polar A360® activity tracker********) | traditional treatment and rehabilitation according to daily specifications of the hospital | RCT, interview/12W | Technology was as a facilitator to physical activity, but technologic difficulties created a barrier to physical activity adherence. |
| Nápoles et al. (2019)[10] | United States | PA, health behavior | Booklet- Spanish-language mobile phone app - activity tracker- telephone counseling | Non | Sampling/2M | The PA and health behaviors of participants increased significantly. |
| Dong et al. (2019)[11] | China | PA | Phone, social media apps, tele-video | Traditional treatment and rehabilitation according to daily specifications of the hospital | RCT/12W | Positive effect on quality of life, muscle strength and cardiorespiratory capacity. |
| Pope et al. (2018)[12] | Minneapolis, USA | PA | Facebook- and mobile app (MapMyFitness) | RCT/10 W | Increasing physical activity by Facebook, Impact of the smart watch was not proven (due to difficulty). | |
| Lozano-Lozano et al. (2018)[13] | Spain | Diet and PA, body composition, muscular strength, upper body functionality and physical fitness | mHealth (BENECA)- tri-axial accelerometer | BENECA app for 8 weeks and usual care information | RCT/1M | It can be effective tool for managing breast cancer patient’s diet and PA behaviors. |
| Anderson et al. (2018)[14] | Scotland | PA, diet behavior and weight loss. | Telephone counseling and web support | Usual care | RCT/12W | Desired results were obtained from the intervention. |
| Lee et al. (2018)[15] | South Korea | Exercise | Mobile application | - | Retrospective/12W | Scores of patients with intervention were significantly higher than patients without intervention.Mutual feedback will increase user loyalty and motivational technology. |
| Van de Wiel et al. (2018)[16] | Netherlands | Physiotherapy counseling | Internet-based Physical Activity Support program (IPAS) and Telephone Support (TS) | Non | RCT/6 & 12 M | The effectiveness on IPAS********* alone or with TS********** in improvement of PA, QoL and fatigue was proved. |
| Hayes et al. (2011)[17] | Queensland/Australia | Exercise (aerobic) and PA | Telephone counseling | Usual care | RCT/8 M | The intervention had positive effect on survival. |
| Uhm et al. (2017)[18] | South Korea | Exercise (Aerobic and resistance exercises), physical function, and Quality of Life (QoL) | mHealth app (Smart After Care) with In Body Band Pedometer*********** | - | Prospective, quasi-randomized multicenter trial/6 &12W | Improve physical function, physical activity and QoL. |
| Lahart et al. (2017)[19] | United Kingdom | Cardiorespiratory fitness | Telephone | Usual care | RCT/6M | Increased cardiorespiratory fitness and self-reported PA. |
| Hartman et al. (2017)[20] | San Diego/USA | Exercise | Telephone and emails | Usual care | RCT/12W | The intervention improved the physical activity |
| Krebs et al. (2017)[21] | United States | PA and Healthy Eating | DVD************ | Advice and counseling alone | RCT/12W | Greater improvement in eating behavior change than physical activity. |
| Valle et al. (2017)[22] | United States | PA, weight loss | Wireless scale with data transfer capability to Website/mobile app | Usual care | RCT/24W | Preventing of weight gain was positive in both groups. |
| Cox et al. (2017)[23] | USA | PA and weight loss | Internet or telephone | Internet | RCT/6M | The outcomes of intervention in telephone group were better than internet group. |
| Lawler et al. (2017)[24] | Queensland/Australia | PA, diet and weight loss | Telephone | ---- | Pre-post study/6M | Positive effect on PA and weight loss of participants. |
| Harder et al. (2017)[25] | United Kingdom | Arm and shoulder exercises | Mobile app | ----- | Focus group | Self-management of arm and shoulder exercises was proved. |
| Fazzino et al. (2017)[26] | United States | Weight management and PA | Group phone sessionsmailed newsletterspedometer | ------ | RCT/6M | The PA of participants improved |
| Ritvo et al. (2017)[27] | Canada | PA | Telephone, Smart phone (iMovie), wearable technology | Only 12-week physical activity program | RCT/12W | Will assess |
| Ollero et al. (2017)[28] | - | Monitor heart rate, energy expenditure, arm mobility | Smart watch, smart phone, web server application | - | System design | The patients have not been evaluated. Only software and application were evaluated. |
| Ariza-Garcia et al. (2019)[29] | Spain | Exercise | Web-based (e-CUIDATE system) | Usual care | RCT/6-8 M | Global health status, physical, role, cognitive functioning, and arm symptoms, pain severity, and pain interference was improved. |
| Reeves et al. (2016) Australia[30] | The University of Queensland | Weight loss | Telephone counseling, posted materials and text-message | Usual care | RCT/6 &12 & 18 | The intervention had positive effect on PA, weight loss and other examined criteria. |
| Quintiliani et al. (2016)[31] | United States | Weight, diet and physical activity. | Text message- pedometer- phone counseling | Usual care | Pre-post study/10W | Weight of participants decreased. Dietary behavior improved. PA increased |
| Cadmus-Bertram et al. (2016)[32] | United States | PA | Telephone and web-based self-monitoring tools. | Usual care | RCT/12M | The PA and weight condition of participants improved significantly |
| Harrigan et al. (2016)[33] | United States | Weight loss | Telephone and in-person counseling. | Usual care | RCT/3M | The both interventions led to significant weight loss via increasing PA and favorable diet changes |
| Lyons et al. (2016)[34] | United States | Fitness and physical activity | Mobile application | Mobile application + narrative-based active video game. | RCT/6M | Improve breast cancer survivors’ health |
| Forbes et al. (2015)[35] | Nova Scotia/Canada | PA | PA tracking website UWALK | Usual care | RCT/9W | Intervention was successful in changing PA behavior. |
| McCarroll et al. (2015)[36] | United States | Control overweight. | Mobile app (LoseIt!) in website and mobile versions. | Usual care | Prospective/1M | The patients PA increased significantly. |
| Kyung Lee et al. (2014)[37] | South Korea | Promoting exercise (aerobic), dietary behaviors, and self-efficacy. | Web-based Self-Management Exercise and diet Intervention (WSEDI) | Booklet on exercise and diet | RCT/12W | Better results in the intervention group |
| De Cocker et al. (2014)[38] | Belgium | PA | Web and pedometer-based PA advice program | - | Pilot/3W | The usability and acceptability of program for PA proved. |
| Short et al. (2017)[39] | Queensland/Australia | PA | Website | - | RCT/12W | Positive effect on increasing PA in breast cancer survivors. |
| Winger et al. (2014)[40] | United States | Exercise and diet. | Telephone and mailed print | Non | RCT/-1Y************* | more positive results of the telephone intervention |
| Rock et al. (2013, 2015)[41,42] | United States | Effect of intervention on weight loss. | Telephone counseling and tailored newsletters | Usual care | RCT/2Y | The intervention group had significantly weight loss comparing with control group. |
| Hatchett et al. (2012)[43] | The University of Mississippi/USA | PA | Usual care | RCT/6 and 12M | Increased physical activity and exercise behavior. | |
| Ligibel et al. (2012)[44] | United States | Exercise | Telephone | Usual care | RCT/16M | Increase PA, physical functioning, and fitness. |
| Demark-Wahnefried et al. (2012)[45] | United States | Diet-exercise to control overweight or obese | Telephone counseling and print materials. | Wait-list control | RCT/2Y | Diet quality, PA, Physical function and BMI were improved significantly. |
| Eakin et al. (2012)[46] | Australia, Queensland | Aerobic and resistance exercise | Telephone | Non | RCT/8Y | Improve the physical activity and fitness |
| Lee et al. (2011)[47] | South Korea | PA and diet behaviors | Telephone and workbook | Non | RCT/12W | The PA increased significantly. Diet behaviors and QOL was improved. |
| Hegel et al. (2011)[48] | Hanover, USA | Quality of Life | Telephone | Usual care | RCT/6 and 12 W | Increase quality of life, Increase emotional state |
| Morey et al. (2009)[49] | United States | PA and diet | Telephone counseling, Automated telephone messages and mailed materials. | Delayed intervention | RCT/4M | PA and health behavior increased significantly in intervention group |
| Pinto et al. (2015)[50] | United States | PA | Telephone | Usual care | RCT/12 W | Increased physical activity, improved fitness and some aspects of psychological well-being |
| Matthews et al. (2007)[51] | United States | PA behaviors, body weight and body composition | Telephone | Usual care | RCT/12W | The level of PA increased in intervention group. No significant change in body weight. |
| Vallance et al. (2007)[52] | Alberta/Canada | PA and QoL | Wearable device and Print Materials | Print materials | RCT/7 M | Effectiveness of each intervention alone proved. Also, the combined approach produces better results. |
QoL*: Quality of Life. Accelerometers**: Device that measures proper acceleration (the rate of change of velocity). RCT***: Randomized Controlled Trial. M****: Month. wearable technology*****: The electronic device that can be embedded in user’s body or clothes. W******: Week. PA*******: Physical Activity. Activity tracker********: Device such as smart watches that monitoring fitness related indicators. IPAS*********: Internet-based Physical Activity Support Program. TS**********: Telephone Support. Pedometer***********: Electronic device that counts steps of a person by detecting the motion of the person’s hands or hips. It measures and encourage physical activity in adults. DVD************: Digital Video Disk. Y*************: Year
Population
The countries that used technology interventions to rehabilitate patients were the United States, Australia, South Korea, and Canada, respectively [refer to Table 1]. Figure 1 depicts the frequency of Telerehabilitation in different countries.
Intervention technologies
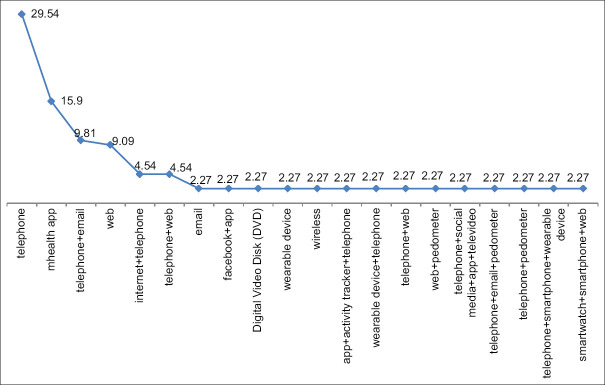
As presented in Table 1, various technologies were used in order to rehabilitate BC patients including telephone, web, mobile health application, etc. In 36.35% of the studies, the combinations of these technologies including phone plus mobile application, phone plus web, and phone plus internet were used to improve the physical activity of BC patients. The types of these technologies with their frequency are reported in Figure 2.
Figure 2.
Frequency of used technology in telerehabilitation of breast cancer patients
Purpose of technologies intervention
According to Table 1, technologies used in BC patients for physical activity by different purposes were summarized as global health status, physical, cognitive functioning, pain severity, pain interference, physical activity, fitness, quality of life, emotional state, eating behavior, fatigue, physical function, muscle strength, cardiorespiratory capacity, self-management of arm and shoulder exercises, diet quality, Body Mass Index (BMI), and exercise behavior.
Time and type of intervention
As shown in Table 1, researchers have applied technologies in various times intervals in order to evaluate the physical activity of BC patients by several types of methods. In most of the studies in different time periods, technology interventions have had a positive effect on the population. The maximum time of using the intervention was eight years in the Australian population and the majority of the studies have applied Randomized Controlled Trial (RCT).
Results of intervention
Although, in very few cases, patients complained about the complexities of some technologies, almost all the studies have shown patient satisfaction and have yielded positive results. The next point was that they tended to interact with health care providers.
Different age ranges
Various technologies have been employed to improve physical activity in diverse age ranges and different stages of the disease.
Studies during Covid-19 outbreak
Although the time period of this article was until 2019, since cancer patients are generally at greater risk during the Covid-19 period, keywords according to the criteria mentioned in the method section, with Covid-19 (Coronavirus disease) were searched in the specified databases. The detailed information extracted from the articles is shown in Table 2.
Table 2.
Examples of studies during Covid-19 period about applying tele technologies to follow-up of BC* patients
| Author/year | Setting/population | Purpose of intervention | Type of intervention | Intervention in control group | Method/time | Results |
|---|---|---|---|---|---|---|
| Mella-Abarca et al. (2020)[53] | Chile | Telerehabilitation | Phone calls and individual or group video calls | Non | Session was approximately 50 min, and frequency of session was different synchronous and asynchronous consultations | Both patients and physiotherapists had a high level of acceptance and satisfaction of tele-rehabilitation |
| Lytras et al. (2020)[54] | Greece | Telephysiotherapy | Skype | Non | 15 days and one hour every day/case-study | Volume of the lymph was significantly reduced |
| Grazioli et al. (2020)[6] | Italia | Exercise for physical fatigue and QoL | Whats app video call | Non | Case study/16W | Positive effects of combined training CT** on QoL and fatigue perception |
*BC: Breast cancer. **CT: Controlled trial
Discussion
In studies before Covid-19, after categorizing different variables in the physical rehabilitation of BC patients based on technology, authors answered the question in this field. Intervention technologies were mainly used in the United States (46.67%). Telephone (28.89%) and mobile application (15.56%) were the most frequent intervention technologies used for the physical rehabilitation of BC patients. The maximum intervention time was eight years.[41] One of the notable points in the selected studies was using RCT to evaluate the result; it means that the impact of interventions was carefully measured.
After the United States, Australians had the highest use of these technologies. Scotland, China, Belgium, and the Netherlands employed these technologies in equal proportions to rehabilitate BC patients. Different technologies were applied to various age groups and different stages of this disease. Although the phone was employed for patient rehabilitation alone and extensively, it was also used in combination with other technologies such as wearable devices and pedometers.[18,26,31,55] Our study did not exclude any intervention technologies and covered just BC survivors, while Haberlin et al.[56] excluded the interventions of telephone calls, SMS, or conference calls and covered all cancer types.
In a large number of studies, the participants were satisfied with the intervention method. But in some studies, the patients complained about the complexity of the technology used.[9,12] Furthermore, the authors based on the comments of the patient stated that mutual feedback will increase user loyalty and motivation.[15] On the other hand, the time of intervention had no effect on patient satisfaction, as significant changes were observed in the situation of patients, even in the two-month period intervention.[10] But in the study by Demark-Wahnefried et al.,[45] no significant difference was observed in the first year of the intervention.
Last but not least, because these interventions were used at different stages of the disease, each had a specific purpose for enhancing physical activity. In some patients, the intervention was used mostly to increase arm and shoulder mobility,[25] whereas, in another group, the goal of the intervention was to lose weight and control or change diet behaviors.[57] According to the results of our review, physical activity intervention has been used in BC patients for various purposes. During the pandemic Covid-19, the use of telecommunications continued, with telephone, Skype, and Whatsapp to communicate and rehabilitate BC patients. The longest rehabilitation period for 16 weeks has been done through Whatsapp video for exercise BC patients.
Given the large number of studies conducted in pre-Covid-19 periods and also proved the effectiveness. The authors recommended that during the Covid-19 pandemic, the direct and routine visits should be suspended due to the special conditions of these patients, and they followed and treated with technological approaches as much as possible. For implementing effective rehabilitation services, health care providers should develop the appropriate online Telerehabilitation programs, which are usable and accessible for all. Like the experience in Chile, Greece, and Italy shows that it is possible to implement Telerehabilitation during the Covid-19 epidemic.
The current systematic review cannot be an up-to-date list of all articles due to the frequent publication of new articles in this field. Since the submission of the article to the journal and its final review, other articles may be published that are not included in our study.
Conclusion
This systematic review was designed to assist the decision-makers, clinicians, and nurses in order to introduce and select effective technology for the rehabilitation of BC patients. The research showed physical activity and exercise especially in the shoulder area is effective in reducing health problems in BC patient. Since it reduces their pain and improves disability. On the other hand, Telerehabilitation systems have shown effectiveness and usability for effective disease management in several studies compared with other interventions such as usual care. Therefore, these technologies can be used to manage pain, diet, physical activities, and quality of life in these patients.
It is important to note that, the different follow-up technologies may be applied in health care according to the condition, location, and available infrastructure. Since the duration and type of the intervention are not the same, it cannot be said which type of intervention was more effective. However, in some studies, patients have expressed that they tended to interact and receive feedback from nurses and other health care providers. In addition, using these technologies in remote areas and cost savings should not be overlooked.
During the Covid-19 pandemic, telehealth allows timely access to cancer care. But this requires establishing the appropriate infrastructures and prerequisites and also adequate training should be provided for both patients and health providers. Government should adopt laws to protect the information confidentiality and privacy issues regarding the use of these systems.
Financial Support and Sponsorship
Nil.
Conflicts of interest
Nothing to declare.
Acknowledgements
Nil.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Musarezaie A, Zargham-Boroujeni A. Quality of life and related factors among the women undergoing mastectomy. Iran J Nurs Midwifery Res. 2015;20:287–91. [PMC free article] [PubMed] [Google Scholar]
- 3.Juvet L, Thune I, Elvsaas IØ, Fors E, Lundgren S, Bertheussen G, et al. The effect of exercise on fatigue and physical functioning in breast cancer patients during and after treatment and at 6 months follow-up: A meta-analysis. Breast. 2017;33:166–77. doi: 10.1016/j.breast.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Dietz JR, Moran MS, Isakoff SJ, Kurtzman SH, Willey SC, Burstein HJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat. 2020;181:487–97. doi: 10.1007/s10549-020-05644-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galiano-Castillo N, Arroyo-Morales M, Lozano-Lozano M, Fernández-Lao C, Martín-Martín L, Del-Moral-Ávila R, et al. Effect of an Internet-based telehealth system on functional capacity and cognition in breast cancer survivors: A secondary analysis of a randomized controlled trial. Support Care Cancer. 2017;25:3551–9. doi: 10.1007/s00520-017-3782-9. [DOI] [PubMed] [Google Scholar]
- 6.Grazioli E, Cerulli C, Dimauro I, Moretti E, Murri A, Parisi A. New strategy of home-based exercise during pandemic COVID-19 in breast cancer patients: A case study. Sustainability. 2020;12:6940. [Google Scholar]
- 7.Vallance JK, Nguyen NH, Moore MM, Reeves MM, Rosenberg DE, Boyle T, et al. Effects of the ACTIVity and TEchnology (ACTIVATE) intervention on health-related quality of life and fatigue outcomes in breast cancer survivors. Psychooncology. 2019;29:204–11. doi: 10.1002/pon.5298. [DOI] [PubMed] [Google Scholar]
- 8.Lynch BM, Nguyen NH, Moore MM, Reeves MM, Rosenberg DE, Boyle T, et al. A randomized controlled trial of a wearable technology-based intervention for increasing moderate to vigorous physical activity and reducing sedentary behavior in breast cancer survivors: The ACTIVATE Trial. Cancer. 2019;125:2846–55. doi: 10.1002/cncr.32143. [DOI] [PubMed] [Google Scholar]
- 9.Kokts-Porietis RL, Stone CR, Friedenreich CM, Froese A, McDonough M, McNeil J. Breast cancer survivors' perspectives on a home-based physical activity intervention utilizing wearable technology. Support Care Cancer. 2019;27:2885–92. doi: 10.1007/s00520-018-4581-7. [DOI] [PubMed] [Google Scholar]
- 10.Nápoles AM, Santoyo-Olsson J, Chacón L, Stewart AL, Dixit N, Ortiz C. Feasibility of a mobile phone app and telephone coaching survivorship care planning program among Spanish-speaking breast cancer survivors. JMIR Cancer. 2019;5:e13543. doi: 10.2196/13543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong X, Yi X, Gao D, Gao Z, Huang S, Chao M, et al. The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients: A randomized controlled trial. Health Qual Life Outcomes. 2019;17:109. doi: 10.1186/s12955-019-1183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pope Z, Zeng N, Zhang R, Lee H, Gao Z. Effectiveness of combined smartwatch and social media intervention on breast Cancer survivor health outcomes: A 10-week pilot randomized trial. J Clin Med. 2018;7:140. doi: 10.3390/jcm7060140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lozano-Lozano M, Martín-Martín L, Galiano-Castillo N, Álvarez-Salvago F, Cantarero-Villanueva I, Fernández-Lao C, et al. Integral strategy to supportive care in breast cancer survivors through occupational therapy and a m-health system: Design of a randomized clinical trial. BMC Med Inform Decis Mak. 2016;16:1–10. doi: 10.1186/s12911-016-0394-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson AS, Dunlop J, Gallant S, Macleod M, Miedzybrodzka Z, Mutrie N, et al. Feasibility study to assess the impact of a lifestyle intervention ('LivingWELL') in people having an assessment of their family history of colorectal or breast cancer. BMJ Open. 2018;8:e019410. doi: 10.1136/bmjopen-2017-019410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee H, Uhm KE, Cheong IY, Yoo JS, Chung SH, Park YH, et al. Patient satisfaction with mobile health (mHealth) application for exercise intervention in breast cancer survivors. J Med Syst. 2018;42:254. doi: 10.1007/s10916-018-1096-1. [DOI] [PubMed] [Google Scholar]
- 16.Van De Wiel H, Stuiver M, May A, Van Grinsven S, Aaronson N, Retèl V, et al. (Cost-) effectiveness of an internet-based physical activity support program (with and without physiotherapy counselling) on physical activity levels of breast and prostate cancer survivors: Design of the PABLO trial. BMC Cancer. 2018;18:1073. doi: 10.1186/s12885-018-4927-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayes S, Rye S, Battistutta D, Yates P, Pyke C, Bashford J, et al. Design and implementation of the Exercise for Health trial—A pragmatic exercise intervention for women with breast cancer. Contemp Clin Trials. 2011;32:577–85. doi: 10.1016/j.cct.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 18.Uhm KE, Yoo JS, Chung SH, Lee JD, Lee I, Kim JI, et al. Effects of exercise intervention in breast cancer patients: Is mobile health (mHealth) with pedometer more effective than conventional program using brochure? Breast Cancer Res Treat. 2017;161:443–52. doi: 10.1007/s10549-016-4065-8. [DOI] [PubMed] [Google Scholar]
- 19.Lahart IM, Carmichael AR, Nevill AM, Kitas GD, Metsios GS. The effects of a home-based physical activity intervention on cardiorespiratory fitness in breast cancer survivors; A randomised controlled trial. J Sports Sci. 2018;36:1077–86. doi: 10.1080/02640414.2017.1356025. [DOI] [PubMed] [Google Scholar]
- 20.Hartman SJ, Nelson SH, Myers E, Natarajan L, Sears DD, Palmer BW, et al. Randomized controlled trial of increasing physical activity on objectively measured and self-reported cognitive functioning among breast cancer survivors: The memory and motion study. Cancer. 2018;124:192–202. doi: 10.1002/cncr.30987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krebs P, Shtaynberger J, McCabe M, Iocolano M, Williams K, Shuk E, et al. An eHealth intervention to increase physical activity and healthy eating in older adult cancer survivors: Summative evaluation results. JMIR Cancer. 2017;3:e4. doi: 10.2196/cancer.6435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valle CG, Deal AM, Tate DF. Preventing weight gain in African American breast cancer survivors using smart scales and activity trackers: A randomized controlled pilot study. J Cancer Surviv. 2017;11:133–48. doi: 10.1007/s11764-016-0571-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cox M, Basen-Engquist K, Carmack CL, Blalock J, Li Y, Murray J, et al. Comparison of internet and telephone interventions for weight loss among cancer survivors: Randomized controlled trial and feasibility study. JMIR Cancer. 2017;3:e16. doi: 10.2196/cancer.7166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawler S, Maher G, Brennan M, Goode A, Reeves M, Eakin E. Get Healthy after Breast Cancer-examining the feasibility, acceptability and outcomes of referring breast cancer survivors to a general population telephone-delivered program targeting physical activity, healthy diet and weight loss. Support Care Cancer. 2017;25:1953–62. doi: 10.1007/s00520-017-3599-6. [DOI] [PubMed] [Google Scholar]
- 25.Harder H, Holroyd P, Burkinshaw L, Watten P, Zammit C, Harris PR, et al. A user-centred approach to developing bWell, a mobile app for arm and shoulder exercises after breast cancer treatment. J Cancer Surviv. 2017;11:732–42. doi: 10.1007/s11764-017-0630-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fazzino TL, Fabian C, Befort CA. Change in physical activity during a weight management intervention for breast cancer survivors: Association with weight outcomes. Obesity (Silver Spring) 2017;25(Suppl 2):S109–15. doi: 10.1002/oby.22007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ritvo P, Obadia M, Santa Mina D, Alibhai S, Sabiston C, Oh P, et al. Smartphone-enabled health coaching intervention (iMOVE) to promote long-term maintenance of physical activity in breast cancer survivors: Protocol for a feasibility pilot randomized controlled trial. JMIR Res Protoc. 2017;6:e165. doi: 10.2196/resprot.6615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ollero J, Moral-Munoz JA, Rojas I, Banos O, editors. Mobile Health System for Evaluation of Breast Cancer Patients during Treatment and Recovery Phases. International Conference on Bioinformatics and Biomedical Engineering. Springer. 2017 [Google Scholar]
- 29.Ariza-Garcia A, Lozano-Lozano M, Galiano-Castillo N, Postigo-Martin P, Arroyo-Morales M, Cantarero-Villanueva I. A web-based exercise system (e-cuidatechemo) to counter the side effects of chemotherapy in patients with breast cancer: Randomized controlled trial. J Med Internet Res. 2019;21:e14418. doi: 10.2196/14418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reeves MM, Terranova CO, Erickson JM, Job JR, Brookes DS, McCarthy N, et al. Living well after breast cancer randomized controlled trial protocol: Evaluating a telephone-delivered weight loss intervention versus usual care in women following treatment for breast cancer. BMC Cancer. 2016;16:830. doi: 10.1186/s12885-016-2858-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quintiliani LM, Mann DM, Puputti M, Quinn E, Bowen DJ. Pilot and feasibility test of a mobile health-supported behavioral counseling intervention for weight management among breast cancer survivors. JMIR Cancer. 2016;2:e4. doi: 10.2196/cancer.5305. [DOI] [PubMed] [Google Scholar]
- 32.Cadmus-Bertram L, Nelson SH, Hartman S, Patterson RE, Parker BA, Pierce JP. Randomized trial of a phone-and web-based weight loss program for women at elevated breast cancer risk: The HELP study. J Behav Med. 2016;39:551–9. doi: 10.1007/s10865-016-9735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harrigan M, Cartmel B, Loftfield E, Sanft T, Chagpar AB, Zhou Y, et al. Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: The lifestyle, exercise, and nutrition (LEAN) study. J Clin Oncol. 2016;34:669–76. doi: 10.1200/JCO.2015.61.6375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyons EJ, Baranowski T, Basen-Engquist KM, Lewis ZH, Swartz MC, Jennings K, et al. Testing the effects of narrative and play on physical activity among breast cancer survivors using mobile apps: Study protocol for a randomized controlled trial. BMC Cancer. 2016;16:202. doi: 10.1186/s12885-016-2244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forbes CC, Blanchard CM, Mummery WK, Courneya KS. Feasibility and preliminary efficacy of an online intervention to increase physical activity in Nova Scotian cancer survivors: A randomized controlled trial. JMIR Cancer. 2015;1:e12. doi: 10.2196/cancer.4586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCarroll ML, Armbruster S, Pohle-Krauza RJ, Lyzen AM, Min S, Nash DW, et al. Feasibility of a lifestyle intervention for overweight/obese endometrial and breast cancer survivors using an interactive mobile application. Gynecol Oncol. 2015;137:508–15. doi: 10.1016/j.ygyno.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 37.Lee MK, Yun YH, Park H-A, Lee ES, Jung KH, Noh D-Y. A Web-based self-management exercise and diet intervention for breast cancer survivors: Pilot randomized controlled trial. Int J Nurs Stud. 2014;51:1557–67. doi: 10.1016/j.ijnurstu.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 38.De Cocker K, Charlier C, Van Hoof E, Pauwels E, Lechner L, Bourgois J, et al. Development and usability of a computer-tailored pedometer-based physical activity advice for breast cancer survivors. Eur J Cancer Care (Engl) 2015;24:673–82. doi: 10.1111/ecc.12225. [DOI] [PubMed] [Google Scholar]
- 39.Short C, James E, Rebar A, Duncan M, Courneya K, Plotnikoff R, et al. Designing more engaging computer-tailored physical activity behaviour change interventions for breast cancer survivors: Lessons from the iMove More for Life study. Support Care Cancer. 2017;25:3569–85. doi: 10.1007/s00520-017-3786-5. [DOI] [PubMed] [Google Scholar]
- 40.Winger JG, Mosher CE, Rand KL, Morey MC, Snyder DC, Demark-Wahnefried W. Diet and exercise intervention adherence and health-related outcomes among older long-term breast, prostate, and colorectal cancer survivors. Ann Behav Med. 2014;48:235–45. doi: 10.1007/s12160-014-9598-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rock CL, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA, Wolin KY, et al. Exercise and Nutrition to Enhance Recovery and Good Health for You (ENERGY) Trial Group. Reducing breast cancer recurrence with weight loss, a vanguard trial: The Exercise and Nutrition to Enhance Recovery and Good Health for You (ENERGY) Trial. Contemp Clin Trials. 2013;34:282–95. doi: 10.1016/j.cct.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rock CL, Flatt SW, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA, et al. Results of the Exercise and Nutrition to Enhance Recovery and Good Health for You (ENERGY) trial: A behavioral weight loss intervention in overweight or obese breast cancer survivors. J Clin Oncol. 2015;33:3169–76. doi: 10.1200/JCO.2015.61.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hatchett A, Hallam JS, Ford MA. Evaluation of a social cognitive theory-based email intervention designed to influence the physical activity of survivors of breast cancer. Psychooncology. 2013;22:829–36. doi: 10.1002/pon.3082. [DOI] [PubMed] [Google Scholar]
- 44.Ligibel JA, Meyerhardt J, Pierce JP, Najita J, Shockro L, Campbell N, et al. Impact of a telephone-based physical activity intervention upon exercise behaviors and fitness in cancer survivors enrolled in a cooperative group setting. Breast Cancer Res Treat. 2012;132:205–13. doi: 10.1007/s10549-011-1882-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Demark-Wahnefried W, Morey MC, Sloane R, Snyder DC, Miller PE, Hartman TJ, et al. Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. J Clin Oncol. 2012;30:2354–61. doi: 10.1200/JCO.2011.40.0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eakin EG, Lawler SP, Winkler EA, Hayes SC. A randomized trial of a telephone-delivered exercise intervention for non-urban dwelling women newly diagnosed with breast cancer: Exercise for health. Ann Behav Med. 2012;43:229–38. doi: 10.1007/s12160-011-9324-7. [DOI] [PubMed] [Google Scholar]
- 47.Kim SH, Shin MS, Lee ES, Ro JS, Kang HS, Kim SW, et al., editors. Randomized pilot test of a simultaneous stage-matched exercise and diet intervention for breast cancer survivors. Oncology nursing forum. 2011 doi: 10.1188/11.ONF.E97-E106. Oncology Nursing Society. 2011. [DOI] [PubMed] [Google Scholar]
- 48.Hegel MT, Lyons KD, Hull JG, Kaufman P, Urquhart L, Li Z, et al. Feasibility study of a randomized controlled trial of a telephone-delivered problem-solving–occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psychooncology. 2011;20:1092–101. doi: 10.1002/pon.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morey MC, Snyder DC, Sloane R, Cohen HJ, Peterson B, Hartman TJ, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: A randomized controlled trial. JAMA. 2009;301:1883–91. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pinto BM, Stein K, Dunsiger S. Peers promoting physical activity among breast cancer survivors: A randomized controlled trial. Health Psychol. 2015;34:463–72. doi: 10.1037/hea0000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matthews CE, Wilcox S, Hanby CL, Der Ananian C, Heiney SP, Gebretsadik T, et al. Evaluation of a 12-week home-based walking intervention for breast cancer survivors. Support Care Cancer. 2007;15:203–11. doi: 10.1007/s00520-006-0122-x. [DOI] [PubMed] [Google Scholar]
- 52.Vallance JK, Courneya KS, Plotnikoff RC, Yasui Y, Mackey JR. Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. J Clin Oncol. 2007;25:2352–9. doi: 10.1200/JCO.2006.07.9988. [DOI] [PubMed] [Google Scholar]
- 53.Mella-Abarca W, Barraza-Sánchez V, Ramírez-Parada K. Telerehabilitation for people with breast cancer through the COVID-19 pandemic in Chile. Ecancermedicalscience. 2020;14:1085. doi: 10.3332/ecancer.2020.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lytras D, Myrogiannis IS. The application of complete decongestive therapy through telephysiotherapy in the treatment of acute upper limb lymphedema after mastectomy during the COVID-19 pandemic: A case study. Phys Ther Rehabil. 2020;7:9. doi: 10.7243/2055-2386-7-9. [Google Scholar]
- 55.Ritvo P, Obadia M, Santa Mina D, Alibhai S, Sabiston C, Oh P, et al. Smartphone-enabled health coaching intervention (iMOVE) to promote long-term maintenance of physical activity in breast cancer survivors: Protocol for a feasibility pilot randomized controlled trial. JMIR Res Protoc. 2017;6:e165. doi: 10.2196/resprot.6615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haberlin C, O'Dwyer T, Mockler D, Moran J, O'Donnell DM, Broderick J. The use of eHealth to promote physical activity in cancer survivors: A systematic review. Support Care Cancer. 2018;26:3323–36. doi: 10.1007/s00520-018-4305-z. [DOI] [PubMed] [Google Scholar]
- 57.Lozano-Lozano M, Galiano-Castillo N, Martín-Martín L, Pace-Bedetti N, Fernández-Lao C, Arroyo-Morales M, et al. Monitoring energy balance in breast cancer survivors using a mobile app: Reliability study. JMIR mHealth uHealth. 2018;6:e67. doi: 10.2196/mhealth.9669. [DOI] [PMC free article] [PubMed] [Google Scholar]