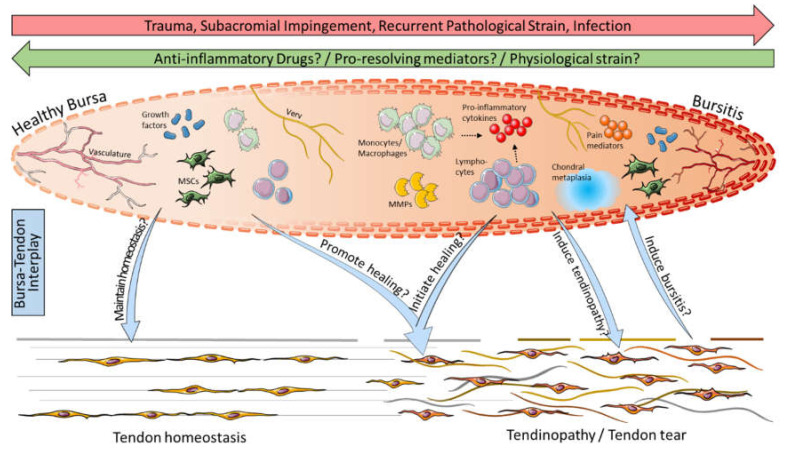
Figure 4.
Possible bursa–tendon interaction: Inflammation through trauma, impingement, recurrent pathological strain, or infection leads to the development of bursitis, whereas bursitis might be cured by anti-inflammatory drugs, pro-resolving mediators, and/or physiological strain. Bursitis is characterized in particular by the presence of immune cells such as monocytes/macrophages and lymphocytes (NK cells, B cells, and T cells), pro-inflammatory cytokines (e.g., SDF-1, IL-1β, and TNF-α), matrix metalloproteinases (MMPs), pain mediators (e.g., COX-2, NGF, and substance P), and chondral metaplasia. Compared to that, healthy bursae contain lower numbers of immune cells and predominate by growth factors and mesenchymal stem cells (MSCs) and, thus, might maintain tendon homeostasis. In bursa–tendon interplay it is hypothesized that growth factors and MSCs in the bursa can promote the healing of tendinopathies, including rotator cuff tears, and it has to be elucidated if pro-inflammatory cells and mediators might help to initiate healing cascades at the tendon rupture side. Vice versa, it is still debatable if bursitis is the cause or consequence of pathological conditions in the tendon. This graphic was created with images from Servier Medical Art.