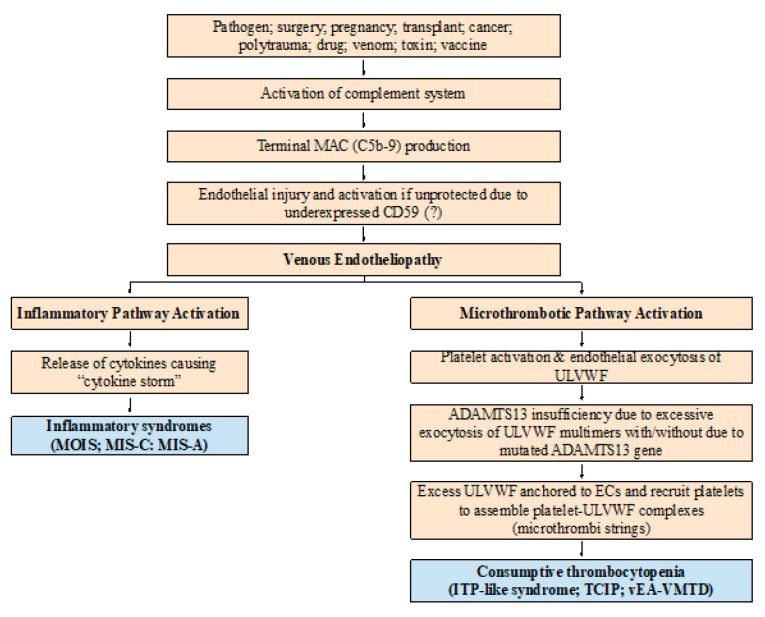
Figure 2.
Pathogenesis of vEA-VMTD. The pathogenesis of endotheliopathy is established based on the “two-activation theory of the endothelium” and is self-explanatory. In the venous system, the molecular responses triggering exocytosis of ULVWF multimers and FVIII and release of cytokines in endotheliopathy are expected to be the same to arterial system. However, the physiological effects between venous and arterial circulation are very different in their shear stress force, vascular directional flow and role of oxygen delivery as noted in the text. Thus, the clinical phenotype of aEA-VMTD is typically TTP-like syndrome and MODS with consumptive thrombocytopenia, which is clinically serious, but that of vEA-VMTD is “silent” ITP with consumptive thrombocytopenia. In severe sepsis, TTP-like syndrome implies sepsis is complicated by overt “arterial” microthrombosis”, but in mild sepsis, ITP-like syndrome suggests transient “venous” microthrombosis has had occurred and perhaps is continuously being resolved by ADAMTS13. This difference has a very important implication in the understanding of combined micro-macrothrombotic syndromes between gangrene-producing arterial combined micro-macrothrombosis and VTE-producing venous combined micro-macrothrombosis. Abbreviations: vEA-VMTD, venous endotheliopathy associated vascular microthrombotic disease; aEA-VMTD, arterial EA-VMTD; ITP, immune thrombocytopenic purpura; MAC, membrane attack complex; MIS-A, multisystem inflammatory syndrome in adults; MIS-C, multisystem inflammatory syndrome in children; MOIS, multiorgan inflammatory syndrome; TCIP, thrombocytopenia in critically ill patients; TTP, thrombotic thrombocytopenic purpura; ULVWF, ultra large von Willebrand factor.