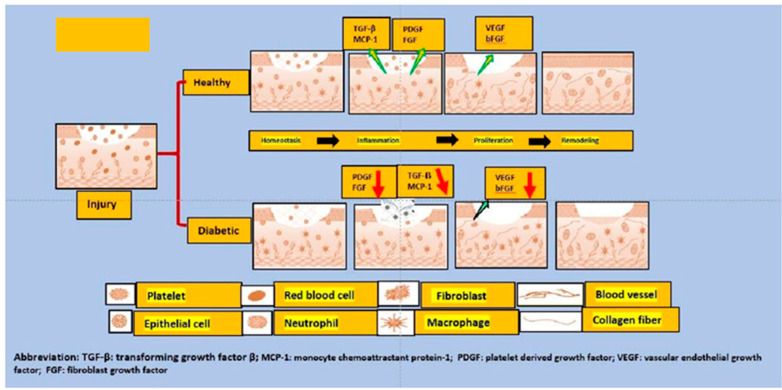
Figure 1.
This figure depicts the differences between the normal and diabetic wound healing phases. When an injury occurs, the formation of various growth factors and cytokines such as transforming growth factor (TGF-) and monocyte chemoattractant protein 1 (MCP-1) from aggregated platelets begins. This is required for the formation of new tissue in the first stage. As a result, growth factors, keratinocytes, and activated fibroblasts start to form a new extracellular matrix and new blood vessels. Reduced levels of all growth factors and cytokines (such as TGF-), MCP-1, and growth and angiogenic factors (VEGF and PDGF) are major contributors to diabetic foot ulcer refractoriness. In short, wound closure is severely impaired in diabetic foot ulcer patients; additionally, reduced angiogenesis is observed due to the hyperglycemic phase, decreased migration of keratinocytes and fibroblasts, resulting in a deficient re-epithelialization; similarly, poor production of the extracellular matrix by fibroblasts contributes to the problem of deficient wound closure.