Abstract
Objectives
The aim of this study was to better understand parental trust in and satisfaction with information sources and medical providers regarding decision making about childhood vaccines.
Setting
The study was part of a Swiss national research programme investigating vaccine hesitancy and underimmunisation.
Participants
We conducted qualitative interviews with 37 providers and 30 parents, observed 34 vaccination consultations, and then conducted quantitative surveys with 130 providers (both complementary and alternative medicine (CAM) oriented and biomedically oriented) and 1390 parents.
Main outcome measures
Participants’ vaccination information sources used in their decision-making process, parents’ trust in and satisfaction with these sources and providers.
Results
Based on the Parent Attitudes about Childhood Vaccines scale, we considered 501 parents as vaccine-hesitant (VH) and 889 parents as non-VH. Whereas both groups mentioned providers as the most trusted source of information, VH-parents were less likely to mention paediatricians (N=358 (71%) vs N=755 (85%)) and public health authorities (N=101 (20%) vs N=333 (37%)) than non-VH-parents. VH-parents were more likely to have consulted another provider (N=196 (39%) vs N=173 (19%)) than non-VH-parents, to express less satisfaction with both their primary (N=342 (82%) vs N=586 (91%)) and other providers (N=82 (42%) vs N=142 (82%)) and less trust in their primary (N=368 (88%) vs N=632 (98%)) and other providers (N=108 (55%) vs N=146 (84%)). VH-parents were less likely to be satisfied with their biomedical primary provider than non-VH-parents (100 (69%) vs 467 (91%)). However, when the primary provider was CAM-oriented, there were similar levels of satisfaction among both groups (237 (89%) VH-parents vs 118 (89%) non-VH-parents). All differences were significant (p<0.05).
Conclusions
While the provider remains the main information source, VH parents turn to additional sources and providers, which is likely related to VH parents being rather dissatisfied with and distrusting in obtained information and their provider.
Ethics
The local ethics committee (Ethikkommission Nordwest- und Zentralschweiz, EKNZ; project ID number 2017-00725) approved the study.
Keywords: public health, medical ethics, paediatric infectious disease & immunisation, epidemiology
Strengths and limitations of this study.
The mixed-methods design brought added value to our study, as this allowed us to address qualitatively documented phenomena and then systematically analyse them on a larger scale.
Our recruitment strategy explicitly oversampled complementary and alternative medicine (CAM) oriented providers and parents consulting them, which allowed us to compare the patient–provider relationship and patient–provider vaccine perspectives for parents seeing CAM versus biomedical providers.
We consider the transdisciplinary research to be a distinct advantage.
The quantitative survey was not administered to a random sample.
Our provider sample was recruited through personal contacts and snowball sampling.
Introduction
The growing body of literature on vaccine hesitancy (VH) points to the multifaceted and complex nature of vaccination decision making.1 2 Most parents—whether vaccine accepting or VH—obtain their vaccine information primarily from healthcare professionals, with the most cited source being paediatricians, followed by other healthcare professionals, such as midwives, nurses and other therapists.3–5 As healthcare providers are the main source of information for parental decision making, issues around satisfaction with and trust in the provider are important to understand. Previous research has shown how trusting relationships between patients and providers are determinative in parents’ vaccination decision making, meaning that parents who trust their providers tend to trust their vaccination recommendations.6–8 In Switzerland, complementary and alternative medicine (CAM) is widely used and integrated into the healthcare system.9 10 Particularly in primary healthcare for children, CAM is mainly provided by biomedically trained physicians with additional CAM training in the sense of integrative medicine.11 Researchers have established associations between VH and CAM use,6 12 13 and suggested that CAM providers and VH parents have a ‘symbiotic’ relationship, meaning that ‘VH and CAM exist and function separately, but when combined, provide each other with ‘resources’ that enable them to thrive together’(p 111).12 Others have shown that VH individuals have lower levels of trust in biomedicine than in CAM.12 14
In addition to medical providers, sources of vaccination information include parents’ social networks, with similar views and norms being shared within networks. Generally, parents with people in their networks who vaccinate less are also less likely to vaccinate.15 16 Social media and the internet offer platforms for disseminating information and thus serve as popular vaccination information sources with its own complexities and dynamics.17–19 Testimonies of (negative) experiences during and after vaccination or the usage of forums are believed to be particularly appealing to parents seeking vaccination information.20 21 In the last two decades, patient–provider dynamics have partially changed from the former doctor-provides-patient to today’s users-provide-users (ie, patients no longer obtain their information only from the doctors who treat them, but doctors as well as lay people frequently disseminate information about health and illness on the internet, which is available to all other users), with health-information seeking audiences being potentially far larger, and everyone with internet access being capable of disseminating information.20 22 This context is further complicated with negative, emotion-focused and often untrue vaccination information being difficult to debunk with medical facts.21
Research consistently shows how trust in and satisfaction with providers who promote vaccination increases parental vaccine acceptance, while parents being misunderstood, criticised or alienated when expressing VH in clinical interactions can have a negative impact on vaccination acceptance.8 Ceasing to consult with a healthcare provider23 24 and, related, the phenomenon of doctor ‘shopping’ (which we refer to as browsing),25 have previously been described as important expressions of patient dissatisfaction. Some of our qualitative data analysis has particularly demonstrated how issues of trust, satisfaction, affect and choice played determinative roles, not only in parents’ vaccination decisions, but also in the types of vaccination sources and the choices of healthcare practitioners (ie, biomedical or CAM) with whom they consult for their children’s cares.24 The nuances of CAM vaccination counselling resulting in higher trust and satisfaction most likely lie within these providers taking time for discussion, incorporating parents into decision making and taking parents’ concerns seriously.26
In this mixed-methods study, we examined the extent to which trust in and satisfaction with vaccination information sources, and in particular, the healthcare provider as the main source of information, differs between VH and non-VH parents and how this affects the parental vaccination decision making.
Material and methods
Study design and population
This study is part of a transdisciplinary national research program (NRP74) into vaccination decision making in Switzerland.27 We employed a mixed-methods approach with sequential exploratory design, meaning that an initial qualitative component informed the design of a subsequent quantitative stage.28 First, we analysed the qualitative results by identifying key areas that seemed to be of central importance. We then focused on these when compiling the quantitative questionnaires. The detailed analysis of qualitative and quantitative results was finally done in parallel by presenting a clustering of similar statements in the qualitative sector, followed by quantitative results showing similar dynamics on a larger scale. We interviewed parents throughout German, French and Italian-speaking Switzerland. The French-speaking part, with approximately 23% of the Swiss population and about 19% of our parental study sample, was slightly under-represented, and the Italian part was slightly over-represented (8% of the Swiss population and 18% of study parents).29 30 At the time of the survey, the interviewed parent was >18 years of age and their child was 0–11 years old. We asked parents to provide us with a copy of their children’s vaccination record.
Patient and public involvement
Given the presumably large number of people who are not to be regarded as vaccine opponents but as vaccine hesitant, we meant to employ a specific focus on the path to decision making with all the thought processes, worries and fears contained therein, as well as the influence of external information. During our qualitative research period, various starting points emerged that were worth investigating on a larger scale (in the quantitative sector). We recruited participating parents from a network of 86 biomedical and 44 CAM providers participating in the project. Participants who indicated they wished to receive the study results will receive notifications once results are published.
Qualitative data collection and analysis
We first conducted semistructured in-depth interviews with parents from September 2017 to February 2018 and with biomedically only trained doctors and providers (ie, physicians or non-physician providers) with additional CAM training from August 2017 to September 2018. Interviews aimed to better understand parents’ vaccination decision-making processes and their interactions with healthcare providers. An interview guide was piloted and revisited iteratively for clarity. We also conducted ethnographic observations of vaccination consultations. Qualitative interviews were audiorecorded and transcribed verbatim. Online supplemental questionnaires S1 and S2 contain the interview guides for the qualitative parental and provider interviews, respectively. Interviews allowed us to gather background information about parents and their providers and perspectives on vaccination. Vaccination consultation observations were documented in field journals and then subsequently written into narrative accounts. Qualitative data were analysed by MD and AB. Analysis of the qualitative interviews and observations were guided by the Framework Method31 with support of MAXQDA software.
bmjopen-2021-053267supp001.pdf (85.8KB, pdf)
bmjopen-2021-053267supp002.pdf (73KB, pdf)
Quantitative data collection and analysis
For the study’s quantitative component, we recruited parents in waiting rooms of participating providers’ offices.27 We refer to these providers as the primary providers. The questionnaire, however, was administered during a telephone interview conducted after office hours from January 2019 to April 2020.27 The latter included the Parent Attitudes about Childhood Vaccines (PACV) survey score, a validated instrument that was designed by Opel et al in order to identify VH parents.32–34 The 2011 Opel-revised 15-item PACV33 results in a score of 0–100 points. If a parent scores ≤49 points, they are considered non-VH; if they score >50 points, they are considered VH. Based on the results of a study validating a five-item version of the PACV in Switzerland with identical scoring,30 we opted for the shorter five-item version for our analyses. The final questionnaire included PACV items, questions gathering sociodemographic information about the parents and the target child, and additional questions informed by our previously published qualitative research investigating CAM provider approaches to vaccination consultations,26 biomedical provider descriptions of interactions with VH parents and dilemmas faced when addressing vaccine hesitancy and refusal,35 and VH parents’ navigation of information sources and consultations with CAM and biomedical providers.24 These qualitative studies informed the design of several components of the quantitative survey, particularly including questions on the parent–provider relationship and vaccination information sources. The quantitative questionnaire is provided in online supplemental questionnaire S3.
bmjopen-2021-053267supp003.pdf (131.5KB, pdf)
A key question posed to parents was ‘What are your most trusted information sources on vaccination?’ to which a series of pre-established response options were made available (eg, ‘internet’). We invited participants to provide additional information through open-answer responses (eg, ‘which websites?’). The number of sources mentioned by each participant was analysed by coding and counting the reported sources, as well as the free-text answers.
We use descriptive statistics plus Pearson’s χ2 and Wilcoxon rank-sum tests to test whether observed differences between non-VH and VH parent participants are significant at the p<0.05 level. Quantitative data analysis was performed by SE and KJ using STATA software V.12.1 (Stata). We personally reviewed the information sources cited by parents and, after consultation within the team, we decided whether to consider each source as critical or accepting of the official vaccination recommendations.
Results
Study population
For the qualitative study component, we conducted ethnographic observations of 34 paediatric vaccination consultations. We also conducted in-depth, face-to-face interviews with 30 parents and 37 providers. Among the provider interviewees, 20 were biomedically oriented physicians and 17 were CAM-oriented providers, of which 15 were biomedically trained physicians with additional training in CAM, and 2 were non-physician CAM providers.
For the research programme’s quantitative component, (ie, both the childhood vaccines and HPV samples27), we completed a full telephone interview with 1390 parents and 130 (86 biomedically and 44 CAM oriented) primary providers. A total of 889 (64%) parents had a PACV score of ≤49, indicating non-VH, and 501 (36%) parents had a PACV score of ≥50, indicating VH. Parent characteristics are shown in table 1. VH parents were more likely to see a CAM-oriented primary provider than non-VH parents (307 (61%) vs 183 (21%); p<0.001).
Table 1.
Characteristics of the quantitative study population
| All parents (N=1390) | By PACV score | P value | |||||
| Non-VH parents (N=889) | VH parents (N=501) | ||||||
| N (%) | N (%) | N (%) | |||||
| Female respondent | 1232 | (89%) | 798 | (90) | 434 | (87) | 0.141* |
| Relationship to child | 0.095* | ||||||
| Mother | 1228 | (88) | 797 | (90) | 431 | (86) | |
| Father | 155 | (11) | 89 | (10) | 66 | (13) | |
| Other | 7 | (1) | 3 | (0) | 4 | (1) | |
| Interviewee age (Mean (SD)) | 37.1 | (6.27) | 37 | (6.16) | 37.2 | (6.46) | 0.592† |
| Born in Switzerland | 981 | (71) | 608 | (68) | 373 | (74) | 0.059* |
| Parent’s highest education | <0.001* | ||||||
| Low‡ | 272 | (20) | 188 | (21) | 84 | (17) | |
| Medium§ | 321 | (23) | 209 | (24) | 112 | (22) | |
| Bachelors¶ | 285 | (21) | 163 | (18) | 122 | (24) | |
| Masters | 358 | (26) | 226 | (25) | 132 | (26) | |
| Doctorate | 105 | (8) | 81 | (9) | 24 | (5) | |
| Other, missing | 49 | (4) | 22 | (2) | 27 | (5) | |
| Household income | <0.001* | ||||||
| <CHF80 000 | 319 | (23) | 174 | (20) | 145 | (29) | |
| CHF80 000–CHF120 000 | 384 | (28) | 225 | (25) | 159 | (32) | |
| >CHF120 000 | 279 | (20) | 195 | (22) | 84 | (17) | |
| Missing, declined to respond | 408 | (29) | 295 | (33) | 113 | (23) | |
| Type of primary provider | <0.001* | ||||||
| Biomedical | 893 | (64) | 705 | (79) | 188 | 38 | |
| CAM | 490 | (35) | 183 | (21) | 307 | (61) | |
| Missing | 7 | (1) | 1 | (0) | 6 | (1) | |
*Pearson’s χ2.
†Wilcoxon rank-sum tests were used for statistical analysis.
‡Secondary school not completed, no completed professional education, completed 9 years of school without further education, apprenticeship, technical school or business school.
§College, higher professional school.
¶Bachelor at university, primary school teacher seminar.
CAM, complementary and alternative medicine; PACV, Parent Attitudes about Childhood Vaccines; VH, vaccine hesitant.
Variety of information sources on vaccination
During our qualitative interviews and observations of vaccination consultations, parents cited a broad array of vaccination information sources as part of their decision-making process. Many VH parents engaged in what we refer to as information browsing, which involves parents comparing and weighing different information sources while striving to reach certainty about the right vaccination decision to make for their children. For example, Mrs Sandoz, a 35-year-old mother of a 13-month-old unvaccinated son explained her decision not to vaccinate:
I think it was a mix of discussions with people close to us and with friends. […] There is my personal feeling about the matter. There is certainly the social influence from my husband. I’ll say that the decision surely came more from me than it did from him. I think I hold the decision closer to my heart than he does. I think it was kind of a vague questioning. There were some things I read on the Internet. I joined Facebook groups where they talk about it. I read some testimonies. I think when I was pregnant, I had a discussion with the [CAM] pediatrician in order to know the true risks that we were taking if we didn’t vaccinate. I was looking for the most neutral point of view possible. […] For now, it’s a decision that is in favor of not vaccinating.
Other VH parents explained how having multiple sources of information reassured them that they were taking the correct course of action for their families.
Qualitative results additionally shed light on parents, often VH parents, having consulted a multitude of sources that varied in both format and content. Parents described how each piece of information could temporarily solidify their opinion, but also raise further doubts and uncertainties. Mrs. Sandoz explained:
We have a lot of doubts around the benefits of vaccines. My husband and I are still reading about it and continue to have discussions and thinking about it in order to be comfortable. […]. We have so much information that we can get lost in it. […] Up until now, everything that I’ve read and the discussions that I’ve had have reinforced our decision to not vaccinate our son.
VH parents described how a multitude of information sources could be both a source of reassurance and of hesitancy in their quest for neutral information about vaccination. We therefore investigated the potential association of VH with the number and trustworthiness of parents’ vaccination information sources by including the question ‘What are your most trusted information sources on vaccination?’ in the quantitative questionnaire.
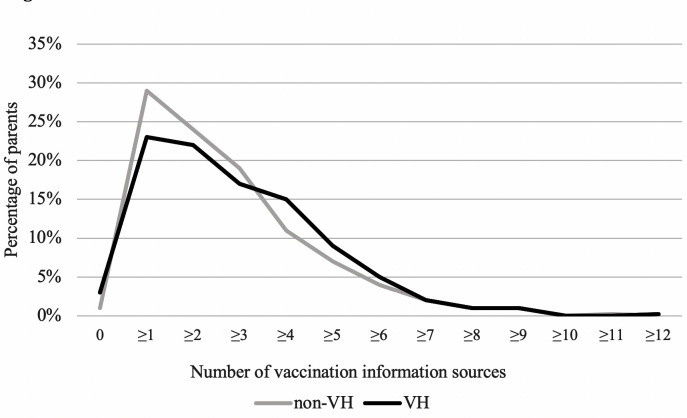
Figure 1 illustrates how the number of trusted information sources varied between VH and non-VH parents. VH parents reported using more sources on average than non-VH parents (2.98 (SD=2.02) vs 2.70 (SD=1.83)). While small, the difference was significant (p=0.012).
Figure 1.
Number of trusted vaccination information sources. Note: distribution of the number of trusted vaccination information sources. We divided parents into non-VH and VH according to PACV score <or >50. The median, mean (SD) of information sources was; 2, 2.80 (1.90) for the entire study population (N=1390); 2, 2.70 (1.83) for the non-VH parents (N=889) and; 3, 2.98 (2.02) for the VH parents (N=501). Wilcoxon rank-sum test was used for statistical analysis. VH, vaccine hesitant.
Types of information sources and media
Based on our initial qualitative research, we generated a preliminary list of information source types which we then included in the quantitative questionnaire. Commonly mentioned information sources included the child’s doctor and other providers, family, friends and acquaintances, official public health recommendations, print media, such as books or newspaper articles, the internet and social media.
In table 2, we list the trusted vaccination information sources cited most by parents. The child’s doctor was the information source cited most (1113 (80%) parents) by both VH and non-VH parents, but VH parents were less likely to report the child’s doctor as the most trusted source than non-VH parents (358 (71%) vs 755 (85%); p<0.001). VH parents were also less likely to report public health authorities as a trusted information source than non-VH parents (101 (20%) vs 333 (37%); p<0.001), as well as information materials that are consistent with the official vaccination recommendation (26 (5%) vs 74 (8%); p=0.03).
Table 2.
Types of trusted vaccination information sources
| All parents (N=1390) | By PACV score | P value | |||||
| Non-VH parents (N=889) | VH parents (N=501) | ||||||
| N (%) | N (%) | N (%) | |||||
| My child’s doctor | 1113 | (80) | 755 | (85) | 358 | (71) | <0.001 |
| Social networks* | 468 | (34) | 253 | (28) | 215 | (43) | <0.001 |
| Public health authorities | 434 | (31) | 333 | (37) | 101 | (20) | <0.001 |
| Other healthcare workers | 224 | (16) | 119 | (13) | 105 | (21) | <0.001 |
| Other physician | 195 | (14) | 111 | (12) | 84 | (17) | 0.027 |
| CAM | 19 | (1) | 3 | (0) | 16 | (3) | <0.001 |
| Homeopathic | 12 | (1) | 2 | (0) | 10 | (2) | 0.001 |
| Midwife | 13 | (1) | 4 | (0) | 9 | (2) | 0.268 |
| Materials that are critical of public health vaccination recommendation† | 109 | (8) | 4 | (0) | 105 | (21) | <0.001 |
| ‘Foundation for consumer protection’ | 22 | (2) | 3 | (0) | 19 | (4) | <0.001 |
| Hirte: ‘Impfen Pro and Contra’ | 15 | (1) | 0 | (0) | 15 | (3) | <0.001 |
| Explicitly CAM materials | 12 | (1) | 0 | (0) | 12 | (2) | <0.001 |
| Berthoud: ‘Qui aime bien vaccine peu’ | 9 | (1) | 0 | (0) | 9 | (2) | <0.001 |
| Glöckler/Goebel/Michael: ‘Kindersprechstunde’ | 6 | (0) | 0 | (0) | 6 | (1) | 0.001 |
| ‘www.impfo.ch’ | 5 | (0) | 2 | (0) | 3 | (1) | 0.264 |
| Materials that are consistent with public health vaccination recommendation† | 100 | (7) | 74 | (8) | 26 | (5) | 0.030 |
| ‘www.swissmom.ch’ | 20 | (1) | 16 | (2) | 4 | (1) | 0.132 |
| ‘Wir Eltern’ | 8 | (1) | 7 | (1) | 1 | (0) | 0.164 |
| ‘Beobachter’ | 6 | (0) | 2 | (0) | 4 | (1) | 0.117 |
| ‘Puls’ | 6 | (0) | 4 | (0) | 2 | (0) | 0.890 |
| 98 | (7) | 78 | (9) | 20 | (4) | 0.001 | |
| Scientific literature§ | 55 | (4) | 37 | (4) | 18 | (4) | 0.601 |
| No source, missing, don't know, don't want to disclose | 49 | (4) | 26 | (3) | 23 | (5) | 0.106 |
| Medical work experience‡ | 42 | (3) | 30 | (3) | 12 | (2) | 0.306 |
| Nurse | 8 | (1) | 6 | (1) | 2 | (0) | 0.514 |
| News | 31 | (2) | 22 | (2) | 9 | (2) | 0.411 |
| Personal experience, gut feeling | 26 | (2) | 10 | (1) | 16 | (3) | 0.006 |
| Described as neutral | 9 | (1) | 0 | (0) | 9 | (2) | <0.001 |
*Family, friends and acquaintances.
†Print media, websites, organisations, television programmes and films that are critical of or consistent with public health vaccination recommendations based on our detailed assessment and on consensus among research team members.
‡Medical, biological or pharmaceutical training or work experience of the interviewee or the other parent of the target child.
§As stated by the interviewee. Pearson’s χ2 tests were used for statistical analysis.
CAM, complementary and alternative medicine; PACV, Parent Attitudes about Childhood Vaccine; VH, vaccine hesitant.
In contrast, VH parents tended to mention information sources other than the child’s doctor or public health authorities more than non-VH parents, including social networks (215 (43%) vs 253 (28%); p<0.001), other healthcare workers (105 (21%) vs 119 (13%); p<0.001) and their personal gut feelings or experiences (16 (3%) vs 10 (1%); p=0.006). The largest difference we identified involved information materials, such as books, online or print magazines and websites that are critical of official vaccination recommendations (105 VH parents (21%) vs 4 non-VH parents (0%); p<0.001), and materials of obvious CAM nature (12 VH parents (2%) vs 0 non-VH parents (0%); p<0.001).
In table 3, we list where parents reported having obtained trusted information about vaccination. We list all information channels reported by at least five parents. The internet was considered the most trustworthy medium by VH parents and non-VH parents in similar proportions (176 (35%) vs 299 (34%); p=0.572). However, VH parents cited print media as their most trusted medium of vaccination information more frequently than non-VH parents (237 (47%) vs 176 (20%); p<0.001), including books and brochures (129 (26%) vs 63 (7%); p<0.001). With regard to specific internet sources, VH parents were less likely to report Google than non-VH parents (20 (4%) vs 78 (9%); p=0.001) as a trusted medium for vaccination information. VH parents were more likely than non-VH parents to cite social media (26 (5%) vs 21 (2%); p=0.005), although overall few parents in either group cited this as a trusted information source.
Table 3.
Types of trusted media for vaccination information
| All parents (N=1390) | By PACV score | P value | |||||
| Non-VH parents (N=889) | VH parents (N=501) | ||||||
| N (%) | N (%) | N (%) | |||||
| Internet | 475 | (34) | 299 | (34) | 176 | (35) | 0.572 |
| 98 | (7) | 78 | (9) | 20 | (4) | 0.001 | |
| Social media | 47 | (3) | 21 | (2) | 26 | (5) | 0.005 |
| 17 | (1) | 7 | (1) | 10 | (2) | 0.490 | |
| Print media | 413 | (30) | 176 | (20) | 237 | (47) | <0.001 |
| Books and brochures | 192 | (14) | 63 | (7) | 129 | (26) | <0.001 |
| Magazine and newspapers | 60 | (4) | 42 | (5) | 18 | (4) | 0.319 |
| Television | 67 | (5) | 37 | (4) | 30 | (6) | 0.127 |
| Films | 13 | (1) | 1 | (0) | 12 | (2) | <0.001 |
| Conferences | 9 | (1) | 2 | (0) | 7 | (1) | 0.150 |
Pearson’s χ2 tests were used for statistical analysis.
Satisfaction with and trust in the primary provider
Our qualitative findings revealed an understudied phenomenon in Switzerland—parents switching providers for their children’s care around the issue of vaccination—and suggested that this switch was often made from biomedical-oriented physicians to those trained in CAM.24 Quantitative results suggest that more VH parents than non-VH parents consulted providers other than the child’s primary provider when making vaccination decisions, as can be seen below. We therefore explored whether this information seeking behaviour is related to issues of (dis)satisfaction with and (dis)trust in the primary provider.
Qualitative evidence particularly showed the saliency of the issue of trust for parents in their vaccination decision-making process. The following except from an interview with Mrs. Godet, a 29-year-old mother of a 13-month-old fully vaccinated daughter illustrates how, despite the mother’s media-induced uncertainty about her vaccination decision, trust in the provider was crucial for her to follow the provider’s recommendation:
There are a lot of so-called ’scientific' studies which have come out with consequences that vaccines might have on children’s health. […]. And so it’s very hard to know who to believe, actually. […]. So, we trust, anyway. Well, I trust my pediatrician. So, if she tells me that I have to vaccinate, I think that’s good. Now, it’s true that if you read a little bit of what’s on the Internet and everything, you don't really know what to do.
Providers also discussed how they fostered trust as part of their clinical practice. Dr. Heffelfinger, an anthroposophic physician, explained how he thought his practices differed from those of a biomedically oriented paediatrician:
I try to take much more time and try to make something out of the time. To gain trust, to create insight to the subject. […]. To me, the free decision to vaccinate is the top priority. The decision belongs to the human being that decides for himself or herself.
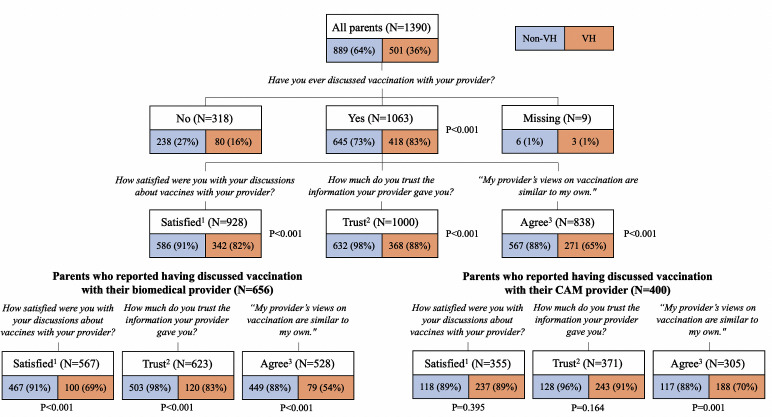
Figure 2 and online supplemental table S1 show how VH parents were more likely to have discussed vaccination with their primary provider than non-VH parents (418 (83%) vs 645 (73%); p<0.001). VH parents were less likely to be satisfied with and to trust their primary provider than non-VH parents (satisfaction: 342 (82%) vs 586 (91%); trust: 368 (88%) vs 632 (98%); p<0.001 for both satisfaction and trust). When their primary provider was biomedically oriented, this difference was even more notable (satisfaction: 100 (69%) vs 467 (91%); trust: 120 (83%) vs 503 (98%); p<0.001 for both satisfaction and trust). In contrast, when the primary provider was CAM-oriented, there was no significant difference in satisfaction and trust for VH and non-VH parents (satisfaction: 237 (89%) vs 118 (89%); trust: 243 (91%) vs 128 (96%); p=0.395 and p=0.164, respectively).
Figure 2.
Parental satisfaction with and trust in the child’s biomedical or CAM primary provider. Note: 1Very satisfied or satisfied; 2Completely or somewhat trust; 3Completely or somewhat agree; Percentages refer to the total number of non-VH and VH parent participants; Pearson’s χ2 tests were used for statistical analysis. CAM, complementary and alternative medicine; VH, vaccine hesitant.
bmjopen-2021-053267supp004.pdf (94.4KB, pdf)
To evaluate issues of (dis)satisfaction and (dis)trust, we analysed parents’ responses regarding perceived agreement between their own vaccination view and their primary provider’s view. VH parents reported significantly lower agreement between their own vaccination view and their child’s doctor perceived view than non-VH parents (271 (65%) vs 567 (88%); p<0.001). The gap between parent and provider views was larger when the primary provider was biomedically oriented (79 (54%) VH parents vs 449 (88%) non-VH parents; p<0.001) and smaller when the primary provider was CAM-oriented (188 (70%) VH parents vs 117 (88%) non-VH parents; p=0.001).
Seeking multiple provider opinions on vaccination
Given the important role children’s doctors play in influencing parents’ vaccination decisions, we further explored a phenomenon that our initial qualitative work brought to light—parents consulting with and/or switching from one to another provider, often to one offering CAM services, in response to issues arising during vaccination consultations,24 a phenomenon we call provider browsing. The following conversation with Mrs. Kugler, a 37-year-old mother of one partially vaccinated child, illustrates this behaviour:
Researcher: Ok. I’ve already seen in the vaccination booklet, there are two or three different doctors that you consult. Do you prefer to see a biomedical provider?
Mother: Well, we actually tend to go to the homeopath. […]. She’s always a little, “I told you so,” after every vaccination. But she tolerates it. It takes her two or three weeks until she gets well enough to be neutral towards us again [laughing]. Because we do vaccinate. And [the homeopath] is the one who treats [our daughter] when she’s sick. […]. And if we needed a diagnosis, for example, if I wasn't sure whether it was otitis media or something like that, I used to go see [the local pediatrician]. […]. He is a classic [biomedical] Algifor-Dafalgan [commonly prescribed pain killers in Switzerland, containing ibuprofen and paracetamol, respectively] doctor.
Researcher: Ok. Purely conventional biomedical?
Mother: Yes, […]. At every diagnosis. In winter, [my daughter] was very sick again with an extremely high temperature. Again, the remedy was Algifor. The doctor added, ‘We should start vaccinating soon. […]. It’s a classic fever. We can easily vaccinate. It’s not too bad at this age.’ […] I felt we were no longer in good hands and switched to Dr. Heffelfinger.
Qualitative analysis of provider browsing suggested that parents were seeking healthcare providers who were willing to listen to and understand parents’ rationales around vaccination and their adherence to complementary and alternative approaches to medicine. Dr. Heffelfinger, an anthroposophical doctor, pointed to the practice of listening to and responding to parents' questions and concerns. He hypothesised why parents might switch to him after seeing a biomedically oriented physician,
That style of consultation doesn’t suit them. […]. The parents don’t feel like they are being taken seriously, or they have many more questions than what they were able to discuss.
When asked if parents followed this provider’s vaccination recommendations, he responded affirmatively, noting that parents did not often return to their previous paediatrician,
People don’t consult that pediatrician again because the pediatrician was vaccinating insanely. [With me], parents do almost exactly the same vaccines as they would have done with their previous pediatrician. But we talked about them.
Table 4 reports quantitative analysis of this phenomenon showing that more VH parents than non-VH parents reported consulting with a provider other than the primary provider for vaccination questions (196 (39%) vs 173 (19%); p<0.001). We specifically asked questions about parents’ motivations for consulting with another provider. More VH parents than non-VH parents cited seeking a second opinion or having a disagreement as the reason for consulting with another provider (87 (17%) vs 38 (4%); p<0.001). Logistical reasons (eg, parents moved or provider stopped working) were mentioned with similar frequency (43 (9%) among VH parents vs 68 (8%) among non-VH parents; p=0.537).
Table 4.
Parents having consulted another doctor about vaccination
| All parents (N=1390) | By PACV score | P value | |||||
| Non-VH parents (N=889) | VH parents (N=501) | ||||||
| N (%) | N (%) | N (%) | |||||
| Consulted another doctor | <0.001 | ||||||
| No | 1012 | (73) | 712 | (80) | 300 | (60) | |
| Yes | 369 | (27) | 173 | (19) | 196 | (39) | |
| Missing | 9 | (1) | 4 | (0) | 5 | (1) | |
| Reason for consultation | <0.001 | ||||||
| Second opinion or disagreement | 125 | (9) | 38 | (4) | 87 | (17) | |
| Moved or stopped working | 111 | (8) | 68 | (8) | 43 | (9) | |
| Other | 130 | (9) | 64 | (7) | 66 | (13) | |
| Missing | 3 | (0) | 3 | (0) | 0 | (0) | |
| Parents with a biomedical primary doctor | Total sample (N=893) | By PACV score | |||||
| Non-VH parents (N=705) | VH parents (N=188) | ||||||
| N (%) | N (%) | N (%) | P value | ||||
| Consulted another doctor | 0.002 | ||||||
| No | 703 | (79) | 572 | (81) | 131 | (70) | |
| Yes | 183 | (20) | 129 | (18) | 54 | (29) | |
| Missing | 7 | (1) | 4 | (1) | 3 | (2) | |
| Reason for consultation | 0.134 | ||||||
| Second opinion or disagreement | 46 | (5) | 27 | (4) | 19 | (10) | |
| Moved or stopped working | 71 | (8) | 55 | (8) | 16 | (9) | |
| Other | 64 | (7) | 45 | (6) | 19 | (10) | |
| Missing | 2 | (0) | 2 | (0) | 0 | (0) | |
| Parents with a CAM primary doctor | Total sample (N=490) | By PACV score | |||||
| Non-VH parents (N=183) | VH parents (N=307) | ||||||
| N (%) | N (%) | N (%) | P value | ||||
| Consulted another doctor | <0.001 | ||||||
| No | 308 | (63) | 140 | (77) | 168 | (55) | |
| Yes | 180 | (37) | 43 | (23) | 137 | (45) | |
| Missing | 2 | (0) | 0 | (0) | 2 | (1) | |
| Reason for consultation | 0.014 | ||||||
| Second opinion or disagreement | 75 | (15) | 10 | (5) | 65 | (21) | |
| Moved or stopped working | 40 | (8) | 13 | (7) | 27 | (9) | |
| Other | 64 | (13) | 19 | (10) | 45 | (15) | |
| Missing | 1 | (0) | 1 | (1) | 0 | (0) | |
| All parents having consulted another doctor before | Total sample (N=369) | By PACV score | |||||
| Non-VH parents (N=173) | VH parents (N=196) | ||||||
| N (%) | N (%) | N (%) | P value | ||||
| Satisfied with other doctor* | 224 | (61) | 142 | (82) | 82 | (42) | <0.001 |
| Trust other doctor† | 254 | (69) | 146 | (84) | 108 | (55) | <0.001 |
Pearson’s χ2 tests were used for statistical analysis.
*Satisfied or very satisfied.
†Somewhat or completely.
CAM, complementary and alternative medicine; PACV, Parent Attitudes about Childhood Vaccine; VH, vaccine hesitant.
Interestingly, among parents who had asked another provider about vaccination, about half as many VH parents as non-VH parents reported satisfaction with and trust in the other provider (satisfaction: 82 (42%) vs 142 (82%); trust: 108 (55%) vs 146 (84%); p<0.001 for both satisfaction and trust).
Since VH parents report higher satisfaction and trust in CAM-oriented providers, we investigated whether provider browsing varied by type of primary provider (ie, biomedical or CAM orientation). Among parents with biomedically oriented primary providers, more VH parents than non-VH parents engaged in provider browsing (54 (29%) vs 129 (18%); p=0.002). However, this difference was even starker among parents with CAM-oriented primary providers (137 (45%) of VH parents vs 43 (23%) of non-VH parents; p<0.001).
Discussion
Principal findings
Our mixed-methods study has several main findings. First, our results confirm previous research showing that children’s doctors are parents’ most important vaccination information.3–5 36 Similarly, VH participants were more likely to turn to additional information sources, including their social networks, books, and other materials critical of official vaccination recommendations.4 15 16 More VH parents than non-VH parents cited print media as a trusted information source. To our knowledge, this has not been reported on previously.
Second, VH parents expressed lower levels of satisfaction with and trust in their primary provider, particularly biomedically oriented physicians. This finding is likely associated with our third main finding showing that VH parents engaged more in provider browsing than non-VH parents. Nevertheless, VH parents reported lower levels of satisfaction with and trust in these other providers. VH parents were more likely to consult with CAM-oriented primary providers and to have higher levels of satisfaction with and trust in CAM than in biomedical providers. Interestingly, the phenomenon of VH parents having consulted with other providers about vaccination occurred more when the primary provider was CAM oriented.
Previous research suggests that the relationship between VH and CAM use is not fully explained by VH individuals’ trust in CAM services, but rather by distrust in biomedicine.14 Accordingly, we argue that the VH parents in our sample may have been more likely to be pushed away from biomedicine than pulled toward CAM, as VH parents seemed to switch providers when they were no longer satisfied with or no longer fully trusted their provider, therefore substantiating not necessarily the attractiveness of the second provider, but rather a form of dissatisfaction with the initial provider. Whereas low trust in medical providers has been documented in previous research as characteristics of VH parents,8 37 38 VH parents’ consultations with multiple providers about vaccination has, to our knowledge, not extensively been studied.
Our results further imply that VH parents’ information browsing behaviours are, similarly to provider browsing, an expression of dissatisfaction and distrust. We argue that individuals who are exposed to a variety of information,39 via the internet40 41 or their social networks,16 are likely to harbour concerns or doubts about official vaccination recommendations. Our qualitative data suggest that these doubts may lead VH parents to seek information from additional sources, by consulting a different doctor or reading additional information materials. Reflecting previous findings,37 several parents described how persistent or novel doubts, uncertainty or dissatisfaction surfaced when they were exposed to new vaccination information.
Strengths and weaknesses in relation to other studies
Building on existing literature, our study provides evidence demonstrating how VH parents can be characterised by their lower levels of satisfaction and trust, and that this may be an important basis for a vicious circle of information seeking, dissatisfaction, distrust and VH, as previous studies have shown the importance of trust when it comes to addressing VH.8 42 43 Furthermore, there is a need to examine decision making on childhood vaccinations and underimmunisation among VH parents in countries where little research has been conducted.1 It is, therefore, important that research provides context-specific insights on Switzerland, due particularly to its high CAM use10 and high rates of VH.27 The focus on Switzerland, the large-scale data on the questions of VH, and the study’s mixed-methods approach speak to the novelty of this research.
That said, this is not a representative, population-based sample and it provides cross-sectional data.
Future studies could investigate how trust and satisfaction are maintained, gained, or lost over time in consultations between parents and HCPs over time.
Meaning of the study
Our results suggest potential intervention possibilities for addressing VH. Since providers remain the number one source of both VH and non-VH parents, we argue that providers can undergo vaccine consultation and communication training to engage more effectively in dialogue about vaccination with patients. Parents, especially VH parents, do not always lack facts but also may lack certainty, trust and satisfaction towards the information they obtain as well as in their medical provider. Previous literature shows that parents showing reluctancy towards childhood vaccination are not necessarily poised to reject vaccination. Such reluctancy is rather a result of uncertainty and doubt acquired through conflicting information.26 It is important that the provider does not hastily label or even exclude those patients, but rather views them as patients with doubts or concerns and with potential for productive dialogue. If hesitant parents’ questions are not adequately addressed and concerns are not met with understanding, distrust and dissatisfaction can arise. In these instances, parents may engage in provider browsing, information browsing and engage in behaviours that might increase their VH.
Unanswered questions and future research
Given the current sociocultural tension surrounding the COVID-19 pandemic, a thorough analysis of the underlying factors and potential intervention measures of widespread VH about the SARS-CoV-2 vaccine is needed. It will also be important for researchers to examine how issues of trust and satisfaction around COVID-19 vaccination services might be associated with routine childhood vaccinations and the influenza vaccination.
Supplementary Material
Acknowledgments
The authors acknowledge the effort and commitment of study participants, study nurse Andrea Kloetzer, L. Suzanne Suggs and medical students. We thank Mirjam Mäusezahl (Federal Office of Public Health) for insightful discussions.
Footnotes
SJE and MJD contributed equally.
Contributors: SJE, MD, and PET codrafted the manuscript. SJE and KJ focused on the quantitative components and MD and AB focused on the qualitative components. SM provided valuable feedback during the writing process. BMH, BW and DK gave rich insight into CAM in Switzerland. BMH and BW helped establishing the network of CAM providers and gave and insight into pediatrics in Switzerland. AB was part of the gathering of qualitative data and gave valuable feedback during the writing process. RE, JP and JH gathered data. PET was the head of the entire project. He directed and supervised all operations from start to finish. He also provided important expertise on infectious diseases and internal medicine. PET is the guarantor - he accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. All authors read and approved the final manuscript.
Funding: This work was supported by the Swiss National Science Foundation [National research programme NRP74] grant number (407440_167398) and supplementary postdoctoral fellowship funding from the Nora van Meeuwen-Haefliger-Foundation.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coidisclosure.pdf and declare: financial support from Swiss National Science Foundation (National research programme NRP74, grant 407440_167398) and supplementary postdoctoral fellowship funding from the Nora van Meeuwen-Haefliger-Foundation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as onlinew supplemental information. Raw data supporting the findings of this study are available from the corresponding author (PT) on request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
This study was conducted in compliance with the Swiss Federal Act on Research Involving Human Beings (Human Research Act) and the Declaration of Helsinki. The local ethics committee (Ethikkommission Nordwest- und Zentralschweiz, EKNZ; project ID number 2017-00725) approved the study. We obtained written informed consent from each participant after the nature and possible consequences of the study had been fully explained. Pseudonyms are used for participants throughout. Direct quotes were translated from the original language of utterance (German, French) into English.
References
- 1. Larson HJ, Jarrett C, Eckersberger E, et al. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine 2014;32:2150–9. 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- 2. MacDonald NE, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33:4161–4. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 3. Kennedy A, Lavail K, Nowak G, et al. Confidence about vaccines in the United States: understanding parents' perceptions. Health Aff 2011;30:1151–9. 10.1377/hlthaff.2011.0396 [DOI] [PubMed] [Google Scholar]
- 4. Charron J, Gautier A, Jestin C. Influence of information sources on vaccine hesitancy and practices. Med Mal Infect 2020;50:727–33. 10.1016/j.medmal.2020.01.010 [DOI] [PubMed] [Google Scholar]
- 5. Freed GL, Clark SJ, Butchart AT, et al. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics 2011;127 Suppl 1:S107–12. 10.1542/peds.2010-1722P [DOI] [PubMed] [Google Scholar]
- 6. Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother 2013;9:1763–73. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goold SD, Lipkin Jr M. The doctor–patient relationship: challenges, opportunities, and strategies. Journal of General Internal Medicine 1999;14:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117:1532–41. 10.1542/peds.2005-1728 [DOI] [PubMed] [Google Scholar]
- 9. Wolf U, Maxion-Bergemann S, Bornhöft G, et al. Use of complementary medicine in Switzerland. Forsch Komplementärmed 2006;13:4–6 10.1159/000093488 10.1159/000093488 [DOI] [PubMed] [Google Scholar]
- 10. Klein SD, Torchetti L, Frei-Erb M, et al. Usage of complementary medicine in Switzerland: results of the Swiss health survey 2012 and development since 2007. PLoS One 2015;10:e0141985. 10.1371/journal.pone.0141985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huber BM, Rodondi P-Y, Wildhaber J. [Pediatric integrative medicine is an integral part of child health care in Switzerland]. Rev Med Suisse 2020;16:2289–92. [PubMed] [Google Scholar]
- 12. Attwell K, Ward PR, Meyer SB, et al. "Do-it-yourself": Vaccine rejection and complementary and alternative medicine (CAM). Soc Sci Med 2018;196:106–14. 10.1016/j.socscimed.2017.11.022 [DOI] [PubMed] [Google Scholar]
- 13. Cassell JA, Leach M, Poltorak MS, et al. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health 2006;120:783–94. 10.1016/j.puhe.2006.03.011 [DOI] [PubMed] [Google Scholar]
- 14. Hornsey MJ, Lobera J, Díaz-Catalán C. Vaccine hesitancy is strongly associated with distrust of conventional medicine, and only weakly associated with trust in alternative medicine. Soc Sci Med 2020;255:113019. 10.1016/j.socscimed.2020.113019 [DOI] [PubMed] [Google Scholar]
- 15. Reich JA. "We are fierce, independent thinkers and intelligent": Social capital and stigma management among mothers who refuse vaccines. Soc Sci Med 2020;257:112015. 10.1016/j.socscimed.2018.10.027 [DOI] [PubMed] [Google Scholar]
- 16. Brunson EK. The impact of social networks on parents' vaccination decisions. Pediatrics 2013;131:e1397–404. 10.1542/peds.2012-2452 [DOI] [PubMed] [Google Scholar]
- 17. Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health 2020;5:e004206. 10.1136/bmjgh-2020-004206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vrdelja M, Kraigher A, Verčič D, et al. The growing vaccine hesitancy: exploring the influence of the Internet. Eur J Public Health 2018;28:934–9. 10.1093/eurpub/cky114 [DOI] [PubMed] [Google Scholar]
- 19. Johnson NF, Velásquez N, Restrepo NJ, et al. The online competition between pro- and anti-vaccination views. Nature 2020;582:230–3. 10.1038/s41586-020-2281-1 [DOI] [PubMed] [Google Scholar]
- 20. Dubé E, Gagnon D, Nickels E, et al. Mapping vaccine hesitancy--country-specific characteristics of a global phenomenon. Vaccine 2014;32:6649–54. 10.1016/j.vaccine.2014.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kata A. A postmodern Pandora's box: anti-vaccination misinformation on the Internet. Vaccine 2010;28:1709–16. 10.1016/j.vaccine.2009.12.022 [DOI] [PubMed] [Google Scholar]
- 22. Stahl J-P, Cohen R, Denis F, et al. The impact of the web and social networks on vaccination. New challenges and opportunities offered to fight against vaccine hesitancy. Med Mal Infect 2016;46:117–22. 10.1016/j.medmal.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 23. Hirschman AO. Exit, voice, and loyalty: responses to decline in firms, organizations, and states. Harvard University press, 1970. [Google Scholar]
- 24. Deml MJ, Buhl A, Huber BM, et al. Trust, affect, and choice in parents' vaccination decision-making and health-care provider selection in Switzerland. Sociol Health Illn 2022;44:41-58. 10.1111/1467-9566.13388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kasteler J, Kane RL, Olsen DM, et al. Issues underlying prevalence of "doctor-shopping" behavior. J Health Soc Behav 1976;17:328–39. 10.2307/2136711 [DOI] [PubMed] [Google Scholar]
- 26. Deml MJ, Notter J, Kliem P, et al. "We treat humans, not herds!": A qualitative study of complementary and alternative medicine (CAM) providers' individualized approaches to vaccination in Switzerland. Soc Sci Med 2019;240:112556. 10.1016/j.socscimed.2019.112556 [DOI] [PubMed] [Google Scholar]
- 27. Deml MJ, Jafflin K, Merten S, et al. Determinants of vaccine hesitancy in Switzerland: study protocol of a mixed-methods national research programme. BMJ Open 2019;9:e032218. 10.1136/bmjopen-2019-032218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks, California: SAGE Publications, Inc, 2017. [Google Scholar]
- 29. Federal Statistical Office . Main languages of the permanent resident population, 1970-2019, 2021. Available: https://www.bfs.admin.ch/bfs/en/home/statistics/population/languages-religions/languages.html [Accessed 06 Dec 2021].
- 30. Olarewaju VO, Jafflin K, Deml MJ, et al. Application of the parent attitudes about childhood vaccines (PACV) survey in three national languages in Switzerland: exploratory factor analysis and Mokken scale analysis. In: Human Vaccines & Immunotherapeutics. 17, 2021: 2652–60. https://www.tandfonline.com/doi/pdf/10.1080/21645515.2021.1894894 10.1080/21645515.2021.1894894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:1–8. 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Opel DJ, Mangione-Smith R, Taylor JA, et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin 2011;7:419–25. 10.4161/hv.7.4.14120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011;29:6598–605. 10.1016/j.vaccine.2011.06.115 [DOI] [PubMed] [Google Scholar]
- 34. Opel DJ, Taylor JA, Zhou C, et al. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr 2013;167:1065–71. 10.1001/jamapediatrics.2013.2483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Deml MJ, Buhl A, Notter J, et al. 'Problem patients and physicians' failures': what it means for doctors to counsel vaccine hesitant patients in Switzerland. Soc Sci Med 2020;255:112946. 10.1016/j.socscimed.2020.112946 [DOI] [PubMed] [Google Scholar]
- 36. Giambi C, Fabiani M, D'Ancona F, et al. Parental vaccine hesitancy in Italy - Results from a national survey. Vaccine 2018;36:779–87. 10.1016/j.vaccine.2017.12.074 [DOI] [PubMed] [Google Scholar]
- 37. Glanz JM, Wagner NM, Narwaney KJ, et al. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad Pediatr 2013;13:481–8. 10.1016/j.acap.2013.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Eller NM, Henrikson NB, Opel DJ. Vaccine information sources and parental trust in their child's health care provider. Health Educ Behav 2019;46:445–53. 10.1177/1090198118819716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang E, Baras Y, Buttenheim AM. "Everybody just wants to do what's best for their child": Understanding how pro-vaccine parents can support a culture of vaccine hesitancy. Vaccine 2015;33:6703–9. 10.1016/j.vaccine.2015.10.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sobo EJ, Huhn A, Sannwald A, et al. Information curation among vaccine cautious parents: web 2.0, Pinterest thinking, and pediatric vaccination choice. Med Anthropol 2016;35:529–46. 10.1080/01459740.2016.1145219 [DOI] [PubMed] [Google Scholar]
- 41. Betsch C, Brewer NT, Brocard P, et al. Opportunities and challenges of web 2.0 for vaccination decisions. Vaccine 2012;30:3727–33. 10.1016/j.vaccine.2012.02.025 [DOI] [PubMed] [Google Scholar]
- 42. Paterson P, Meurice F, Stanberry LR, et al. Vaccine hesitancy and healthcare providers. Vaccine 2016;34:6700–6. 10.1016/j.vaccine.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 43. Cooper S, Schmidt B-M, Sambala EZ, et al. Factors that influence parents' and informal caregivers' views and practices regarding routine childhood vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev 2021;10:CD013265. 10.1002/14651858.CD013265.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053267supp001.pdf (85.8KB, pdf)
bmjopen-2021-053267supp002.pdf (73KB, pdf)
bmjopen-2021-053267supp003.pdf (131.5KB, pdf)
bmjopen-2021-053267supp004.pdf (94.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as onlinew supplemental information. Raw data supporting the findings of this study are available from the corresponding author (PT) on request.