Abstract
Background:
In response to the opioid epidemic, addiction consultation services (ACS) increasingly provide dedicated hospital-based addiction treatment to patients with substance use disorder. We assessed hospitalist and medical staff perceptions of how the presence of 2 hospitals′ ACS impacted care for hospitalized patients with opioid use disorder (OUD). We inquired about ongoing challenges in caring for this patient population.
Methods:
We conducted a qualitative study of hospital-based providers utilizing focus groups and key informant interviews for data collection. Transcripts were analyzed using a mixed inductivedeductive approach. Emergent themes were identified through an iterative, multidisciplinary team–based process using a directed content analysis approach.
Results:
Hospitalists (n = 20), nurses (n = 13), social workers (n = 11), and pharmacists (n = 18) from a university hospital and a safety-net hospital in Colorado participated in focus groups or key informant interviews. In response to the availability of an ACS, hospitalists described increased confidence using methadone and buprenorphine to treat opioid withdrawal, which they perceived as contributing to improved patient outcomes and greater job satisfaction. Participants expressed concern about inconsistent care provided to patients with OUD that varied by the admitting team’s specialty and the physician’s background and training. Nurses and hospitalists reported frustrations with achieving adequate pain control among patients with OUD. Last, pharmacists reported practice variations when physicians dosed buprenorphine for acute pain among patients with OUD. A lack of standardized dosing led to concerns of inadequate analgesia or return to opioid use following hospital discharge.
Conclusions:
An ACS reportedly supports hospitalists and medical staff to best care for hospitalized patients with OUD. Notably, care provided to patients with OUD may not be uniform depending on various physician-level factors. Future work to address the concerns reported by study participants may include education for OUD treatment, early involvement of the ACS, and incorporation of buprenorphine prescribing algorithms to standardize care.
Keywords: Hospital medicine, addiction, addiction consult, opioid
Background
Patients with opioid use disorder (OUD) are commonly hospitalized for complications related to their substance use.1–3 Unfortunately, these hospitalizations may be complicated by patients leaving prior to treatment completion, often leading to subsequent rehospitalization due to disease progression.4,5 Highly effective medications, including buprenorphine and methadone, are available to treat OUD and are associated with a reduction in overdose-related death and all-cause mortality.6–8 It is legal to dispense methadone or buprenorphine for the prevention of opioid withdrawal during hospitalization.9,10 At hospital discharge, buprenorphine should be prescribed with linkage to ongoing OUD treatment.
Patients who prefer methadone for OUD treatment should be referred to an opioid treatment program for ongoing methadone dosing after hospital discharge. Despite the benefits of these medications, many hospitalized patients with OUD are not initiated on medications for OUD treatment during their hospitalization, even following a near-fatal opioid overdose.11–14
Various efforts to expand OUD treatment among hospitalized patients have been implemented in hospitals across the United States and Canada.15–17 Identifying and treating addiction in the hospital is associated with increased abstinence from substance use, greater engagement in addiction treatment following discharge, and decreased hospital readmissions.18–20 One effort to expand addiction treatment is to integrate addiction consultation services (ACS) in the hospital to provide dedicated addiction treatment to hospitalized patients with substance use disorder.18–21 Key aspects of care provided by an ACS include obtaining a patient history, physical exam, and laboratory testing for infectious diseases; management of substance withdrawal, when indicated; initiation of medications for substance use disorder treatment with adequate dose titration; and care linkage following hospital discharge.22 Previous work indicates that the presence of an ACS may reduce moral distress felt by providers by reframing addiction as a treatable disease, by modeling compassionate care, and by acknowledging and addressing stigma toward people with substance use disorder.23 A national survey of physicians demonstrated that hospital-based physicians (hospitalists) with access to an addiction specialist were more likely to feel supported to screen patients for concerning substance use behaviors, to be aware of local treatment resources, and to refer patients to addiction treatment.24
Integrating addiction treatment in the hospital facilitates the delivery of evidence-based care and improves provider and patient satisfaction.19,20,25,26 Due to the compelling results in other studies, we sought to explore implementation factors that may facilitate or impede efforts to utilize an ACS in 2 different hospitals. Given the team and multidisciplinary nature of use and interaction with an ACS, this paper reports results of how the presence of an ACS affected perceived care provided to hospitalized patients with OUD by different hospital-based professional groups: hospitalists, nurses, social workers, and pharmacists. We also report these groups’ perspectives on the challenges and gaps in care provided to patients with OUD and their recommendations for improvements. This work adds to the field by illuminating strategies that may be put into place to overcome challenges with implementing an ACS.
Methods
Study design
We conducted a qualitative study to facilitate a detailed understanding of participants’ perspectives on the care provided to hospitalized patients with OUD in the presence of an ACS. Qualitative research is an interpretive and naturalistic approach used to describe and understand social or human problems and the context in which the problems occur.27–29 As described by Schliep et al., “qualitative research clarifies ways to interpret and draw meaning from participants’ experiences and make sense of the context in which a phenomenon occurs,” which was the intent of the study.30 The specific design included purposeful key informant sampling and use of directed content analysis, a form of pragmatic inquiry.28,31 The Colorado Multiple Institutional Review Board (Protocol #19–0336) determined the study to be exempt from convened committee meeting review. Informed consent was obtained from all study participants.
Study setting and participants
Medical staff were eligible for participation if they worked in the hospital setting. We recruited a sample of hospitalists, nurses, social workers, and pharmacists from 2 academic hospitals, both with an ACS: a 650-bed university hospital in Aurora, Colorado, and a 525-bed safety-net hospital in Denver, Colorado. We describe study physician participants as hospitalists and other health care professionals (nurses, pharmacists, and social workers) as medical staff. The term physician, as used in the key results section, generally refers to all types of physicians and not just the hospitalists in this study. Recruitment occurred via email solicitation and placement of flyers in medical staff work areas. The sampling was purposeful in the sense that we sought to identify and include specific professional groups utilizing a key informant sampling strategy. Both hospitals implemented an ACS 2 years prior to this study. Between November 2019 and February 2020, we conducted 6 in-person focus groups with hospitalists (n = 20), social workers (n = 11), nurses (n = 5), and pharmacists (n = 18), with an average of 9 participants per group. Due to nurse scheduling, we also conducted telephone interviews with nurses at both hospitals (n = 8). Recruitment continued until all reasonable participants were included and no substantive new messages were being shared; thus, it appeared that data saturation was reached.32
Description of the ACS
The ACS at the university hospital is staffed by hospitalists trained in addiction medicine and 2 full-time addiction medicine social workers.15 The ACS at the safety-net hospital is staffed by dual-boarded internal medicine and addiction medicine physicians and includes a clinical nurse specialist. ACS physicians initiate methadone or buprenorphine for opioid withdrawal prevention and OUD treatment, they manage postoperative pain control in patients on buprenorphine or methadone, and they assist the primary team to facilitate emergency commitments for patients with life-threatening substance use.17 ACS social workers offer addiction-focused counseling in the hospital. When patients are interested, they link patients to posthospital discharge addiction treatment including outpatient counseling, intensive outpatient programs, opioid treatment programs, and outpatient-based opioid treatment programs. ACS operate during weekdays and work closely with affiliated opioid treatment programs for in-hospital methadone enrollments. Importantly, ACS team members advocate for people with substance use disorder by providing and modeling compassionate, patient-centered care.
Data collection
Two methods of data collection were utilized: focus groups and key informant interviews. We conducted focus groups to best achieve the goal of recreating the open-ended conversations and flow of ideas about patient care that occurs naturally in nursing stations, in medical staff work rooms, and in team meetings in the hospital setting. Six focus groups were segmented into 3 groups at each of the 2 hospitals: 2 groups with pharmacists, 2 groups with hospitalists, and 2 groups with nurses and social workers. We anticipated that homogenous provider groups would lead to more free-flowing conversation and would highlight differences in group perspectives.33 An experienced facilitator trained in qualitative research methods (SL) conducted the focus groups with assistance from a graduate student (KH) using an interview guide with a combination of broad, open-ended questions and follow-up prompts. Prior to each discussion, the goals of the focus group and overall study were presented to participants. Focus groups were held at the hospital over the lunch hour with lunch provided. Each focus group session was approximately 1 hour. Focus group guides were drafted on the assumption that, given the increase in opioid-related hospitalizations,34 hospitalists, nurses, pharmacists, and social workers had experience caring for patients with OUD. The guides were informed by 2 theoretical frameworks: the Knowledge, Attitudes, and Practices Framework,35 which is used to identify barriers to physician adherence to practice guidelines in relation to behavior change, and the Donabedian Framework for the Evaluation of the Quality of Care,36 which is used to identify structures, processes, and outcomes of care provided by health care organizations. Last, the interview guides were informed by a literature review exploring physician’s clinical practice when caring for patients with OUD, and their perceptions of caring for this patient population.24,25,37 The interview guides included questions to assess hospitalists’ and medical staffs’ knowledge and beliefs about patients with OUD, to understand hospital processes for treating patients with OUD, and to learn of perceived barriers and facilitators to caring for patients with OUD (Appendices A–C).
We experienced difficulty recruiting nurses to participate in focus groups due to work-schedule conflicts. To increase nurse participation, we conducted key informant interviews with nurses over the telephone at a convenient time to reach data saturation. The facilitator (SL) and principal investigator (SLC) conducted all interviews. Neither interviewer had previous relationships with key informant interviewees. Prior to each interview, the goals of the conversation and overall study were presented to key informant interviewees. Each nurse was provided with a modest monetary incentive for participation. Key informant interviews were approximately 45 minutes. Summary and reflective notes were completed after each focus group and key informant interview using a semi-structured template.38 All sessions were digitally recorded, transcribed verbatim, cleaned, organized by file naming, and entered into ATLAS.ti, version 8 for data organization and management (ATLAS.ti GmbH).39
Data analysis
An iterative and team-based process using a constant comparative method and reflexive team analysis guided by a directed content analysis was conducted.40 The qualitative analysis team included the following team members: principal investigator (SLC), a hospitalist (CC), a trained qualitative analyst (SL), and a graduate student (KH). The study team was mentored by a senior scientist with expertise in qualitative and mixed methods research methodology (JH). The study team both inductively and deductively developed a codebook. Initial domains for codes were informed by our interview guide and included the following categories: knowledge/training; attitudes; barriers; facilitators; processes/structures of care; and outcomes of care.35,41 The codebook was expanded based on codes that emerged from the data and iterative discussion while reviewing the data individually and in group review sessions.42 The study team reviewed and consolidated their emergent codes until no new codes were identified and there was strong code assignment agreement. All transcripts were independently read, double-coded, and merged prior to analysis. Any discrepancies in coding were addressed through discussion and consensus among the coders.40 Throughout the analytic process, the study team met regularly to discuss new findings and emergent new codes and themes and to assess the preliminary and final results.40 In this manuscript, we present emergent themes related to changes in care provision to hospitalized adults with OUD in the setting of an ACS and ongoing areas needing improvement.
Key results
We conducted 6 focus groups with approximately 9 participants per group and 8 key informant interviews with nurses (n = 62) (Table 1). From our focus groups and key informant interviews, we identified emergent themes in 3 domains: (1) perceived benefits of buprenorphine and methadone on patient outcomes and provider satisfaction; (2) perceived concern for ongoing, inconsistent care provided to patients with OUD; and (3) perceived challenges with pain management in patients with OUD (Figure 1).
Table 1.
Demographic data of participants (N = 62).*
| Variables | N (%) | Interview type |
|---|---|---|
| Female | 46 (75) | |
| Male | 16 (25) | |
| Job type | FG and II (n) | |
| Physician | 19 (31) | FG (2) |
| Pharmacist | 18 (30) | FG (2) |
| Nurse | 13 (21) | FG (2) & II (8) |
| Social worker | 11 (18) | FG (2) |
| Years working in job type | ||
| ≤5 | 20 (33) | |
| 6–10 | 17 (28) | |
| 11–15 | 16 (26) | |
| ≥15 | 8 (13) |
Note.
N = 62 participants; 1 participant did not complete a survey. FG = focus groups; II = individual interviews.
Figure 1.
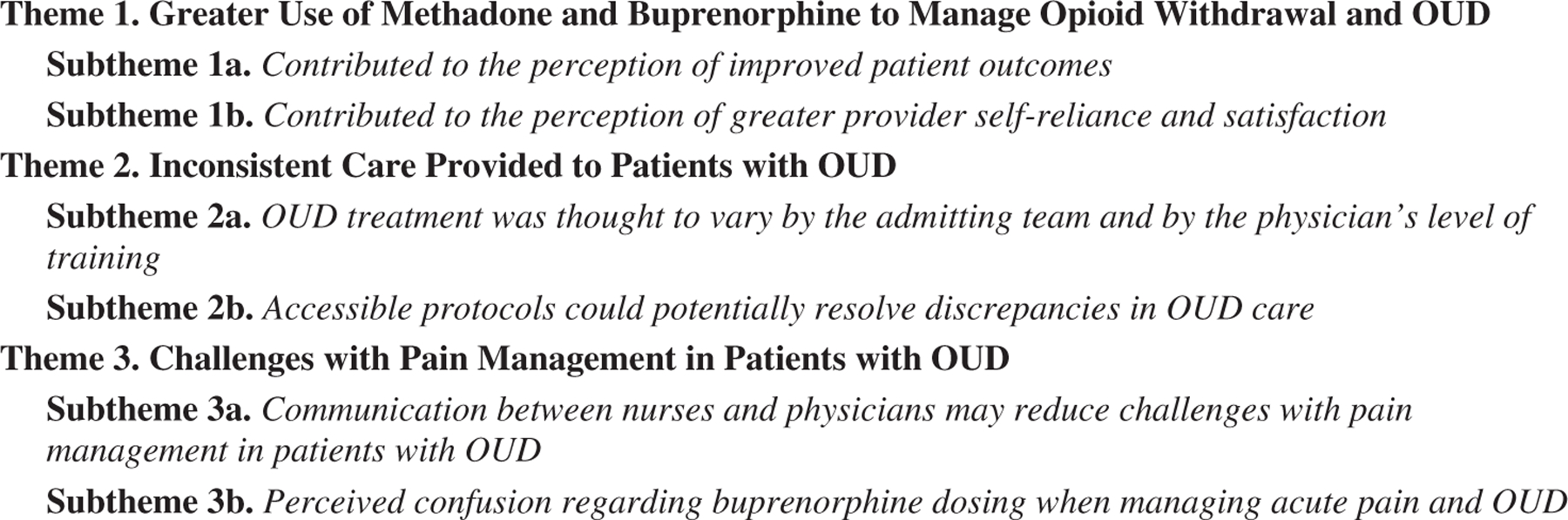
Emergent themes (in text).
Key themes
Theme 1: With the ACS, hospitalists and other health care professionals perceived greater use of methadone and buprenorphine to manage opioid withdrawal and OUD
Subtheme 1a: Greater use of methadone and buprenorphine contributed to the perception of improved patient outcomes.
Hospitalists, nurses, and social workers reported that, with the presence of the ACS, they believed there was increased use of buprenorphine and methadone for management of opioid withdrawal. This practice change was thought to have contributed to improved patient outcomes including fewer patient-directed discharges, increased patient comfort, and a perception that patients were being linked to definitive OUD treatment following discharge. These perceptions were reported across all professional groups.
I just had a patient a week ago that needed oxygen and had pneumonia. He was about to leave AMA … just treating the withdrawal with buprenorphine and getting him plugged in … he stayed a couple of days and was incredibly grateful. It was [a] night-and-day difference from how things were in the past. … I appreciate how much their behavior is correlated with poorly treated withdrawal. (Hospitalist)
Subtheme 1b: Greater use of methadone and buprenorphine contributed to the perception of greater provider self-reliance and satisfaction.
Hospitalists noted that with increased use of buprenorphine and methadone, they became more confident when treating patients with OUD, which led to a reported increased satisfaction when caring for these patients.
When I have a path by which I could see how a patient’s gonna be cared for during hospitalization, it gives you a great deal of courage and confidence. And you can walk into that room and know you’re in charge of all the aspects of their care. (Hospitalist)
Nurses and pharmacists also recognized greater confidence in hospitalists’ management of opioid withdrawal, shifting from “as-needed” medications for symptomatic relief to initiating methadone or buprenorphine for definitive OUD treatment.
I think providers are less intimidated by using buprenorphine. And so, we’re able to effectively treat these patients, and that’s really helped. We’re not undertreating them, but we’re also not dumping them with tons of opioids. Using these adjunct drugs to help them withdraw safely in a safe environment is much more humane. (Nurse)
Theme 2. Even with an ACS, hospitalized patients with OUD may receive inconsistent care
Subtheme 2a. OUD treatment was thought to vary by the admitting team and physician training.
Nurses reported that the use of methadone and buprenorphine seemed variable among their patients. This was concerning because standardized care was not being provided to their patients.
You know, patient A’s getting these medications, and patient B isn’t. Why isn’t patient B? Is it because of a clinical indication, or is it because the physician’s uncomfortable with prescribing these medications? (Nurse)
Nurses observed that OUD treatment practices seemed to depend upon the admitting team and the physician’s experience or training in OUD.
My perception is that the surgical services don’t have a good handle on any of it [OUD management]. I don’t know what any curriculum looks like in medical school or in residency, and I feel like more robust training would be infinitely helpful for everybody because this permeates everywhere. (Nurse)
Subtheme 2 b. Accessible protocols could potentially resolve discrepancies in OUD care.
Pharmacists attributed discordant OUD management to a lack of easily accessible protocols with best practice recommendations for buprenorphine dosing.
Treating acute pain syndromes with these patients on long-term maintenance therapies, we don’t have a protocol within our institution. That could be a good thing. Creating policies, protocols, or guidelines helps. (Pharmacist)
Theme 3. Challenges with pain management in patients with OUD persist
Subtheme 3a. Increased communication between nurses and physicians may reduce challenges with pain management in patients with OUD.
Nurses described challenges with pain control in patients with OUD due to difficult patient behaviors. Nurses appreciated it when physicians involved them in the pain management plan.
It depends on the primary team, how they’ll write the orders based on those patients’ needs. … If the pain medications ordered are not adequate for managing the patient’s pain, and they’re not narcotized in any way, and the doctors won’t give them any more pain meds, then it’s challenging. Some doctors are more open to hear what you’re saying. (Nurse)
In contrast, hospitalists expressed concern with underutilization of “as-needed” opioids prescribed for patients with OUD. This reluctance to administer opioids for pain control was attributed to mixed messaging associated with the use of opioids in the time of an opioid epidemic.
Every time I’ve encountered that [reluctance to administer “as-needed” opioids] I’ve done the education myself with nursing. It’s a lot because it’s not just like, “These are the medications, and these are how they work,” but “This is how we talk about people with OUD. This is what it means to have pain when you have OUD and why you need a PCA [patient-controlled analgesia]. (Hospitalist)
Subtheme 3b. Perceived confusion regarding buprenorphine dosing in setting of acute pain and OUD.
Pharmacists described various practices by physicians with buprenorphine continuation or cessation in the setting of acute pain. There was a concern that in either scenario, the patient may have uncontrolled pain or their OUD recovery may be destabilized.
Scenario 1: “The pain team felt that buprenorphine should be held because we were trying to treat this guy’s actual pain, but the primary service didn’t feel comfortable holding it. Those kinds of conflicts come up in those situations. The attending I was with that week felt pretty strongly, and I tend to agree, that if we’re trying to treat their pain, then why give a partial agonist that’s just gonna tie up receptors?” (Pharmacist)
Scenario 2: “It is extremely difficult, if you stop buprenorphine, to restart it. It’s a partial agonist, but it still provides great analgesia. I think things are going back the other way, that you use multimodal pain management and higher doses of opioids than you would without buprenorphine. [Addiction physician] can tell you disastrous cases where buprenorphine was stopped for acute pain or a procedure, and they couldn’t get the person back on it.” (Pharmacist)
Discussion
In this qualitative study of hospitalists, nurses, social workers, and pharmacists working in hospitals with an ACS, we identified important themes around beneficial changes and ongoing challenges in care provided to hospitalized adults with OUD. This study affirmed previously reported findings that physicians express greater job satisfaction and confidence when they believe they are treating patients with substance use disorder humanely, by prescribing medications to manage their substance use and withdrawal symptoms.23,25 Important challenges remain in the care of people with OUD, even with readily available access to addiction experts through an ACS. Nurses perceived inconsistent use of methadone and buprenorphine for opioid withdrawal management. Hospitalists, nurses, and pharmacists perceived difficulty with pain management in patients with OUD due to poor communication and underutilization of opioids for acute pain management. Finally, pharmacists reported confusion over conflicting physician practices when dosing buprenorphine for acute pain and OUD.
Hospitalists and medical staff identified that with the ACS there was greater use of methadone and buprenorphine to manage opioid withdrawal and OUD. However, medical staff also perceived variable use of these medications across physician type and level of training. Overcoming these variations in practice is important because multiple guidelines recommend the use of these medications to manage opioid withdrawal with continuation for treatment of OUD.43–47 Furthermore, high-quality evidence demonstrates a mortality benefit with OUD treatment continuation with opioid agonist therapy vs opioid withdrawal management alone.48–50 Both buprenorphine and methadone can be legally prescribed by any physician to hospitalized patients experiencing opioid withdrawal who were hospitalized for medical reasons beyond OUD, for example, endocarditis or infection.10 Multiple online resources provide step-by-step buprenorphine initiation protocols for reference.51,52 While an X waiver is required to prescribe buprenorphine at hospital discharge, prescribers are no longer required to complete buprenorphine waiver training and can apply for a Notification of Intent to prescribe buprenorphine.53 Finally, patients who prefer methadone for OUD treatment following hospital discharge require enrollment to an opioid treatment program, and this care linkage can be facilitated by the ACS.54 Education regarding best practice for opioid withdrawal management and OUD treatment targeted to medical students, medical residents, and established physicians could reduce the treatment variability reported in this study.
Despite the presence of an ACS, hospitalists and medical staff reported challenges with pain management among patients with OUD. Pharmacists described variable buprenorphine prescribing practices by physicians for patients with OUD and acute pain. Expert consensus and recommendations incorporate the use of multimodal pain control methods, including the use of short-acting opioid agonists, for example, oxycodone or hydromorphone, to manage acute pain in patients with OUD.55,56 Increasingly, experts recommend continuing buprenorphine in the perioperative period to avoid the risk of relapse to illicit opioid use.57–62 Integrating evidenced-based recommendations for pain management among people with OUD in the form of easily accessible electronic protocols, as suggested by the pharmacists included in our study, could reduce difficulties related to pain management in patients with OUD. Nurses and hospitalists described challenges in communication as a factor contributing to difficult pain management in patients with OUD. Previous studies demonstrate that much of pain management depends on how patients, physicians, and medical staff interact with one another when discussing expectations and strategies for pain control.63–65 Identifying approaches to address and resolve communication challenges among physicians, medical staff, and patients may mitigate the concerns described by our study participants. For example, “giving permission” to physicians and medical staff to prescribe and dispense opioid pain medications to people with acute pain and OUD at higher doses and shorter intervals may reduce some of the concerns expressed by hospitalists and medical staff.56
Limitations
The study findings should be interpreted in the context of the potential limitations of our study. Our study participants worked in one of two academic hospitals in a large metropolitan area. Both hospitals have a weekday ACS available to consult on patients with substance use disorder. Thus, the experiences described by our study participants may not reflect experiences of hospitalists or medical staff working in hospitals without access to an ACS or dedicated addiction experts. We included hospitalists, social workers, pharmacists, and nurses working in 2 hospitals to obtain multiple professional perspectives of people who interact with the patient population of interest. Although qualitative research is not intended to be representative, our purposeful selection may have resulted in recruiting study participants who were more interested or engaged with this topic and may have strong opinions about treating patients with OUD. In all qualitative studies, findings may be influenced by the perspectives of investigators during the collection and analysis of the data. We assembled a multidisciplinary team and used a team-based, iterative process with triangulation to employ a rigorous approach to our study questions. Lastly, although there is a temptation to sort the data by provider type, our results indicated common themes that crossed professions and were uniformly present.66
Conclusions
This study illustrates key aspects of OUD care provision that were perceived as beneficial for patients and for hospitalists and medical staff while also identifying areas that need ongoing improvement. An ACS may offer positive benefits to patients with OUD, but these benefits may be limited to patients cared for by selected physicians who consult the ACS for assistance with OUD management. This leads to unequal care provided to hospitalized patients with OUD within the same institution. Given the various challenges reported by hospitalists and medical staff, targeted strategies may be considered to address individual areas needing improvement. For example, some medical staff participants noted that education and training on OUD treatment should be offered in medical school, that prescribing of medications for OUD treatment should be standardized and informed by existing protocols, and that greater efforts to improve upon physician–medical staff–patient communication may reduce challenges with pain management. Future work could include the design, implemention, and evaluation of these strategies for future improvement of care provided to hospitalized patients with OUD.
Supplementary Material
Table 2.
Qualitative theme with additional health care perspectives and representative quotes.
| Theme and subtheme | Respondent | Representative quote |
|---|---|---|
| Greater use of methadone and buprenorphine to manage opioid withdrawal and OUD | ||
| • Increased use of methadone and buprenorphine was perceived to have contributed to improved patient outcomes | Pharmacist | I think more people are being treated, fewer people are falling through the cracks with transitions in care, especially with things being initiated inpatient and the communication to the outpatient clinic world. |
| • Increased use of methadone and buprenorphine contributed to the perception of greater provider self-reliance and satisfaction | Pharmacist | I think a shift from considering as-needed medications for controlling withdrawal vs prescribing methadone or buprenorphine, that’s where there has been a decent switch with the new protocols and the expansion of addiction medicine. |
| Social worker | It’s pretty significant for me from a social work standpoint. It has significantly reduced the amount of planning and coordination that I have to do because we have people who are experts in doing that and coordinating methadone and Suboxone starts. We really have an exceptional team too that goes above and beyond. They really know the system. | |
| Inconsistent care provided to patients with OUD | ||
| • OUD treatment was thought to be varied by the admitting team and physician’s level of training | Social worker | Our doctors are not coming at situations motivationally interviewed or trauma-informed when they’re having these conversations. I do not know that everybody’s skill set includes that or has given them the opportunity to really practice and home in on it. … Creating a safe space to be able to tell your provider what you’re really going through without worrying about the consequences. I think that’s a huge barrier. |
| •Accessible protocols could potentially resolve discrepancies in OUD care | Pharmacist | I know sometimes somebody’s admitted overnight. We have limited knowledge of what they have been using. The overnight resident isn’t familiar with our protocols so they’re deferring to the day team. I’ve seen several patients we could have intervened on earlier. They start to have withdrawal symptoms. Then it’s not until the next morning after the physician has seen them that we get them squared away with more robust treatment |
| Challenges with pain management in patients with OUD persist | ||
| • Increased communication between nurses and physician may reduce challenges with pain management in patients with OUD | Nurse | A times, patients will say, “I’m in pain,” and your observation is they look completely comfortable, and they’re on their phone. It’s usually oxycodone that I’m administering or hydromorphone. I thought in the past, “Well, I’m not a provider. I don’t prescribe,” but with the fact that state is looking at nursing and our nursing assessments regarding pain, that’s—that’s frustrating to me that I’m not the one who prescribes these, I’m not the one who makes those decisions. |
| • Perceived confusion regarding buprenorphine dosing in setting of acute pain and OUD | Pharmacist | Buprenorphine tends to be the trickier one because there are different preferences for whether a patient stops, but again, mine is usually for pain, so it’s not really for opioid use disorder. That’s tricky. For pain, it’s different, whether they stop or start it. |
Note. OUD = opioid use disorder.
Funding
Dr Calcaterra is supported by the National Institute on Drug Abuse, National Institutions of Health, grant award number K08DA049905. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health.
Footnotes
Supplemental data for this article is available online at publisher’s website.
Disclosure statement
The authors declare that they do not have any conflicts of interest.
References
- [1].Rudasill SE, Sanaiha Y, Mardock AL, et al. Clinical outcomes of infective endocarditis in injection drug users. J Am Coll Cardiol 2019;73(5):559–570. [DOI] [PubMed] [Google Scholar]
- [2].Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009–2014: statistical brief #219. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. [Google Scholar]
- [3].Singh JA, Cleveland JD. National U.S. time-trends in opioid use disorder hospitalizations and associated healthcare utilization and mortality. PLoS One 2020;15(2):e0229174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Choi M, Kim H, Qian H, Palepu A. Readmission rates of patients discharged against medical advice: a matched cohort study. PLoS One 2011;6(9):e24459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mejia de Grubb MC, Salemi JL, Gonzalez SJ, Chima CC, Kowalchuk AA, Zoorob RJ. Opioid, cocaine, and amphetamine use disorders are associated with higher30-day inpatient readmission rates in the United States. Subst Abus 2020;41(3): 310–365. [DOI] [PubMed] [Google Scholar]
- [6].Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and metaanalysis of cohort studies. BMJ 2017;357:j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hickman M, Steer C, Tilling K, et al. The impact of buprenorphine and methadone on mortality: a primary care cohort study in the United Kingdom. Addiction 2018;113(8):1461–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2003;(2):CD002209. [DOI] [PubMed] [Google Scholar]
- [9].Noska A, Mohan A, Wakeman S, Rich J, Boutwell A. Managing opioid use disorder during and after acute hospitalization: a case-based review clarifying methadone regulation for acute care settings. J Addict Behav Ther Rehabil 2015;4(2):1000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].US Department of Justice DEA, Diversion Control Divsion. Title 21 Code of Federal Regulations: PART 1306 — PRESCRIPTIONS: §1306.07 Administering or dispensing of narcotic drugs. DRUG ENFORCEMENT ADMINISTRATION https://www.deadiversion.usdoj.gov/21cfr/cfr/1306/1306_07.htm. Published 2020. Accessed May 19, 2021.
- [11].Rosenthal ES, Karchmer AW, Theisen-Toupal J, Castillo RA, Rowley CF. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med 2016;129(5):481–485. [DOI] [PubMed] [Google Scholar]
- [12].Peterson C, Xu L, Mikosz CA, Florence C, Mack KA. US hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011–2015. J Subst Abuse Treat 2018;92:35–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kilaru AS, Xiong A, Lowenstein M, et al. Incidence of treatment for opioid use disorder following nonfatal overdose in commercially insured patients. JAMA Netw Open 2020;3(5): e205852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med 2018;169(3): 137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Calcaterra SL, McBeth L, Keniston AM, Burden M. The development and implementation of a hospitalist-directed addiction medicine consultation service to address a treatment gap. J Gen Intern Med 2021. doi: 10.1007/s11606-021-06849-8 [DOI] [PMC free article] [PubMed]
- [16].Braithwaite V, Ti L, Fairbairn N, et al. Building a hospital-based addiction medicine consultation service in Vancouver, Canada: the path taken and lessons learned. Addiction 2021;116(7): 1892–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am 2018;102(4):587–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Englander H, Dobbertin K, Lind BK, et al. Inpatient addiction medicine consultation and post-hospital substance use disorder treatment engagement: a propensity-matched analysis. J Gen Intern Med 2019;34(12):2796–2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wakeman SE, Kane M, Powell E, Howard S, Shaw C, Regan S. Impact of inpatient addiction consultation on hospital readmission. J Gen Intern Med 2021;36(7):2161–2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Intern Med 2017;32(8):909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Association AH. Addressing the opioid epidemic-resources https://www.aha.org/advocacy/access-and-health-coverage/access-behavioral-health/opioids. Published 2018. Accessed September 26, 2020.
- [22].Priest KC, McCarty D. The role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med 2019;13(2):104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’attitudes and experiences. J Hosp Med 2018;13(11):752–758. [DOI] [PubMed] [Google Scholar]
- [24].Calcaterra SL, Binswanger IA, Edelman EJ, McNair BK, Wakeman SE, O’Connor PG. The impact of access to addiction specialist on attitudes, beliefs and hospital-based opioid use disorder related care: A survey of hospitalist physicians. Subst Abus 2020:1–9. doi: 10.1080/08897077.2020.1748169 [DOI] [PMC free article] [PubMed]
- [25].Wakeman SE, Kanter GP, Donelan K. Institutional substance use disorder intervention improves general internist preparedness, attitudes, and clinical practice. J Addict Med 2017;11(4): 308–314. [DOI] [PubMed] [Google Scholar]
- [26].Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med 2019. doi: 10.1007/s11606-019-05311-0 [DOI] [PubMed]
- [27].Denzin NK, Lincoln YS. Introduction: The discipline and practice of qualitative research. In: Denzin NK, Lincoln YS, eds. The Sage Handbook of Qualitative Research Thousand Oaks, CA: Sage Publications Ltd.; 2005:1–32. [Google Scholar]
- [28].Creswell JW, Poth CN. Qualitative Inquiry and Research Design: Choosing among Five Approaches Thousand Oaks, CA: Sage publications; 2016. [Google Scholar]
- [29].Starks H, Brown Trinidad S. Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res 2007;17(10):1372–1380. [DOI] [PubMed] [Google Scholar]
- [30].Schliep ME, Alonzo CN, Morris MA. Beyond RCTs: innovations in research design and methods to advance implementation science. Evid-Based Commun Assess Intervent 2017; 11(3–4):82–98. [Google Scholar]
- [31].Fetters MD. The Mixed Methods Research Workbook: Activities for Designing, Implementing, and Publishing Projects Thousand Oaks, CA: SAGE Publications; 2019. [Google Scholar]
- [32].Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods 2006;18(1):59–82. [Google Scholar]
- [33].Morgan DL. Focus Groups as Qualitative Research Vol 16. Thousand Oaks, CA: Sage publications; 1996. [Google Scholar]
- [34].Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/ dependence and associated serious infections increased sharply, 2002–12. Health Aff (Millwood)) 2016;35(5):832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Cabana MD, Rand CS, Powe NR, et al. “Why don’t physician follow clinical practice guidelines?” A framework for improvement.. JAMA 1999;282(15):1458–1465. [DOI] [PubMed] [Google Scholar]
- [36].Donabedian A Evaluating the quality of medical care. Milbank Q 2005;83(4):691–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus 2016;37(4):635–641. [DOI] [PubMed] [Google Scholar]
- [38].Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6): 349–357. [DOI] [PubMed] [Google Scholar]
- [39].Analysis AtQD. Qualitative Data Analysis Software http://atlasti.com/. Published 2020. Accessed February 13, 2021.
- [40].Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- [41].Donabedian A Evaluating the quality of medical care. Milbank Mem Fund Q 1966;44(3): 166–206. [PubMed] [Google Scholar]
- [42].Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5(1): 80–92. [Google Scholar]
- [43].Department of Veterans Affairs. VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders Washington, DC: Department of Veterans Affair–Department of Defense United States of America; 2015. [Google Scholar]
- [44].Gowing L, Ali R, Dunlop A, Farrell M, Lintzeris N. National guidelines for medication-assisted treatment of opioid dependence Canberra: Commonwealth of Australia; 2014:77–162. [Google Scholar]
- [45].Bruneau J, Ahamad K, Goyer ME, et al. Management of opioid use disorders: a national clinical practice guideline. CMAJ 2018;190(9):E247–E257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Cunningham CE, Fishman M, Gordon AJ, et al. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med 2020;14(2S Suppl 1): 1–91. [DOI] [PubMed] [Google Scholar]
- [47].Comer S, Cunningham C, Fishman MJ, et al. National practice guideline for the use of medications in the treatment of addiction involving opioid use. Am Soc Addicit Med 2015:1–66. https://newmexico.networkofcare.org/content/client/1446/2.6_17_AsamNationalPracticeGuidelines.pdf
- [48].Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Syst Rev 2009;(3): CD002209. doi: 10.1002/14651858.CD002209.pub2 [DOI] [PMC free article] [PubMed]
- [49].Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014;(2). doi: 10.1002/14651858.CD002207.pub2 [DOI] [PMC free article] [PubMed]
- [50].Gowing L, Ali R, White JM. Buprenorphine for the management of opioid withdrawal. Cochrane Database Syst Rev 2009; (3):CD002025. doi: 10.1002/14651858.CD002025.pub5 [DOI] [PubMed] [Google Scholar]
- [51].Medicine YDoE. ED-Initiated Buprenorphine https://medicine.yale.edu/edbup/Algorithm_338052_5_v2.pdf. Published 2020. Updated 09/24/2019. Accessed February 12, 2021.
- [52].Project CB. Buprenorphine hospital quick start CA Bridge. https://cabridge.org/resource/buprenorphine-bup-hospital-quick-start/. Published 2021. Accessed February 12, 2021. [Google Scholar]
- [53].Substance Abuse and Mental Health Services Administration. Buprenorphine https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenor-phine. Published 2021. Accessed 2021, May 20.
- [54].Substance Abuse and Mental Health Services Administration. Federal Guidelines for Opioid Treatment Programs HHS Publication No. (SMA) XX-XXXX. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- [55].Ti L, Voon P, Dobrer S, Montaner J, Wood E, Kerr T. Denial of pain medication by health care providers predicts in-hospital illicit drug use among individuals who use illicit drugs. Pain Res Manag 2015;20(2):84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med 2006;144(2):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Goel A, Azargive S, Weissman JS, et al. Perioperative Pain and Addiction Interdisciplinary Network (PAIN) clinical practice advisory for perioperative management of buprenorphine: results of a modified Delphi process. Br J Anaesth 2019;123(2): e333–e342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Haber LA, DeFries T, Martin M. Things we do for no reason™: Discontinuing buprenorphine when treating acute pain. J Hosp Med 2019;14(10):633–635. [DOI] [PubMed] [Google Scholar]
- [59].Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period Oxford University Press; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Quaye AN-A, Zhang Y. Perioperative management of buprenorphine: solving the conundrum. Pain Med 2019;20(7): 1395–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Quaye A, Potter K, Roth S, Acampora G, Mao J, Zhang Y. Perioperative continuation of buprenorphine at low-moderate doses was associated with lower postoperative pain scores and decreased outpatient opioid dispensing compared with buprenorphine discontinuation. Pain Med 2020;21(9):1955–1960. [DOI] [PubMed] [Google Scholar]
- [62].Goel A, Azargive S, Lamba W, et al. The perioperative patient on buprenorphine: a systematic review of perioperative management strategies and patient outcomes. Can J Anesth/J Can Anesth 2019;66(2):201–217. [DOI] [PubMed] [Google Scholar]
- [63].Butow P, Sharpe L. The impact of communication on adherence in pain management. PAIN® 2013;154 Suppl 1:S101–S107. [DOI] [PubMed] [Google Scholar]
- [64].Millard L, Hallett C, Luker K. Nurse-patient interaction and decision-making in care: patient involvement in community nursing. J Adv Nurs 2006;55(2):142–150. [DOI] [PubMed] [Google Scholar]
- [65].Cormie P, Nairn M, Welsh J. Control of pain in adults with cancer: summary of SIGN guidelines. BMJ 2008;337:a2154. [DOI] [PubMed] [Google Scholar]
- [66].Holtrop JS, Fisher M, Martinez DE, et al. What works for managing chronic pain: an appreciative inquiry qualitative analysis. J Prim Care Community Health 2019;10:2150132719885286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


