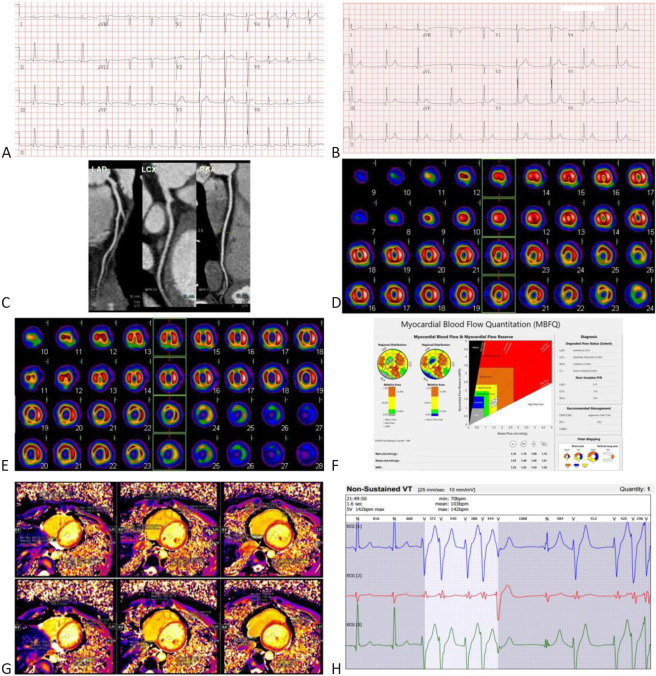
Figure 1.
(A) At 15 years old, 12-lead electrocardiogram (ECG) showed elevations of ST-segments in V1-V4 at the onset of angina pectoris and ischemia and no obstructive coronary artery disease (INOCA). (B) After recovery from angina pectoris and INOCA, a follow-up 12-lead ECG showed regression of elevation of ST-segment in V1-V4. (C) At 19 years old, computerized tomography angiography of coronary artery showed non-obstructive coronary artery disease and no myocardial bridging coronary artery of the left anterior descending coronary artery (LAD), left circumflex coronary artery (LCX), and right coronary artery (RCA). (D) At 20 years old, thallium-201 single photon emission computed tomography-myocardial perfusion image (SPECT-MPI) showed fixed and some reversible perfusion defects, involving the apex, apical-mid-basal anterior, basal anteroseptal, apical-mid-inferior, and basal inferoseptal segments of the left ventricle (LV). (E) At 24.5 years old, technetium-99m sestamibi dynamic SPECT-MPI showed fixed perfusion defects involving the same territories of the LV. (F) Simultaneously, dipyridamole-stress technetium-99m sestamibi dynamic SPECT was performed to study the myocardial blood flow quantitation (MBFQ). Interestingly, myocardial flow reserve (MFR) of the LV, left anterior descending coronary artery (LAD), left circumflex coronary artery (LCX), and right coronary artery (RCA) were 1.35, 1.23, 1.53, and 1.35, respectively. Stress flow (SF) of the LV, LAD, LCX, and RCA were 1.53 mL/min/gm, 1.46 mL/min/gm, 1.65 mL/min/gm, and 1.51 mL/min/gm, respectively. Using thresholds of MFR ≤ 1.74 and/or SF ≤ 1.54 mL/min/gm, the polar map and Gould’s plot showed an 8.29% ischemia in our patient. (G) At the same time, adenosine-stress cardiac magnetic resonance images (MRI) showed a blunted T1 reactivity (ΔT1 = (stress T1 – rest T1)/rest T1 = 0.3%-3.8%). A decrease of MFR and SF (repercussion of coronary flow reserve) by dipyridamole-stress dynamic SPECT MBFQ, and a blunted T1 reactivity by adenosine-stress cardiac MRI substantiate presence of coronary microvascular dysfunction (CMVD) and meet the diagnostic criteria of microvascular angina (MVA). (H) Holter ECG showed non-sustained ventricular tachycardia.