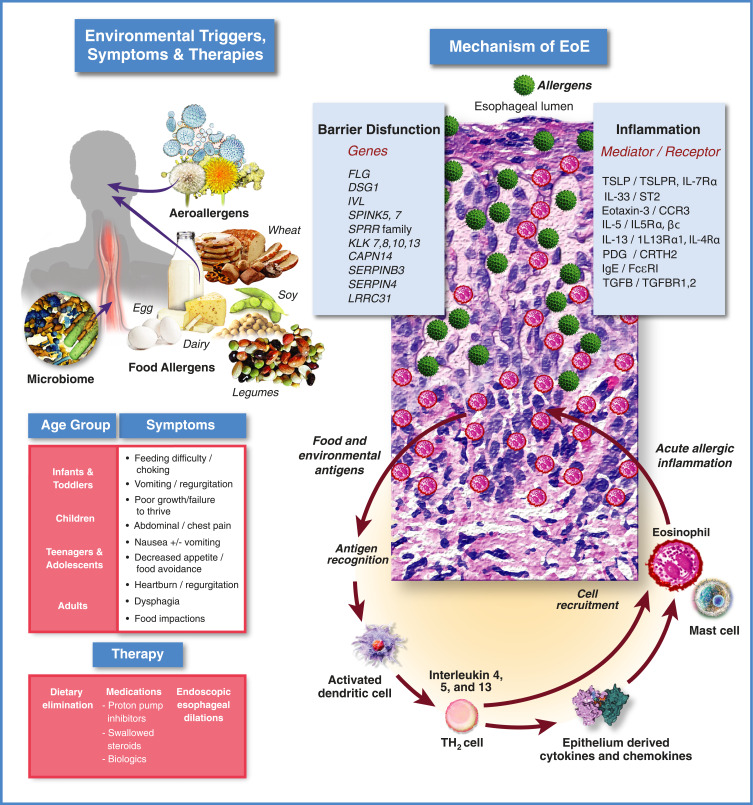
Figure 1.
Eosinophilic esophagitis: clinical & pathophysiologic overview.
Notes: Top Left: Major known environmental triggers of EoE include most commonly food allergens (ie, dairy, wheat, egg, soy and legumes) and to a lesser extent, aeroallergens (eg, pollen). Recently, a role for the gut microbiome in inception and/or severity of EoE has been proposed.209 Middle Left: EoE symptoms by age group. Bottom left: The three main classes of EoE therapies: 1.) diet modification, ie, elimination diets; 2.) medications including proton pump inhibitors, topical swallowed corticosteroids, and biologics; 3.) endoscopic dilation. Upper right: EoE pathophysiology current understanding. A breach in the integrity of the esophageal epithelium, potentially facilitated by gastric acid exposure and/or carriage of genetic variants that compromise epithelial barrier function, allows ingress of food or aeroallergens (green spheres) leading to initiation of an immune response. Dilated intercellular spaces seen in biopsies of esophageal epithelium are a hallmark of EoE and tend to reflect disease severity. Interleukins produced by activated Th2 cells can act directly to recruit eosinophils to the esophagus (IL-5, red/pink cells), or can stimulate the epithelium to express inflammatory genes (IL-4/IL-13), including eotaxin-3, by activation of cell surface receptors that signal through a pathway involving JAKs and STAT6. Eotaxin-3 produced by the epithelium is a powerful chemotactic factor for eosinophils which are then recruited to the esophageal epithelium to propagate the inflammatory response. Mast cells also play a role in the inflammatory response that continues to be an active area of research investigation.