Abstract
Objective:
Access to firearms is an independent risk factor for completed suicide and homicide, and the American Academy of Pediatrics recommends that pediatricians screen and counsel about firearm access and safe storage. This study investigates how often pediatric residents screen for access to firearms or counsel about risk-reduction in patients with suicidal or homicidal ideation.
Methods:
Retrospective chart review of visits by patients younger than the age of 19 years presenting to the pediatric emergency department (ED) of a tertiary academic medical center from January to December 2016. Visits were eligible if there was an ultimate ED discharge diagnosis of “suicidal ideation,” “suicide attempt,” or “homicidal ideation” as identified by International Statistical Classification of Diseases and Related Health Problems, 10th revision codes and the patient was seen by a pediatric resident before evaluation by psychiatry. Descriptive statistics were used to analyze results.
Results:
Ninety-eight patients were evaluated by a pediatric resident for medical assessment before evaluation by a psychiatry team during the study period and were therefore eligible for inclusion. Screening for firearm access was documented by a pediatric resident in 5 of 98 (5.1%) patient encounters. Twenty-five patients (25.5%) had no documented screening for firearm access by any provider during the ED visit, including in 5 cases when patients were discharged home.
Conclusions:
Pediatric residents rarely document screening for firearm access in patients with known suicidal or homicidal ideation who present to the ED. Additional understanding of the barriers to screening and potential strategies for improving screening and counseling are critical to providing appropriate care for high-risk pediatric patients.
Keywords: guns, injury prevention, trauma
Firearm-related injury among children and adolescents is a persistent public health problem in the United States. In particular, children at risk for self-harm or harm to others represent a population for whom understanding access to firearms is particularly important. Firearms represent one of the most lethal methods of suicide attempt, with completion in up to 90% of attempts.1,2 Of all homicides in adolescents between 15 and 19 years of age, approximately 90% are firearm-related.3 Adolescents are particularly vulnerable to firearm-related injuries, as they are more likely to exhibit impulsivity, and the presence of a firearm in the home repeatedly has been shown to increase their overall risk of death.4–8 Given these risks, the American Academy of Pediatrics has issued guidelines recommending that pediatricians routinely screen for access to firearms and counsel about risk reduction, including safe storage practices, as well as counseling families to remove firearms from the home of any adolescent.4,9,10
Although all pediatricians share the responsibility for this counseling, emergency department (ED) clinicians are often the first-line physicians to care for a child after disclosure of homicidal ideation, suicidal ideation, or a suicide attempt. Visits to pediatric EDs for psychiatric conditions continue to increase.11 Therefore, physicians in the ED should be equipped to effectively screen for access to lethal means, including firearms, and counsel about risk reduction during these visits. Previous studies have shown that ED clinicians often do not screen for access to firearms, even in high-risk patients.12–15 Limited previous data show that trainees also appear to have low rates of screening, with one study of psychiatry residents showing that firearms access screening was documented in only 3% of patient encounters.16 The rate of screening for access to firearms by pediatric trainees in high-risk patients presenting to the ED is unknown.
In our hospital, all patients 19 years of age or younger presenting for safety evaluations are seen by a pediatric emergency medicine attending, often in conjunction with a trainee (either a pediatric resident or emergency medicine resident rotating through the pediatric ED), for medical evaluation and determination of the need for involuntary hold before evaluation by the psychiatry team. Although access to firearms is an important factor to assess when determining a patient’s risk of harm to self or others, we hypothesize that pediatric residents in the ED rarely assess and document this risk factor or provide counseling about risk reduction.
Methods
Design and Setting
We conducted a retrospective chart review of patients presenting to a single tertiary care ED in Boston, Massachusetts, that serves both pediatric and adult patients. We included visits of patients younger than 19 years of age who presented to the ED between January 1, 2016, and December 31, 2016, with a diagnosis of suicidal ideation, homicidal ideation, or suicide attempt as captured by International Statistical Classification of Diseases and Related Health Problems, 10th revision codes x71-x83, T14.91, and R45.85x. Identified patients were excluded if, on chart review, they were not evaluated by a pediatric resident during their visit. For example, this occurred if the patient was seen by an emergency medicine resident working in the pediatric ED or by an attending physician only.
For each eligible visit, the chart was reviewed manually by the lead investigator (C.N.L.) and data were entered into a secure online REDCap database (Research Electronic Data Capture, Vanderbilt, Tenn), hosted by the Partners Healthcare Information Systems. The study was approved by the Partners Human Research Committee Institutional Review Board.
Measures
The data extracted included patient demographics, medical and social history, and ED visit characteristics (including method of arrival and disposition). The co-primary outcomes were the proportion of visits in which there was documentation of patient access to firearms by any provider and documentation specifically by a pediatric resident. The secondary outcome was documentation of counseling about firearm risk reduction.
Data Analysis
Descriptive statistics were used to compare firearms assessment among patients based on patient and ED visit characteristics, as well as provider type. Categorical variables were reported as percentages with 95% confidence intervals and compared by Chi-square or Fisher exact tests. Statistical analyses were performed in SAS Software (Version 9.4; SAS Institute Inc, Cary, NC).
Results
In total, 139 patient visits were evaluated. Of these, 98 patients had a documented assessment by a pediatrics resident and were included in the analysis. The mean age was 14.3 years. The majority of patients were female (73.5%) and spoke English as their preferred language (87.8%). Most patients (94.9%) were authorized for temporary involuntary hospitalization. The reason for this involuntary hold was documented as suicidality in 84% of patients, homicidality in 5% of patients, both in 4%, and other in 7% (Table 1). In total, 33.7% of patients had a documented history of a previous suicide attempt. Patients arrived to the ED by ambulance in 32.7% of cases. Most patients (75.5%) were discharged to an inpatient psychiatry unit from the ED. In 17% of patient encounters, the authorization of temporary involuntary hospitalization was lifted and the patient was discharged directly home after the completion of the psychiatry evaluation (Fig. 1).
Table 1.
Patient Characteristics (n = 98)
| n | % | |
|---|---|---|
| Age, y | ||
| 0–9 | 2 | 2.0 |
| 10–14 | 47 | 48.0 |
| 15–17 | 49 | 50.0 |
| Sex (female) | 72 | 73.5 |
| Primary Language is English | 86 | 87.8 |
| Authorization of temporary involuntary hospitalization filed | 93 | 94.9 |
| Reason for authorization of involuntary hospitalization | ||
| Suicidality | 82 | 83.7 |
| Homicidiality | 5 | 5.1 |
| Other | 7 | 7.1 |
| Insurance | ||
| Private | 39 | 39.8 |
| Medicaid | 54 | 55.1 |
| Other/none | 5 | 5.1 |
| Documentation of substance use | ||
| Alcohol | 16 | 16.3 |
| Tobacco | 3 | 3.1 |
| Marijuana | 19 | 19.4 |
| Other | 8 | 8.2 |
| None documented | 70 | 71.4 |
| History of previous suicide attempt | 33 | 33.7 |
| ED visit characteristics | ||
| Method of arrival | ||
| Private car/public transport/walking | 33 | 33.7 |
| Ambulance | 32 | 32.7 |
| Other/unknown | 33 | 33.7 |
| Disposition | ||
| Home | 17 | 17.3 |
| Pediatric inpatient floor | 1 | 1.0 |
| Inpatient psychiatric unit | 74 | 75.5 |
| Other | 6 | 6.1 |
ED indicates emergency department.
Figure 1.
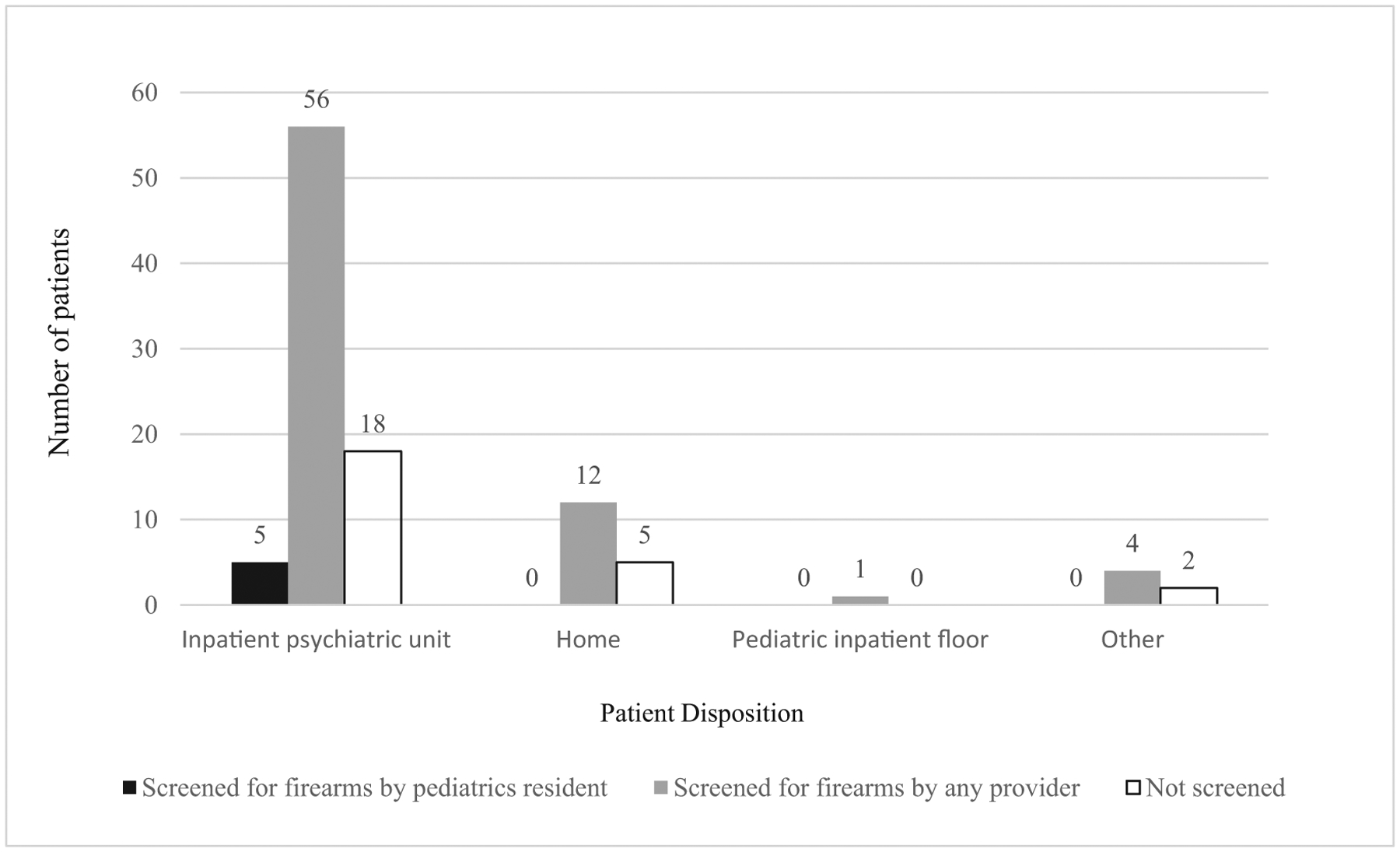
Patient disposition.
Of the 98 patients, 5 patients (5.1%) had documentation by the pediatric resident of screening for firearms access (Fig. 2). A total of 73 (74.5%) had documentation of screening for access to firearms during their ED stay by the psychiatry team (Fig. 2); all patients with documented screening by the pediatrics resident also had screening documented by the psychiatry team. No patient without documented screening by a pediatrics resident had screening documented by the pediatric emergency medicine attending. In 25 patients (25.5%), no documentation of access to firearms was present by any provider; and 5 patients (5.1%) were discharged to home without documented screening for access to firearms. One patient (1.0%) had documentation of counseling regarding firearms risk reduction (Table 2).
Figure 2.
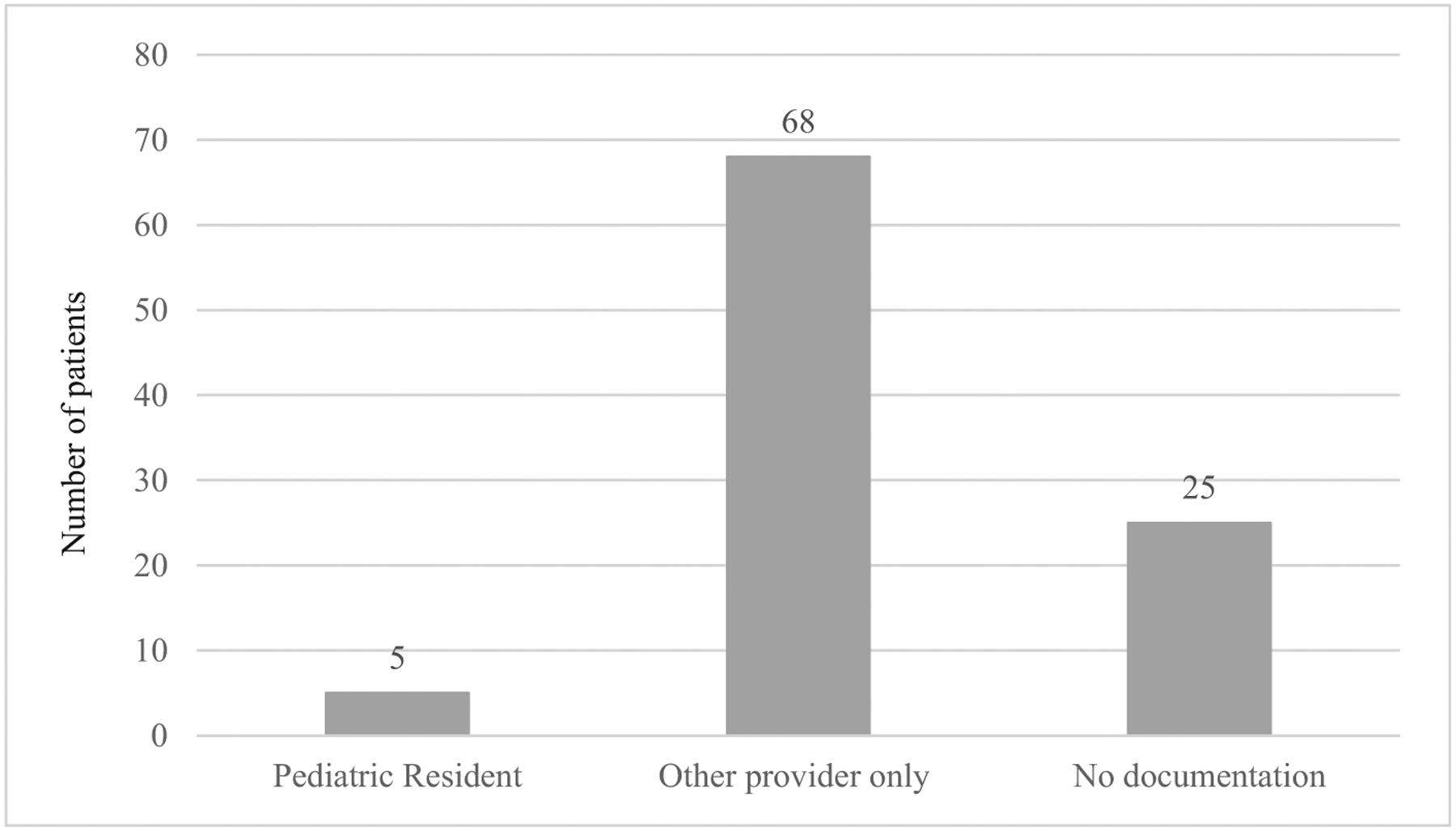
Firearms access screening by provider type.
Table 2.
Patient Characteristics by Documentation of Firearms Access Screening
| Demographic | Firearms Screening (n = 73) | No Firearms Screening (n = 25) | P Value |
|---|---|---|---|
| Age group, y | .57 | ||
| 0–9 | 1 | 1 | |
| 10–14 | 36 | 11 | |
| 15–17 | 36 | 13 | |
| Sex | .23 | ||
| Female | 53 | 19 | |
| Male/other | 20 | 6 | |
| Previous history of suicidality | 23 | 10 | .47 |
| Authorization for temporary involuntary hospitalization | 71 | 22 | .10 |
| Language | .48 | ||
| English | 62 | 24 | |
| Spanish/other | 11 | 1 | |
| Method of arrival | .01 | ||
| Ambulance | 29 | 3 | |
| Other | 44 | 22 | |
| Insurance type | .50 | ||
| Private | 26 | 13 | |
| Medicaid | 43 | 11 | |
| None | 1 | 0 | |
| Other | 3 | 1 | |
| Substance use disorder | .23 | ||
| None | 49 | 21 | |
| Alcohol | 4 | 2 | |
| Marijuana | 13 | 1 | |
| Other | 7 | 1 | |
| Disposition | .82 | ||
| Home | 12 | 5 | |
| Pediatric inpatient floor | 1 | 0 | |
| Inpatient psychiatric unit | 56 | 18 | |
| Other | 4 | 2 | |
| Documentation of firearms risk reduction counseling | 1 | 0 | 1.0 |
Patients who arrived by ambulance were significantly more likely to have documentation of firearms screening (odds ratio, 4.77; 95% confidence interval, 1.32−17.6; P = .01). Comparison of other categorical variables revealed no other significant association with documentation of firearms screening (Table 2).
Discussion
Pediatricians across levels of training nearly universally believe that it is their responsibility to reduce the risk of firearm-related injuries through screening and counseling of patients and parents about their risks.17–19 The majority of providers in the ED also believe that patients with active suicidal ideation always should be asked about their access to firearms.20 However, our findings indicate that these beliefs often do not translate into practice; pediatric residents rarely document screening for access to firearms in high-risk patients who present to the pediatric ED. Our results are in line with multiple previous studies that have found that pediatric residents do not effectively screen for access to firearms in outpatient settings,21–23 ED-based studies in which families reported that they never received risk-reduction counseling,24 and reports showing that ED providers have low rates of screening on both self-report12,20 and chart review.13,14,16
Our findings are especially concerning because 26% of patients had no documented screening about access to firearms by any provider during their visit, including 5 patients who were discharged directly home. Patients who arrived by ambulance were more likely to have documented screening for access to firearms by any provider than those arriving by other means (Table 2). We postulate that arrival by ambulance perhaps conferred a greater sense of urgency to the screening provider and patients may have been perceived to be at greater risk. No other variables in this study were found to be significant predictors of access to firearm screening during their visit. Pediatric trainees may assume that a patient’s access to lethal means will be assessed by other providers later in their visit, as previous research has shown that ED providers believe that this screening is the responsibility of the psychiatry team.12 These data demonstrate that although this was true in some cases, screening by the psychiatry team was not universal.
Although gun ownership in Massachusetts is below the national average, it is still estimated that 12.8% of Massachusetts households contain at least 1 firearm,25 and 2 families in our review who were asked about firearm access reported the presence of a firearm at home. A recent study found that a child’s history of mental illness did not influence caretaker decisions about having firearms in the home or storing them safely in accordance with the recommendations of the American Academy of Pediatrics,26 which may be due to the fact that many adults are unaware that having a firearm in the home increases the risk of completed suicide.27 Pediatricians have been shown to be ineffective at predicting which families own firearms18; therefore, universal firearms screening, especially in patients presenting with a demonstrated elevated risk of suicide or homicide, is critical.
Multiple barriers to screening previously have been identified, although data are limited and recent evidence is not available. Surveys of residents suggest that many feel they do not have adequate training to counsel on firearm safety.17,28 Only a fraction of residency training programs in the United States reported having formal training on firearm risk-reduction counseling as part of their standard curriculum.29,30 This deficiency is addressable. Multiple brief one-time interventions have been developed that have been shown to increase resident comfort with counseling about firearm safety with lasting efficacy.23,31 Data from other settings also have shown that the use of electronic medical record−based templates can increase rates of screening for firearms,32 but this strategy’s efficacy has not yet been reported in the resident population.
In addition, both pediatric residents and emergency medicine providers have expressed a sense of futility, perceiving that their screening and counseling was unlikely to have an impact.12,17,33 However, this too may be a point where further education is useful; although data are mixed, multiple studies have shown that physician counseling may have an observable impact on safe firearm storage practices.34–36
Our study has several limitations. Because of the retrospective design and chart review methodology, we may have missed instances in which a clinician asked about the presence of firearms in a patient’s home or counseled about lethal means restriction if these interactions were not documented in the medical record. The study period included the hospital’s transition between electronic medical records, which could have impacted documentation practices, and data from the single year reviewed for this study may not be representative of all patient interactions in our ED. Some patients presenting with suicidal or homicidal ideation may have had different International Statistical Classification of Diseases and Related Health Problems, 10th revision codes recorded on discharge and would not have been included in this cohort. In addition, as our data were collected at a single center in a state with a comparatively low prevalence of firearm ownership, the results may not be generalizable to pediatric residents in other programs or other areas of the country with different levels of or perceptions about gun ownership. Broader data collection will be important for further understanding the scope of the problem and designing life-saving interventions.
Conclusions
Pediatric residents rarely screen for access to firearms in high-risk patients in the ED, and many of these patients are not screened by other providers during their visit. The consequences of failing to recognize this significant, potentially modifiable risk factor for completed suicide or homicide can be devastating, and residency programs must work to prioritize training on this topic for pediatric residents.
What’s New.
This study is the first to examine rates of screening for access to firearms and counseling regarding risk reduction by pediatric trainees in patients with active suicidal or homicidal ideation presenting to the emergency department.
Acknowledgments
We thank the Massachusetts General Hospital Gun Violence Prevention Coalition, Trauma and Injury Prevention Outreach Program, and the pediatrics’ residency program for their support.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Miller M, Azrael D, Hemenway D. The epidemiology of case fatality rates for suicide in the northeast. Ann Emerg Med. 2004;43:723–730. [DOI] [PubMed] [Google Scholar]
- 2.Vyrostek SB, Annest JL, Ryan GW. Surveillance for fatal and non-fatal injuries—United States, 2001. MMWR Surveill Summ. 2004;53 (7):1–57. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). 2016. Available at: https://www.cdc.gov/injury/wisqars/index.html. Accessed March 3, 2018.
- 4.Dowd MD, Sege RD. Council on Injury, Violence, and Poison Prevention Executive Committee; American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2012;130:e1416–e1423. [DOI] [PubMed] [Google Scholar]
- 5.Brent DA, Perper JA, Allman CJ, et al. The presence and accessibility of firearms in the homes of adolescent suicides. A case-control study. JAMA. 1991;266:2989–2995. [PubMed] [Google Scholar]
- 6.Brent DA, Perper JA, Moritz G, et al. Firearms and adolescent suicide. A community case-control study. Am J Dis Child. 1993;147:1066–1071. [DOI] [PubMed] [Google Scholar]
- 7.Kellermann AL, Rivara FP, Somes G, et al. Suicide in the home in relation to gun ownership. N Engl J Med. 1992;327:467–472. [DOI] [PubMed] [Google Scholar]
- 8.Kellermann AL, Rivara FP, Rushforth NB, et al. Gun ownership as a risk factor for homicide in the home. N Engl J Med. 1993;329:1084–1091. [DOI] [PubMed] [Google Scholar]
- 9.Shain B Committee On Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2016;138(1). [DOI] [PubMed] [Google Scholar]
- 10.Committee on Injury and Poison Prevention. American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2000;105:888–895. [PubMed] [Google Scholar]
- 11.Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Acad Emerg Med. 2014;21:25–30. [DOI] [PubMed] [Google Scholar]
- 12.Betz ME, Miller M, Barber C, et al. Lethal means restriction for suicide prevention: beliefs and behaviors of emergency department providers. Depress Anxiety. 2013;30:1013–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Betz ME, Miller M, Barber C, et al. Lethal means access and assessment among suicidal emergency department patients. Depress Anxiety. 2016;33:502–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betz ME, Kautzman M, Segal DL, et al. Frequency of lethal means assessment among emergency department patients with a positive suicide risk screen. Psychiatry Res. 2017;260:30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Habis A, Tall L, Smith J, et al. Pediatric emergency medicine physicians’ current practices and beliefs regarding mental health screening. Pediatr Emerg Care. 2007;23:387–393. [DOI] [PubMed] [Google Scholar]
- 16.Giggie MA, Olvera RL, et al. Screening for risk factors associated with violence in pediatric patients presenting to a psychiatric emergency department. J Psychiatr Pract. 2007;13:246–252. [DOI] [PubMed] [Google Scholar]
- 17.Solomon BS, Duggan AK, Webster D, et al. Pediatric residents’ attitudes and behaviors related to counseling adolescents and their parents about firearm safety. Arch Pediatr Adolesc Med. 2002;156:769–775. [DOI] [PubMed] [Google Scholar]
- 18.Becher EC, Christakis NA. Firearm injury prevention counseling: are we missing the mark? Pediatrics. 1999;104:530–535. [DOI] [PubMed] [Google Scholar]
- 19.Olson LM, Christoffel KK, O’Connor KG. Pediatricians’ involvement in gun injury prevention. Inj Prev. 2007;13:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Betz ME, Barber CW, Miller M. Firearm restriction as suicide prevention: variation in belief and practice among providers in an urban emergency department. Inj Prev. 2010;16:278–281. [DOI] [PubMed] [Google Scholar]
- 21.Gielen AC, McDonald EM, Forrest CB, et al. Injury prevention counseling in an urban pediatric clinic. Analysis of audiotaped visits. Arch Pediatr Adolesc Med. 1997;151:146–151. [DOI] [PubMed] [Google Scholar]
- 22.Cohen LR, Runyan CW, Bowling JM. Social determinants of pediatric residents’ injury prevention counseling. Arch Pediatr Adolesc Med. 1998;152:169–175. [DOI] [PubMed] [Google Scholar]
- 23.Johnson CD, Fein JA, Campbell C, et al. Violence prevention in the primary care setting: a program for pediatric residents. Arch Pediatr Adolesc Med. 1999;153:531–535. [DOI] [PubMed] [Google Scholar]
- 24.McManus BL, Kruesi MJ, Dontes AE, et al. Child and adolescent suicide attempts: an opportunity for emergency departments to provide injury prevention education. Am J Emerg Med. 1997;15:357–360. [DOI] [PubMed] [Google Scholar]
- 25.Okoro CA, Nelson DE, Mercy JA, et al. Prevalence of household firearms and firearm-storage practices in the 50 states and the District of Columbia: findings from the Behavioral Risk Factor Surveillance System, 2002. Pediatrics. 2005;116:e370–e376. [DOI] [PubMed] [Google Scholar]
- 26.Scott J, Azrael D, Miller M. Firearm storage in homes with children with self-harm risk factors. Pediatrics. 2018. [DOI] [PubMed] [Google Scholar]
- 27.Conner A, Azrael D, Miller M. Public opinion about the relationship between firearm availability and suicide: results from a national survey. Ann Intern Med. 2018;168:153–155. [DOI] [PubMed] [Google Scholar]
- 28.Wright MS. Pediatric injury prevention. Preparing residents for patient counseling. Arch Pediatr Adolesc Med. 1997;151:1039–1043. [DOI] [PubMed] [Google Scholar]
- 29.Price JH, Conley PM, Oden L. Training in firearm safety counseling in pediatric residency programs. Arch Pediatr Adolesc Med. 1997;151:306–310. [DOI] [PubMed] [Google Scholar]
- 30.Zavoski RW, Burke GS, Lapidus GD, et al. Injury prevention training in pediatric residency programs. Arch Pediatr Adolesc Med. 1996;150:1093–1096. [DOI] [PubMed] [Google Scholar]
- 31.Dingeldein L, Sheehan K, Krcmarik M, et al. Evaluation of a firearm injury prevention web-based curriculum. Teach Learn Med. 2012;24:327–333. [DOI] [PubMed] [Google Scholar]
- 32.LoConte NK, Gleason CE, Gunter-Hunt G, et al. Standardized note template improves screening of firearm access and driving among veterans with dementia. Am J Alzheimers Dis Other Demen. 2008;23:313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Price JH, Thompson A, Khubchandani J, et al. Perceived roles of Emergency Department physicians regarding anticipatory guidance on firearm safety. J Emerg Med. 2013;44:1007–1016. [DOI] [PubMed] [Google Scholar]
- 34.Kruesi MJ, Grossman J, Pennington JM, et al. Suicide and violence prevention: parent education in the emergency department. J Am Acad Child Adolesc Psychiatry. 1999;38:250–255. [DOI] [PubMed] [Google Scholar]
- 35.Carbone PS, Clemens CJ, Ball TM. Effectiveness of gun-safety counseling and a gun lock giveaway in a Hispanic community. Arch Pediatr Adolesc Med. 2005;159:1049–1054. [DOI] [PubMed] [Google Scholar]
- 36.Barkin SL, Finch SA, Ip EH, et al. Is office-based counseling about media use, timeouts, and firearm storage effective? Results from a cluster-randomized, controlled trial. Pediatrics. 2008;122:e15–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]


