FIGURE 14.
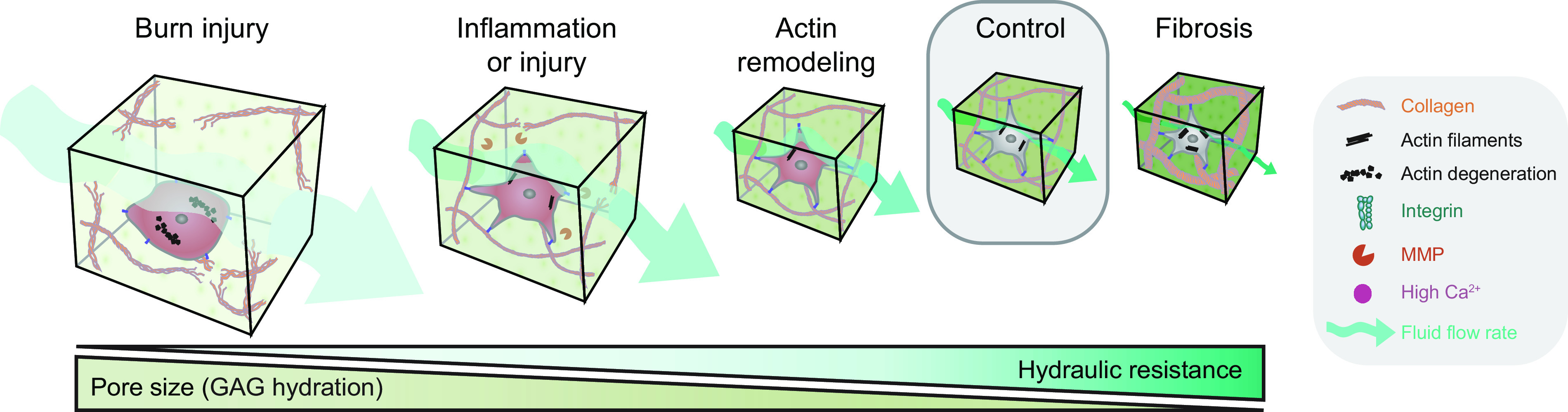
Glycosaminoglycans (GAGs) swell in the setting of injury and increases tissue fluid flow. During normal physiological conditions, solid elements in the extracellular space, including collagen, as well as the cellular tension, together limit GAG hydration in peripheral tissue (355). After a burn injury, the degradation and conformational changes of collagen and cellular elements lead to rapid influx of vascular fluid resulting in massive swelling and an enormous increase in GAG hydration (204, 344, 358, 359). Tissue swelling is slower in onset and less severe in the setting of inflammation or tissue injury. In these conditions, matrix metalloproteinases (MMPs) are activated, resulting in a breakdown of the fibrillar extracellular matrix proteins and interruption of cellular adhesion complexes, mainly integrins. The resultant decrease in tissue tension leads to an increase in GAG hydration and tissue swelling. Ca2+ signaling in the setting of tissue injury can also be associated with a breakdown of the actin cytoskeleton and thus result in a more modest increase in GAG hydration (360). In fibrotic scar tissue, the relative amounts of the fibrillar extracellular matrix structures and the actin cytoskeleton increase, thus placing GAGs under additional pressure and reducing their hydration. Indeed, hydraulic resistance has an inverse relationship with GAG hydration. The more water that GAGs bind, the lower their resistance to flow, resulting in an increase in convective flow. On the other hand, fibrosis reduces the tissue fluid flow rate.
