1. CASE PRESENTATION
A 58‐year‐old male with a history of diabetes and hypertension was brought to the emergency department (ED) for evaluation of altered mental status. Upon arrival, the patient was ill appearing, encephalopathic, and with the following vital signs: temperature 37.2°C, blood pressure 121/89 mmHg, heart rate 168 beats/min, respiratory rate 28 breaths/min, and oxygen saturation 98% on a nonrebreather mask. Physical examination revealed extensive tenderness and erythema of the distal right lower extremity with associated ecchymosis and necrotic tissue of the medial‐plantar aspect of the right foot (Figure 1). Bedside soft tissue point‐of‐care ultrasound (POCUS) was subsequently performed, which demonstrated hyperechoic air foci with dirty posterior shadowing and perifascial fluid accumulation consistent with necrotizing fasciitis (Figure 2). Orthopedic surgery was immediately consulted based on the abnormal POCUS findings. The patient was further resuscitated with intravenous fluids and empiric antibiotics, and orthopedic surgery emergently brought the patient to the operating room for a right below‐knee amputation.
FIGURE 1.

Physical examination of the distal right lower extremity revealing extensive erythema with ecchymosis and necrotic tissue of the medial‐plantar aspect of the right foot
FIGURE 2.
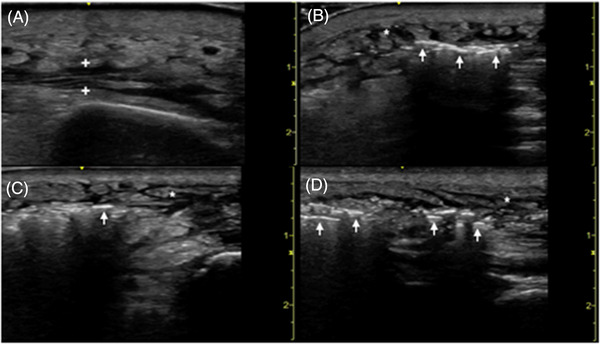
Point‐of‐care ultrasound of the affected right tibia in a transverse (A) plane demonstrating perifascial fluid accumulation (between plus symbols). Point‐of‐care ultrasound of the affected right foot in transverse (B,C) and longitudinal (D) planes demonstrating hyperechoic air foci (arrows) with dirty posterior shadowing representative of necrotizing fasciitis. Subcutaneous edema (asterisks) clinically consistent with overlying cellulitis
2. DIAGNOSIS
2.1. Necrotizing fasciitis
Necrotizing fasciitis is a time‐sensitive, life‐threatening skin and soft tissue infection that necessitates early identification in the ED. 1 , 2 Clinical examination and plain radiography findings are poorly sensitive for detecting necrotizing fasciitis; therefore, prompt diagnosis is notoriously challenging. 3 There is an emerging role for POCUS performed by emergency physicians as an alternative diagnostic modality for necrotizing fasciitis, with high sensitivity and specificity previously reported. 4 , 5 The sonographic features of necrotizing fasciitis may include the presence of the following: diffuse thickening of subcutaneous tissue, irregular fascial planes with perifascial fluid accumulation, and air foci with dirty posterior shadowing. 6 , 7 , 8 , 9 , 10 Critically, POCUS was instrumental in our case to yielding a rapid diagnosis and expedited surgical management without obtaining further advanced gold standard imaging. This report highlights the decisive role of emergency physician‐performed POCUS ultrasound as a first‐line bedside screening tool in the ED diagnosis of necrotizing fasciitis.
Pramanik I, Domozick A, Jackson J, Cabrera Correa G, Acevedo HG, Kalivoda EJ. Point‐of‐care ultrasound evaluation of lower extremity erythema. JACEP Open. 2022;3:e12691. 10.1002/emp2.12691
Disclaimer: This research was supported in part by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
REFERENCES
- 1. Hefny AF, Eid HO, Al‐Hussona M, et al. Necrotizing fasciitis: a challenging diagnosis. Eur J Emerg Med. 2007;14(1):50‐52. [DOI] [PubMed] [Google Scholar]
- 2. Kaafarani HMA, King DR. Necrotizing skin and soft tissue infections. Surg Clin North Am. 2014;94(1):155‐163. [DOI] [PubMed] [Google Scholar]
- 3. Fernando SM, Tran A, Cheng W, et al. Necrotizing soft tissue infection: diagnostic accuracy of physical examination, imaging, and LRINEC score. Ann Surg. 2019;269(1):58‐65. [DOI] [PubMed] [Google Scholar]
- 4. Yen ZS, Wang HP, Ma HM, et al. Ultrasonographic screening of clinically‐suspected necrotizing fasciitis. Acad Emerg Med. 2002;9(12):1448‐1451. [DOI] [PubMed] [Google Scholar]
- 5. Lahham S, Shniter I, Desai M, et al. Point of care ultrasound in the diagnosis of necrotizing fasciitis. Am J Emerg Med. 2022;51:397‐400. [DOI] [PubMed] [Google Scholar]
- 6. Hosek WT, Laeger TC. Early diagnosis of necrotizing fasciitis with soft tissue ultrasound. Acad Emerg Med. 2009;16(10):1033. [DOI] [PubMed] [Google Scholar]
- 7. Oelze L, Wu S, Carnell J. Emergency ultrasonography for the early diagnosis of necrotizing fasciitis: a case series from the ED. Am J Emerg Med. 2013;31(3):632.e5‐7. [DOI] [PubMed] [Google Scholar]
- 8. Castleberg E, Jenson N, Dinh VA. Diagnosis of necrotizing fasciitis with bedside ultrasound: the STAFF exam. West J Emerg Med. 2014;15(1):111‐113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shyy W, Knight RS, Goldstein R, et al. Sonographic findings in necrotizing fasciitis: two ends of the spectrum. J Ultrasound Med. 2016;35(10):2273‐2277. [DOI] [PubMed] [Google Scholar]
- 10. Klein J, Sodhi S, Cheng A, et al. Female with leg pain. Ann Emerg Med. 2019;74(6):e113‐e114. [DOI] [PubMed] [Google Scholar]


