Abstract
STUDY DESIGN:
Prospective cohort study, cross-sectional design.
BACKGROUND:
The hip-spine syndrome is described in patients with known arthritis of the hip. This study describes the hip examination findings of people presenting with low back pain (LBP).
OBJECTIVES:
To (1) report examination findings of the hip in patients with LBP and (2) compare pain and function in patients with positive hip examination findings to those in patients without positive hip examination findings.
METHODS:
An examination and validated questionnaires of spine and hip pain and function were completed. Pain and function scores were compared between patients with and without positive hip findings.
RESULTS:
Consecutive patients (68 women, 33 men) with a mean age of 47.6 years (range, 18.4–79.8 years) participated. On physical examination, 81 (80%) had reduced hip flexion; 76 (75%) had reduced hip internal rotation; and 25 (25%) had 1, 32 (32%) had 2, and 23 (23%) had 3 positive provocative hip tests. Patients with reduced hip flexion had worse LBP-related (mean modified Oswestry Disability Index, 35.3 versus 25.6; P = .04) and hip-related function (mean modified Harris Hip Score, 66.0 versus 82.0; P = .03). Patients with reduced hip internal rotation had worse LBP-related function (mean Roland-Morris questionnaire, 12.4 versus 8.2; P = .003). A positive provocative hip test was coupled with more intense pain (median, 9 versus 7; P = .05) and worse LBP-related (mean Roland-Morris questionnaire, 12.1 versus 8.5; P = .02) and hip-related function (mean modified Harris Hip Score, 65.8 versus 89.7; P = .005).
CONCLUSION:
Physical examination findings indicating hip dysfunction are common in patients presenting with LBP. Patients with LBP and positive hip examination findings have more pain and worse function compared to patients with LBP but without positive hip examination findings.
LEVEL OF EVIDENCE:
Symptom prevalence, level 1b.
Keywords: developmental hip dysplasia, femoroacetabular impingement, hip osteoarthritis, hip-spine syndrome, low back pain
The etiology of low back pain (LBP) is not well understood. Researchers and clinicians have focused on better understanding LBP by studying and treating presumed lumbar structural sources and their coincident biomechanical and physiological changes. This focus has continued, despite evidence that people without LBP have structural changes of their lumbar spine.4 Even less is understood regarding LBP in patients without structural changes on imaging studies of the lumbar spine. Experts in the assessment of movement have developed models to group people with LBP based on movement and alignment patterns that provoke and relieve symptoms, regardless of structural changes in the lumbar spine.13,18,60 Long and colleagues31 used one of these models and performed a standardized mechanical assessment on 312 patients with LBP, with and without sciatica. They were able to successfully subgroup 230 (74%) of these patients. Despite the success of this method of assessment, 26% of the patients did not fit into a subgroup. So the question remains: how do health care providers best assess people with LBP in order to develop a specific and successful treatment recommendation? Might we look beyond the spinal column for the source of, or contributor to, pain and loss of function?
The pain distributions that patients report for lumbar spine disorders can be similar and overlap with those related to disorders of the pelvic girdle and hip.17,30 The overlap in pain distributions can contribute to the difficulty in making an accurate diagnosis. Like the lumbar spine, the hip can also present with a broad distribution of pain. Lesher and colleagues30 described 12 different patterns of distribution of hip pain that responded to an image-guided intra-articular hip injection used to identify symptomatic hip osteoarthritis (OA). Of those patients who reported 90% or greater improvement following the injection, the most common distribution of pain was in the buttock and posterior thigh, atypical of the expected groin and lateral hip distribution for hip OA. Khan et al28 reported that 47% of patients treated for hip OA complained of pain below the knee, a distribution commonly attributed to a lumbar spine disorder. Clearly, at the time of presentation, hip pain can present with similar pain distributions as a disorder of the lumbar spine.
In addition to overlapping pain distributions, hip and spine disorders have been found to coexist. Offierski and MacNab41 described these coexisting disorders and coined the term hip-spine syndrome. The authors proposed that patients with the hip-spine syndrome could be subgrouped into simple (either the hip or the spine was the source of pain and dysfunction), complex (both the hip and the lumbar spine were symptomatic and the source of pain and dysfunction), or secondary (the dysfunction of one region was interrelated with the dysfunction of the other region). Studies describing the hip-spine syndrome have primarily included patients with degenerative disorders of the hip and spine.3,5,16,36,41,45,49,50 Ben-Galim and colleagues3 were the first to prospectively report treatment outcomes in patients with the hip-spine syndrome. They described pain and functional improvements in LBP in 25 patients treated with total hip replacement (THR) for hip pain due to OA. A retrospective study45 of 3335 patients receiving a THR for OA found that 17% of patients were evaluated for complaints of LBP within 2 years before or after their THR. Those who were evaluated for LBP reported greater pain and loss of function following THR compared to patients treated with THR alone. In addition, patients with THR and complaints of LBP required treatment for a longer duration, and treatment was more costly compared to patients treated with THR alone.
There is emerging evidence that LBP coexists with intra-articular hip disorders that occur prior to the onset of hip OA.6,12,40,44 These disorders include hip deformities (femoroacetabular impingement [FAI] and developmental hip dysplasia) with or without acetabular labral tears. Clohisy and colleagues12 reported that, in addition to groin and lateral hip pain, 23% of patients surgically treated for symptomatic FAI also reported LBP at the time of their initial presentation. Buttock pain (a distribution of pain that overlaps spine disorders with the pelvic girdle and hip disorders) was also reported in patients treated surgically for FAI (29%),12 developmental hip dysplasia (17%),40 and acetabular labral tears (38%).6 Though not reported, one can speculate that the hip-spine syndrome may include a spectrum of disorders that can begin prior to the onset of degenerative changes in the hip and spine and continue to the end of the spectrum, which includes hip OA and spinal stenosis.
A better understanding of the hip-spine syndrome may lead to improved diagnostic tests and, ultimately, treatment. Further, improved knowledge of the relationship between the hip and the lumbar spine will provide avenues of investigation for patients presenting with LBP of unclear etiology. Better recognition by health care providers that both disorders can coexist will improve treatment recommendations, which should involve both the hip and the lumbar spine.
Previous studies have assessed the hip physical examination in people with LBP, including hip range of motion (ROM),47,54,56,59 lumbopelvic motion with hip motion,22,23,25,47,48,57 and the relationship of relief of LBP following total hip arthroplasty for OA.3,10,26,51,52 To date, data regarding patient characteristics and hip and lumbar spine pain and function measures, combined with multiple physical examination assessments of the lumbar spine and hip, are not readily available in one study. The objectives of this study were to (1) prospectively collect observational cross-sectional data regarding patient characteristics and hip physical examination findings in patients presenting for evaluation and treatment of LBP, and (2) compare pain and function in patients with positive hip examination findings to those in patients without positive hip examination findings.
METHODS
Participants
After approval by the Washington University in St Louis Human Research Protection Office, consecutive patients who presented to the physical medicine and rehabilitation service at a tertiary university orthopaedic department for evaluation and treatment of LBP were recruited by a research assistant at the initial appointment, prior to meeting the physician. The research assistant reviewed the patients’ demographics and past medical and surgical history on a questionnaire that is used routinely for all patients evaluated in this orthopaedic surgery department. Recruitment occurred over 2 separate 8-week periods, when a research assistant was available. Patients were asked to be in the study if they were 18 years of age or older and had LBP symptoms for more than 4 weeks. Patients were not asked to be in the study if they were pregnant; had a history of tumor, fracture, or surgery involving the lumbar spine, pelvis, or hip; or had a history of spondyloarthropathy or inflammatory arthropathy. All patients who met the inclusion criteria agreed to participate. Informed consent was received by every participant and the rights of the subjects were protected. Observational cross-sectional data regarding the recruited patients were collected at their initial examination, and no follow-up data were collected.
Pain and Function Measurements
Patients completed a standardized set of questionnaires that included a medical and surgical history, a body pain diagram, and a numeric pain-rating scale (NPRS) to rate the least, average, and worst pain experienced over the 7 days prior to the examination. The modified Oswestry Disability Index (mODI)19 and the Roland-Morris questionnaire (RMQ)46 were used to assess a patient’s LBP-related function. The University of California at Los Angeles activity scale2 and the modified Harris Hip Score (mHHS)8 were used to assess activity and hip-related function, respectively. Patients marked the locations of the pain for which they were seeking treatment on the body pain diagram. To ensure consistency in reporting, the research assistant placed an overlay on the body pain diagram that specified anatomic locations (eg, lumbar spine, lateral hip, and groin). The research assistant assisted patients in completing the intake forms upon request.
History and Physical Examination
The history taking and physical examination were performed by a physiatrist (H.P.) with experience in the evaluation and treatment of musculoskeletal conditions. The research assistant recorded all physical examination findings as the physiatrist performed the examination. As part of the history, patients were asked what activities incited the pain for which they were seeking treatment. In addition, patients were asked specifically about pain with standing, sitting, moving from sit to stand, pivoting, leg crossing in sitting, and trunk flexion and extension. The physical examination included selected tests that are standard of care for evaluating the neurological and musculoskeletal systems. The examination included assessment of gait, muscle strength, muscle stretch reflexes, sensation, single-leg stance, pain provocation with lumbar active ROM, neural tension, hip ROM, and selected provocative tests for the hip. If an antalgic gait was observed, the side of the gait abnormality was recorded. Muscle strength, muscle stretch reflexes, and sensation were assessed using methods consistent with the standard of care for a clinical examination.33 The patient was asked to complete a single-leg stance and then asked if this position reproduced his or her pain. To assess the direction(s) of lumbar spine movement that provoked pain, the patient was instructed to actively perform flexion, extension, and sidebending in standing. The patients were questioned after performing each motion if they experienced pain, and the response was recorded for each motion.31 A slump-sit test was performed while the patient was seated with the shoulders internally rotated and extended.7,33 Peroneal bias was added to the slump position by passively internally rotating the leg, plantar flexing the ankle, and inverting the foot. Tibial bias was added to the slump-sit position by passively externally rotating the lower extremity, dorsiflexing the ankle, and everting the foot.7 The patient was asked whether the test reproduced pain in the lower extremity, and the response was recorded for each side. A femoral nerve stretch test was performed with the patient in prone. The knee was passively flexed by the examiner while the pelvis was stabilized with her other hand. The patient’s response was recorded in the same manner as for the slump-sit test.
Passive hip ROM was measured with a goniometer using standardized methods.20,37,39 The passive hip motions tested included hip flexion, hip internal rotation (IR) with the hip flexed to 90°, and hip external rotation (ER) with the hip flexed to 90°. These motions were chosen because they are known to be altered in patients with hip deformity6,12 and OA.21,55 In a previous study,43 the authors demonstrated excellent intrarater reliability (intraclass correlation coefficient = 0.76–0.97) and good to excellent interrater reliability (intraclass correlation coefficient = 0.63–0.87) for these hip ROM assessments among multiple examiners. In a prior study, these ROM measures were obtained from 50 (25 women and 25 men) healthy, asymptomatic volunteers between the ages of 18 and 50 years. The data were analyzed by sex because hip ROM differs between sexes.43 The prior healthy volunteer data set was used to classify the patients with LBP in the current study into 2 sex-based groups (normal or reduced hip ROM) for each of the 3 hip motions. In the healthy, asymptomatic volunteer study, the mean value for hip flexion ROM for women was 112° and for men was 103°. The mean values for hip flexion and IR were 31° for women and 18° for men. The mean values for hip flexion and ER were 42° for women and 42° for men.
Provocative hip tests to identify intra-articular hip disorders32,35 included the anterior hip impingement test; the flexion, abduction, external rotation (FABER) test; and the log-roll test. Two authors of the current study (H.P. and K.S.M.) have previously reported excellent interrater and intrarater agreement of provocative hip tests in asymptomatic adults.43 The anterior hip impingement test was performed with the patient in supine. The examiner passively moved the hip into 90° of flexion and maximal IR and adduction. The FABER test was performed with the patient in supine. The examiner passively moved the hip into flexion, abduction, and ER. The log-roll test was performed with the patient in supine. The examiner passively moved the hip into IR and ER with the hip in a neutral position. While performing the provocative hip tests, lumbar spine movement was limited by having the examiner place one hand on the pelvis opposite the side being tested. The patient was asked to report whether the test reproduced his or her pain, and to identify the location of the pain. The test was recorded as positive if the test provoked pain in the groin, lateral hip, low back, or posterior pelvis.
Analysis
For normally distributed continuous data, summary statistics are reported as mean ± SD. Ordinal scaled or nonnormally distributed continuous variables are reported as median, with the interquartile range defined as the 25th to 75th percentile. Categorical variables are reported as the number of patients (percent of group). Range of motion is reported as the mean of up to 3 testing trials. Separately for the right and left limbs, ROM measurements were compared for men and women by unpaired t tests. Patients were classified as having normal ROM when ROM in both limbs was equal to or above previously reported, sex-specific, asymptomatic mean ROM values43 or as having reduced ROM when ROM in at least 1 limb was below previously reported, sex-specific, asymptomatic mean ROM values. The proportion of patients with normal ROM was compared for men and women by chi-square tests, unless the sample size was small, in which case Fisher’s exact test was used. To determine whether pain, function, and activity were similar in patients with normal versus reduced ROM, pain, function, and activity measures were compared by unpaired t tests or Wilcoxon tests (when the assumptions for t tests were not satisfied). Patients were classified as having a positive provocative hip exam when they reported an increase in symptoms in either limb, as assessed by the hip impingement, FABER, or log-roll test. Pain, function, and activity were compared between patients with and without a positive provocative hip test by unpaired t tests or Wilcoxon tests. Analyses were performed in each limb, and, for clarity, the results from the most impaired limb were reported. Differences in measures were compared to published minimal detectable difference values (NPRS and mODI)15,34 and minimal clinically important difference values (NPRS, mODI, RMQ).19,34,42
RESULTS
Participant Characteristics, Pain, Function, and Activity at Presentation
One hundred one consecutive patients met the inclusion criteria and agreed to participate. The demographic characteristics, baseline pain, lumbar spine and hip function, and activity scores of the 101 participants are provided in TABLE 1. The baseline pain, function, and activity scores indicated that patients were limited. The locations of pain marked by patients on the body pain diagram were consistent with many lumbar spine disorders (FIGURE).
TABLE 1.
Patient Characteristics, Self-report Scores for Pain and Function, and Self-report of Pain-Provoking Activities (n = 101)*
| Variable | Value |
|---|---|
| Patient demographics | |
| Sex (female), n (%) | 68 (67) |
| Race (Caucasian), n (%) | 88 (87) |
| Age, y | 47.6 ± 14 |
| Body mass index, kg/m2 | 28.9 ± 8 |
| Current duration of low back pain, mo†‡ | 6 (2, 16) |
| NPRS† | |
| Average pain | 4 (3, 6) |
| Worst pain | 9 (7, 10) |
| Least pain | 2 (0, 4) |
| Lumbar spine and hip function questionnaires | |
| Modified ODI | 34.5 ± 18 |
| UCLA activity scale† | 5 (4, 7) |
| RMQ | 11.4 ± 6 |
| Modified HHS | 69.7 ± 21 |
| Pain-provoking activities (self-report), n (%) | |
| Pivoting | 73 (72) |
| Sitting | 72 (71) |
| Transition | 71 (70) |
| Weight bearing (standing) | 70 (69) |
| Lumbar flexion (bending forward) | 50 (50) |
| Crossing legs | 48 (48) |
| Lumbar extension (arching backward) | 60 (59) |
Abbreviation: HHS, Harris Hip Score; NPRS, numeric pain-rating scale; ODI, Oswestry Disability Index; RMQ, Roland-Morris questionnaire; UCLA, University of California at Los Angeles.
Values are mean ± SD unless otherwise indicated.
Values are median (interquartile range [25th, 75th percentile]).
Data missing for 8 patients.
FIGURE.
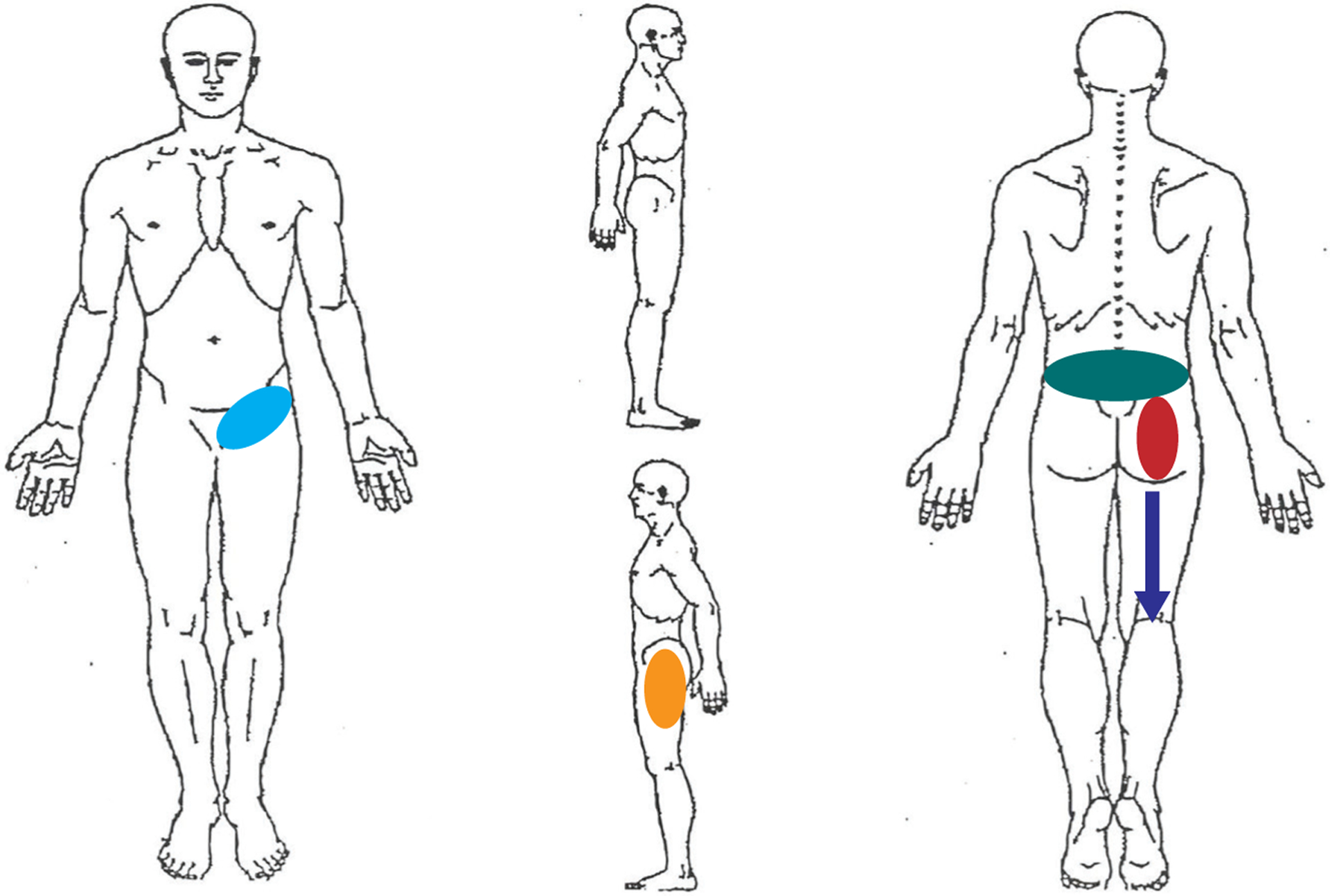
Distribution of pain, self-reported by the patient. The percentages listed denote the percentage of patients who marked this area to be painful. Light blue: groin, n = 35 of 101 (35%). Orange: lateral hip, n = 50 of 101 (50%). Green: L5 and superior, n = 100 of 101 (99%). Red: distal to L5 and proximal to the gluteal fold, n = 67 of 101 (66%). Dark blue: below the gluteal fold, n = 71 of 101 (70%).
Physical Examination Findings
Of 101 patients, 25 (25%) displayed an antalgic gait and 34 (34%) reported pain with single-leg stance. Physical examination findings were consistent with lumbar spine disorders (TABLE 2). Hip passive ROM measures for each side for female and male patients with LBP were compared, and the side with the greatest limitation is reported (TABLE 3). Mean hip flexion was significantly less for men compared to women (approximately 97° for men and 102° for women, P<.001). Mean hip IR with the hip flexed to 90° also was significantly less for men compared to women (approximately 12.5° in men and 19° in women, P<.001). Finally, mean left hip ER with the hip flexed to 90° was less, but not statistically significantly less, for men compared to women (39.5° in men and 43° in women, P = .07). The percentages of female and male patients with LBP with normal hip ROM compared to the prior sample of asymptomatic healthy volunteers43 also are presented in TABLE 3. Significantly more men than women had normal hip flexion ROM (30% versus 10%, P = .008) and hip IR with the hip flexed to 90° (39% versus 18%, P = .02), but not hip ER with the hip flexed to 90° (70% versus 81%, P = .21). Overall, hip flexion was reduced in 81 patients, hip IR with the hip flexed to 90° was reduced in 76 patients, and hip ER with the hip flexed to 90° was reduced in 23 patients.
TABLE 2.
Lumbar Spine Tests That Provoked the Patient’s Symptoms (n = 101)*
| Variable | Value |
|---|---|
| Pain with lumbar flexion | 43 (43) |
| Pain with lumbar extension | 60 (59) |
| Pain with lumbar sidebending: right | 32 (32) |
| Pain with lumbar sidebending: left | 35 (35) |
| Femoral nerve test | |
| No | 85 (84) |
| Yes: bilateral | 5 (5) |
| Yes: left | 2 (2) |
| Yes: right | 6 (6) |
| Unable to perform† | 3 (3) |
| Slump-sit test | |
| Peroneal bias: no | 59 (58) |
| Yes: bilateral | 6 (6) |
| Yes: left | 18 (18) |
| Yes: right | 16 (16) |
| Unable to perform† | 2 (2) |
| Slump-sit tibial bias‡ | |
| No | 48 (48) |
| Yes: bilateral | 17 (17) |
| Yes: left | 15 (15) |
| Yes: right | 18 (18) |
| Unable to perform† | 2 (2) |
Values are n (%).
Indicates that the test was not fully completed because the patient reported severe pain when the test was initiated.
Data missing for 1 patient.
TABLE 3.
Passive Hip Range of Motion for the Most Impaired Limb in Patients Presenting for Evaluation of LBP, by Sex (n = 101)*
| Sex | |||
|---|---|---|---|
| Variable | Women (n = 68)† | Men (n = 33)‡ | P Value§ |
| Hip flexion, deg∥ | 102 ± 7 | 97.3 ± 5 | <.001 |
| Hip flexion IR, deg | 19.1 ± 7 | 12.5 ± 8 | <.001 |
| Hip flexion ER, deg | 42.9 ± 8 | 39.5 ± 9 | .07 |
| Normal hip flexion, n (%)∥¶ | 7 (10) | 10 (30) | .008 |
| Normal hip flexion IR, n (%)¶ | 12 (18) | 13 (39) | .02 |
| Normal hip flexion ER, n (%)¶ | 55 (81) | 23 (70) | .21 |
Abbreviations: ER, external rotation; IR, internal rotation; LBP, low back pain.
Values are mean ± SD unless otherwise indicated.
Mean ± SD age, 47.6 ± 13.0 years (range, 22.3–77.4 years).
Mean ± SD age, 47.4 ± 16.2 years (range, 18.4–79.8 years).
Compares women to men by unpaired t test (for continuous variables) or chi-square test (for categorical variables).
Data missing for both sides of 1 woman, both sides of 1 man, and the right side of 1 man.
Compared to the sex-specific asymptomatic mean.
Provocative hip tests were considered positive when the test reproduced pain in any of the following regions: groin, lateral hip, and buttocks. Positive provocative hip test findings were as follows: (1) 65 of 101 (64%) had a positive hip impingement test, (2) 60 of 101 (59%) had a positive FABER test, and (3) 33 of 101 (33%) had a positive log-roll test. The frequency and percentage of positive provocative hip tests are reported in TABLE 4. Only 21 of 101 (21%) of the patients did not have at least 1 positive provocative hip test.
TABLE 4.
Hip Tests That Provoked the Patient’s Symptoms (n = 101)*
| Sum of Positive Provocative Hip Tests† | Value |
|---|---|
| 0 | 21 (21) |
| 1 | 25 (25) |
| 2 | 32 (32) |
| 3 | 23 (23) |
Values are n (%).
Tests specific for the hip include (for either side): hip impingement; flexion, abduction, external rotation; and log roll. Unable to perform indicated that the test was not fully completed because the patient reported severe pain at the initiation of the test and was recorded as a positive test.
Association of Pain, Function, and Activity Measures With Hip ROM and Provocative Hip Tests
TABLE 5 provides a comparison of the pain, function, and activity scores for patients with LBP who had (1) normal passive hip ROM based on the values of asymptomatic adults, and (2) reduced passive hip ROM based on the values of asymptomatic adults. Patients with reduced hip flexion had higher mODI (P = .04) and lower mHHS (P = .03) scores compared to those without reduced hip flexion. This reached the minimal clinically important difference (6 or greater) for the mODI.19 Patients with reduced hip IR with the hip flexed to 90° had significantly higher RMQ scores (P = .003) compared to those without reduced hip IR. This reached the minimal clinically important difference of 3.5 or greater.42 However, no significant differences were found in the mODI (P = .12) and University of California at Los Angeles activity scale (P = .10) scores for patients with and without reduced hip IR with the hip flexed to 90°. However, minimal detectable differences in the mODI (10% or greater)15 were found when comparing the results of all measures in patients with reduced hip ROM to the results of patients without reduced hip ROM. Minimal clinically important differences (6 or greater) in the mODI19 were found when comparing patients with reduced hip flexion and internal ROM to those without reduced hip ROM. No statistical differences in pain were noted in patients with hip ROM limitations as compared to those without hip ROM limitations (all, P>.05). No significant differences were found in function and in activity in patients with reduced hip ER with the hip flexed to 90° compared to patients with normal hip ER with the hip flexed to 90° (all, P>.05).
TABLE 5.
For Each ROM Test, Comparison of Clinical Outcomes for Patients With Reduced Versus Normal ROM (n = 101)*
| Variable | Reduced† | Normal† | P Value‡ |
|---|---|---|---|
| Hip flexion§ | |||
| Average NPRS∥ | 4 (3, 7) | 4 (3, 5) | .32¶ |
| Worst NPRS∥ | 9 (7, 10) | 8 (6, 8) | .06¶ |
| Least NPRS∥ | 2 (0, 4) | 1 (0, 2) | .25¶ |
| Modified ODI | 35.3 ± 18 | 25.6 ± 15 | .04#** |
| UCLA activity scale∥ | 5 (4, 6) | 6 (4, 8) | .28¶ |
| Roland-Morris questionnaire | 11.6 ± 6 | 8.8 ± 5 | .10 |
| Modified HHS | 66.0 ± 21 | 82.0 ± 16 | .03 |
| Hip flexion IR†† | |||
| Average NPRS∥ | 4 (3, 6) | 5 (3, 7) | .93¶ |
| Worst NPRS∥ | 9 (7, 10) | 8 (7, 9) | .12¶ |
| Least NPRS∥ | 2 (0, 4) | 2 (0, 5) | .53¶ |
| Modified ODI | 36.1 ± 16 | 29.6 ± 22 | .12#** |
| UCLA activity scale∥ | 5 (4, 6) | 6 (4, 9) | .10¶ |
| Roland-Morris questionnaire | 12.4 ± 6 | 8.2 ± 6 | .003** |
| Modified HHS | 65.1 ± 21 | 76.0 ± 20 | .10 |
| Hip flexion ER‡‡ | |||
| Average NPRS∥ | 5 (4, 7) | 4 (3, 6) | .28¶ |
| Worst NPRS∥ | 9 (7, 10) | 9 (7, 10) | .63¶ |
| Least NPRS∥ | 2 (1, 4) | 2 (0, 3) | .13¶ |
| Modified ODI | 38.8 ± 20 | 33.2 ± 17 | .19# |
| UCLA activity scale∥ | 4 (3, 7) | 5 (4, 7) | .33¶ |
| Roland-Morris questionnaire | 10.1 ± 7 | 11.7 ± 6 | .28 |
| Modified HHS | 63.9 ± 18 | 73.1 ± 22 | .17 |
Abbreviations: ER, external rotation; HHS, Harris Hip Score; IR, internal rotation; NPRS, numeric pain rating scale; ODI, Oswestry Disability Index; ROM, range of motion; UCLA, University of California at Los Angeles.
Values are mean ± SD unless otherwise indicated.
Compared to the sex-specific asymptomatic mean.
Compares groups by unpaired t test unless otherwise indicated.
Data missing for 3 patients; n = 81 reduced, n = 17 normal.
Values are median (interquartile range [25th, 75th percentile]).
Compares patients with reduced versus normal ROM by Wilcoxon test.
Minimal detectable difference was determined.
Minimal clinically important difference was found.
n = 76 reduced, n = 25 normal.
n = 23 reduced, n = 78 normal.
In TABLE 6, pain, function, and activity scores are compared between patients with LBP and at least 1 positive provocative hip test and patients without a positive provocative hip test. All 3 pain ratings reached a statistically significant difference. The difference in “worst pain” scores also exceeded the minimal detectable difference (greater than 1.5),34 but not the minimal clinically important difference (2.5 or greater),34 for the NPRS. The RMQ and mHHS scores both were significantly worse in patients with at least 1 positive provocative hip test (P<.05). The RMQ score difference value reached a minimal clinically important difference (3.5 points or greater).42 There was no statistically significant difference in the mODI between patients with and without provocative hip tests.
TABLE 6.
Association Between a Positive Provocative Hip Physical Examination Finding (for Either Side: Hip Impingement, FABER, Log Roll) and Baseline Clinical Outcomes (n = 101)*
| Provocative Hip Finding | |||
|---|---|---|---|
| Variable | Negative (n = 21) | Positive (n = 80) | P Value† |
| Average numeric pain rating‡ | 4 (2, 5) | 5 (4, 7) | .02§ |
| Worst numeric pain rating‡ | 7 (7, 9) | 9 (7, 10) | .055§∥ |
| Least numeric pain rating‡ | 1 (0, 2) | 2 (1, 4) | .005§ |
| Modified ODI | 30.1 ± 13 | 35.7 ± 19 | .21∥ |
| UCLA activity scale‡ | 6 (4, 7) | 5 (4, 7) | .14§ |
| Roland-Morris questionnaire | 8.5 ± 5 | 12.1 ± 6 | .02¶ |
| Modified HHS | 89.7 ± 9 | 65.8 ± 21 | .005 |
Abbreviations: FABER, flexion, abduction, external rotation; HHS, Harris Hip Score; ODI, Oswestry Disability Index; UCLA, University of California at Los Angeles.
Values are mean ± SD unless otherwise indicated.
Compares patients with a negative versus positive provocative hip examination by unpaired t test unless otherwise indicated.
Values are median (interquartile range [25th, 75th percentile]).
Compares groups by Wilcoxon test.
Minimal detectable difference was determined.
Minimal clinically important difference was found.
DISCUSSION
The current study is the first to report (1) patient characteristics, pain, and function scores described via validated hip and spine outcome tools; and (2) history and physical examination findings for both the lumbar spine and hip in consecutive patients presenting for evaluation and treatment with a common chief complaint of LBP. In this cohort of 101 consecutive patients who presented for evaluation and treatment of LBP with and without lower extremity pain, passive hip flexion and hip IR were reduced as compared to asymptomatic adults 50 years of age and younger.43 Further, 80% of the cohort had at least 1 positive provocative hip test that produced pain in the groin, lateral hip, or buttocks. Patients reported pain with pivoting (72%) and crossing the legs (48%), both daily activities suggestive of a hip disorder.27,35 Collectively, our findings suggest that there is a hip-spine connection in a number of patients seeking care for LBP. Because the etiologies for LBP are not well understood, assessing the patient history and hip physical examination findings may provide information as to whether a hip disorder may be a contributing factor to the complaint of LBP.
Our findings are consistent with the first description of the hip-spine syndrome by Offierski and MacNab.41 The hip disorder contributing to pain could include a structural change in the hip (OA, labral pathology, or hip deformity) or altered pain processing with hip movements.
Recognizing that movement of the hip can provoke LBP also is important, as this may be a secondary adaptive change to an initial spine, pelvic girdle, or hip disorder that, if left unrecognized or untreated, may result in continued LBP. Further, primary aberrant patterns of movement in the spine, pelvic girdle, or hip can be the primary source of pain. Distinguishing adaptive changes in one region that are related to movement or structural changes in another can be impossible from the clinical standpoint, especially when symptoms are chronic. Regardless, recognition that movement of the hip can provoke LBP is an important concept to assess and be recognized by health care providers. Improved recognition will promote more specifically directed treatment.
Our findings are similar to other reports of an association between reduced hip IR and LBP.1,9,11,14,38,53,54 Though the exact mechanisms for the association between hip IR and LBP remain under investigation, a hip with reduced IR due to a bony structural abnormality may alter forces across the lumbar spine. The alteration in force may manifest as pain over time. The current data also suggest that not only is there an association of reduced hip IR and flexion in people presenting with LBP, but also that these patients reported greater pain and reduced function of the hip and spine as compared to patients with LBP and no hip ROM restrictions.
The current data suggest that positive provocative hip tests are not uncommon in people with LBP. In the current study, 79% of patients with LBP had at least 1 provocative hip test. Further, patients with a provocative hip test reported greater pain and reduced hip and spine function as compared to patients with LBP and no positive provocative hip tests. Collectively, the current data suggest that assessment of the hip is important in evaluating patients presenting with LBP. A positive hip examination finding can provide information as to what diagnostic tests may need to be completed, as well as the need for treatment of the hip in addition to the lumbopelvic spine. For example, Van Dillen and colleagues58 and Hoffman et al24 found that restricting lumbopelvic movement during hip movement tests results in an immediate improvement in LBP symptoms. The concept of treating regions outside the lumbar spine to further improve LBP needs further investigation.
The current study has limitations. Because this study included only 101 consecutive patients presenting for evaluation of LBP to a single physician, the results may not be generalizable to the entire population of people with LBP. In addition, the median length of time of LBP reported by patients would classify their LBP as chronic. Therefore, although the sample included patients with a pain duration of less than 3 months, the findings of the current study cannot be directly applied to patients with acute pain. Though some statistical differences were found with regard to hip ROM and pain and function, the differences in degrees of motion were small, and clinical relevance related to a specific measured ROM cannot be determined with these data. However, reduced hip flexion and IR were associated with greater pain and reduced function. This is consistent with previously published works specifically assessing hip ROM in people with LBP.3,10,22,23,25,26,29,47,48,51,52,54,56,57,59
Biopsychosocial issues are associated with LBP. Another limitation of this study is that the study focused on the patient characteristics and physical examination findings, and did not include assessment of biopsychosocial factors that are also known to coexist in people with LBP. Finally, a large number of statistical tests were performed. As the number of tests increase, the likelihood increases that any one of these tests is significant by chance alone (ie, type I error). Adjusting P values for multiple comparisons would decrease this likelihood at the expense of an increased chance of type II error (ie, failing to identify a relationship that exists). We have not adjusted P values for multiple comparisons due to the exploratory nature of the study (ie, hypothesis generating rather than hypothesis confirming), and encourage readers to draw inferences based on the combined weight of evidence across variables rather than on any single result.
CONCLUSION
Physical examination findings in the hip, including reduced passive hip ROM and positive provocative hip tests, are not uncommon in patients presenting with LBP, with or without lower extremity pain. Patients with reduced hip ROM in different planes of motion and positive provocative hip tests reported worse LBP and worse hip and spine function at presentation compared to patients with LBP and no physical examination findings in the hip. Physical examination findings in the hip of people who present for evaluation of LBP are more common than previously reported. The unrecognized contribution of the hip to symptoms of a patient with LBP is a lost opportunity to provide intervention for factors that may be contributing to the symptoms. Care should be taken to examine the hip in patients presenting with LBP in order to improve the understanding of mechanisms for the development and persistence of LBP that, in turn, will drive treatment recommendations.
KEY POINTS.
FINDINGS:
Patients presenting for evaluation and treatment of LBP may have physical examination findings consistent with both lumbar spine and hip disorders. Patients with LBP who were found to have reduced hip flexion and IR were also noted to have reduced hip- and spine-related function compared to people with LBP without reduced hip ROM. One third of patients with LBP were found to have 2 positive provocative hip tests. A positive provocative hip test was associated with greater intensity of pain and reduced spine- and hip-related function as compared to patients with LBP and negative provocative hip tests.
IMPLICATIONS:
The movement of the hip and pain related to a hip disorder may impact LBP or coexist in people with LBP.
CAUTION:
On average, patients in this study had chronic LBP, and all were examined by a single physician. As a result, the findings are not generalizable to the entire population of patients with LBP.
Acknowledgments
This study was approved by the Washington University in St Louis Human Research Protection Office. Support for this project was provided by the Foundation for Physical Medicine and Rehabilitation through its Scott F. Nadler PASSOR Musculoskeletal Research Grant. Research reported in this publication was also supported by Washington University Institute of Clinical and Translational Sciences grant UL1TR000448, from the National Center for Advancing Translational Sciences of the National Institutes of Health. This research was also supported by National Heart, Lung, and Blood Institute training grant 2T35HL007815 and the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
REFERENCES
- 1.Almeida GP, de Souza VL, Sano SS, Saccol MF, Cohen M. Comparison of hip rotation range of motion in judo athletes with and without history of low back pain. Man Ther. 2012;17:231–235. 10.1016/j.math.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 3.Ben-Galim P, Ben-Galim T, Rand N, et al. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976). 2007;32:2099–2102. 10.1097/BRS.0b013e318145a3c5 [DOI] [PubMed] [Google Scholar]
- 4.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403–408. [PubMed] [Google Scholar]
- 5.Bohl WR, Steffee AD. Lumbar spinal stenosis: a cause of continued pain and disability in patients after total hip arthroplasty. Spine (Phila Pa 1976). 1979;4:168–173. [PubMed] [Google Scholar]
- 6.Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457. 10.2106/JBJS.D.02806 [DOI] [PubMed] [Google Scholar]
- 7.Butler DS. Tension testing: the lower limbs and trunk. In: Butler DS, Jones MA, eds. Mobilisation of the Nervous System. London, UK: Churchill Livingstone; 1991:139–146. [Google Scholar]
- 8.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. 10.1053/jars.2000.7683 [DOI] [PubMed] [Google Scholar]
- 9.Chesworth BM, Padfield BJ, Helewa A, Stitt L. A comparison of hip mobility in patients with low pack pain and matched healthy subjects. Physiother Can. 1994;46:267–274. [Google Scholar]
- 10.Chimenti PC, Drinkwater CJ, Li W, Lemay CA, Franklin PD, O’Keefe RJ. Factors associated with early improvement in low back pain after total hip arthroplasty: a multi-center prospective cohort analyses [sic]. J Arthroplasty. 2016;31:176–179. 10.1016/j.arth.2015.07.028 [DOI] [PubMed] [Google Scholar]
- 11.Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila Pa 1976). 1998;23:1009–1015. [DOI] [PubMed] [Google Scholar]
- 12.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. 10.1007/s11999-008-0680-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donelson R, Grant W, Kamps C, Medcalf R. Pain response to sagittal end-range spinal motion. A prospective, randomized, multicentered trial. Spine (Phila Pa 1976). 1991;16:S206–S212. [DOI] [PubMed] [Google Scholar]
- 14.Ellison JB, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther. 1990;70:537–541. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–2952; discussion 2952. [DOI] [PubMed] [Google Scholar]
- 16.Fogel GR, Esses SI. Hip spine syndrome: management of coexisting radiculopathy and arthritis of the lower extremity. Spine J. 2003;3:238–241. 10.1016/S1529-9430(02)00453-9 [DOI] [PubMed] [Google Scholar]
- 17.Fortin JD, Kissling RO, O’Connor BL, Vilensky JA. Sacroiliac joint innervation and pain. Am J Orthop (Belle Mead NJ). 1999;28:687–690. [PubMed] [Google Scholar]
- 18.Fritz JM, George S. The use of a classification approach to identify subgroups of patients with acute low back pain. Interrater reliability and short-term treatment outcomes. Spine (Phila Pa 1976). 2000;25:106–114. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. [DOI] [PubMed] [Google Scholar]
- 20.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67:1867–1872. [DOI] [PubMed] [Google Scholar]
- 21.Harris-Hayes M, Royer NK. Relationship of acetabular dysplasia and femoroacetabular impingement to hip osteoarthritis: a focused review. PM R. 2011;3:1055–1067.e1. 10.1016/j.pmrj.2011.08.533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil. 2009;18:60–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman SL, Johnson MB, Zou D, Harris-Hayes M, Van Dillen LR. Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Man Ther. 2011;16:344–350. 10.1016/j.math.2010.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffman SL, Johnson MB, Zou D, Van Dillen LR. Gender differences in modifying lumbopelvic motion during hip medial rotation in people with low back pain. Rehabil Res Pract. 2012;2012:635312. 10.1155/2012/635312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffman SL, Johnson MB, Zou D, Van Dillen LR. Sex differences in lumbopelvic movement patterns during hip medial rotation in people with chronic low back pain. Arch Phys Med Rehabil. 2011;92:1053–1059. 10.1016/j.apmr.2011.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsieh PH, Chang Y, Chen DW, Lee MS, Shih HN, Ueng SW. Pain distribution and response to total hip arthroplasty: a prospective observational study in 113 patients with end-stage hip disease. J Orthop Sci. 2012;17:213–218. 10.1007/s00776-012-0204-1 [DOI] [PubMed] [Google Scholar]
- 27.Jones S Evaluation of the hip. In: Fagerson TL, ed. The Hip Handbook. Boston, MA: Butterworth-Heinemann; 1998:ch 3. [Google Scholar]
- 28.Khan AM, McLoughlin E, Giannakas K, Hutchinson C, Andrew JG. Hip osteoarthritis: where is the pain? Ann R Coll Surg Engl. 2004;86:119–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee SW, Kim SY. Comparison of chronic low-back pain patients hip range of motion with lumbar instability. J Phys Ther Sci. 2015;27:349–351. 10.1589/jpts.27.349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lesher JM, Dreyfuss P, Hager N, Kaplan M, Furman M. Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9:22–25. 10.1111/j.1526-4637.2006.00153.x [DOI] [PubMed] [Google Scholar]
- 31.Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine (Phila Pa 1976). 2004;29:2593–2602. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald SJ, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9. [Google Scholar]
- 33.Magee DJ. Lumbar spine. In: Orthopedic Physical Assessment. 2nd ed. Philadelphia, PA: W.B. Saunders; 1992:247–281. [Google Scholar]
- 34.Mannion AF, Balagué F, Pellisé F, Cedraschi C. Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol. 2007;3:610–618. 10.1038/ncprheum0646 [DOI] [PubMed] [Google Scholar]
- 35.Martin HD, Kelly BT, Leunig M, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26:161–172. 10.1016/j.arthro.2009.07.015 [DOI] [PubMed] [Google Scholar]
- 36.McNamara MJ, Barrett KG, Christie MJ, Spengler DM. Lumbar spinal stenosis and lower extremity arthroplasty. J Arthroplasty. 1993;8:273–277. 10.1016/S0883-5403(06)80089-6 [DOI] [PubMed] [Google Scholar]
- 37.Moore ML. The measurement of joint motion; the technic of goniometry. Phys Ther Rev. 1949;29:256–264. [PubMed] [Google Scholar]
- 38.Murray E, Birley E, Twycross-Lewis R, Morrissey D. The relationship between hip rotation range of movement and low back pain prevalence in amateur golfers: an observational study. Phys Ther Sport. 2009;10:131–135. 10.1016/j.ptsp.2009.08.002 [DOI] [PubMed] [Google Scholar]
- 39.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA: F.A. Davis; 2003. [Google Scholar]
- 40.Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011;93 suppl 2:17–21. 10.2106/JBJS.J.01735 [DOI] [PubMed] [Google Scholar]
- 41.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976). 1983;8:316–321. [DOI] [PubMed] [Google Scholar]
- 42.Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607. 10.1016/j.berh.2005.03.003 [DOI] [PubMed] [Google Scholar]
- 43.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010;2:888–895. 10.1016/j.pmrj.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Prather H, Hunt D, Fournie A, Clohisy JC. Early intra-articular hip disease presenting with posterior pelvic and groin pain. PM R. 2009;1:809–815. 10.1016/j.pmrj.2009.07.013 [DOI] [PubMed] [Google Scholar]
- 45.Prather H, Van Dillen LR, Kymes SM, Armbrecht MA, Stwalley D, Clohisy JC. Impact of coexistent lumbar spine disorders on clinical outcomes and physician charges associated with total hip arthroplasty. Spine J. 2012;12:363–369. 10.1016/j.spinee.2011.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983;8:141–144. [DOI] [PubMed] [Google Scholar]
- 47.Sadeghisani M, Manshadi FD, Kalantari KK, et al. Correlation between hip rotation range-of-motion impairment and low back pain. A literature review. Ortop Traumatol Rehabil. 2015;17:455–462. 10.5604/15093492.1186813 [DOI] [PubMed] [Google Scholar]
- 48.Sánchez-Zuriaga D, López-Pascual J, Garrido-Jaén D, García-Mas MA. A comparison of lumbopelvic motion patterns and erector spinae behavior between asymptomatic subjects and patients with recurrent low back pain during pain-free periods. J Manipulative Physiol Ther. 2015;38:130–137. 10.1016/j.jmpt.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 49.Saunders WA, Gleeson JA, Timlin DM, Preston TD, Brewerton DA. Degenerative joint disease in the hip and spine. Rheumatol Rehabil. 1979;18:137–141. [DOI] [PubMed] [Google Scholar]
- 50.Sembrano JN, Polly DW Jr., How often is low back pain not coming from the back? Spine (Phila Pa 1976). 2009;34:E27–E32. 10.1097/BRS.0b013e31818b8882 [DOI] [PubMed] [Google Scholar]
- 51.Staibano P, Winemaker M, Petruccelli D, de Beer J. Total joint arthroplasty and preoperative low back pain. J Arthroplasty. 2014;29:867–871. 10.1016/j.arth.2013.10.001 [DOI] [PubMed] [Google Scholar]
- 52.Tanaka S, Matsumoto S, Fujii K, Tamari K, Mitani S, Tsubahara A. Factors related to low back pain in patients with hip osteoarthritis. J Back Musculoskelet Rehabil. 2015;28:409–414. 10.3233/BMR-140535 [DOI] [PubMed] [Google Scholar]
- 53.Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32:494–497. [DOI] [PubMed] [Google Scholar]
- 54.Vad VB, Gebeh A, Dines D, Altchek D, Norris B. Hip and shoulder internal rotation range of motion deficits in professional tennis players. J Sci Med Sport. 2003;6:71–75. [DOI] [PubMed] [Google Scholar]
- 55.van Dijk GM, Veenhof C, Spreeuwenberg P, et al. Prognosis of limitations in activities in osteoarthritis of the hip or knee: a 3-year cohort study. Arch Phys Med Rehabil. 2010;91:58–66. 10.1016/j.apmr.2009.08.147 [DOI] [PubMed] [Google Scholar]
- 56.Van Dillen LR, Bloom NJ, Gombatto SP, Susco TM. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9:72–81. 10.1016/j.ptsp.2008.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van Dillen LR, Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Phys Med Rehabil. 2007;88:351–360. 10.1016/j.apmr.2006.12.021 [DOI] [PubMed] [Google Scholar]
- 58.Van Dillen LR, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Man Ther. 2009;14:52–60. 10.1016/j.math.2007.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Dillen LR, McDonnell MK, Fleming DA, Sahrmann SA. Effect of knee and hip position on hip extension range of motion in individuals with and without low back pain. J Orthop Sports Phys Ther. 2000;30:307–316. 10.2519/jospt.2000.30.6.307 [DOI] [PubMed] [Google Scholar]
- 60.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78:979–988. [DOI] [PubMed] [Google Scholar]


