Abstract
Objective
People with pulmonary hypertension (PH) are at an increased risk of experiencing anxiety disorders. This study developed and tested the acceptability, feasibility and preliminary effectiveness of a cognitive behavioural self-help intervention for anxiety in adults with PH using a pilot randomised control trial design.
Methods
Individuals with PH recruited from pulmonary hypertension associations were randomised to either receive a newly developed self-help intervention (n=37) or a wait-list condition (n=40). Acceptability was explored using mixed-methods questionnaires. A 2×3 repeated-measures analysis of variance was used to explore anxiety (GAD-7), depression (PHQ-9), health-related quality of life (emPHAsis-10), dyspnoea (D-12), self-mastery (Self-Mastery Scale) and mood-related cognitions and behaviours (CBP-Q) at baseline, post-intervention and 1-month follow up. A mediation analysis was performed to examine potential mechanisms of change.
Results
Dropout was low at 15.6%. All participants would recommend the intervention to another person with PH and felt it had helped with their anxiety. Participants in the intervention group reported a reduction in anxiety, depression and cognitive and behavioural processes linked with mood disorders, compared to the control group. Change in unhelpful cognitions and behaviours mediated the relationship between intervention condition and change in anxiety and depression.
Discussion
The intervention was found to be acceptable, feasible and safe. Anxiety at baseline was higher than previously observed, which could be associated with the additional burden caused by COVID-19 as the intervention was trialled during the pandemic. Findings add to the growing evidence supporting the use of psychological therapies, including cognitive behavioural therapy, in this clinical group.
Short abstract
Mood disorders are highly prevalent in people with pulmonary hypertension (PH), although there is limited research examining effective treatments. This study developed and piloted a self-help intervention targeting anxiety specifically in PH. https://bit.ly/30MUrOB
Introduction
Anxiety and depression disorders are highly prevalent in people with pulmonary hypertension (PH) with rates of up to 50% [1, 2]. Such figures may also be underestimated as mental health conditions maybe under recognised in this group [2–4], and a recent UK survey found 85% of people with PH (n=824) reported greater symptoms of anxiety associated with the current COVID-19 pandemic [5]. Indeed, anxiety is a pertinent issue in PH due to its prevalence, the physiological effects on cardiovascular functioning which could exacerbate difficulties [6] and overlapping symptoms. Anxiety in PH is also associated with reduced health-related quality of life (HRQoL) and depression [7, 8].
There is limited research examining treatments for anxiety in PH. In terms of psychological interventions, a systematic review found only three trials, all of which used cognitive behavioural therapy (CBT) or strategies commonly associated with CBT, such as psychoeducation and relaxation techniques [1]. CBT informed interventions were found to be associated with significant improvements in anxiety, depression and HRQoL in PH [1]. In the UK, treatment guidelines recommend the use of CBT for anxiety and panic disorder in the general population, delivered within a stepped care model – first providing CBT self-management interventions [9]. There is growing evidence suggesting self-help interventions offer an accessible and effective form of treatment, including condition-specific interventions, which have the benefit of addressing specific challenges within clinical groups [10].
In collaboration with Pulmonary Hypertension Association UK, we developed a CBT informed self-help intervention for anxiety in adults with PH. In the current study, we conducted a pilot randomised controlled trial investigating the intervention against a wait-list control condition. The aim was the explore the feasibility and acceptability of the intervention, and preliminary effectiveness to help inform a sample size calculation for a definitive trial. Furthermore, potential active mechanisms of change associated with the trial were explored using a mediation analysis.
Methods
Design
Participants were block randomised 1:1 to the two groups using an online randomiser (available at: https://www.random.org). Participants were asked to complete a series of measures at baseline, post-intervention and one-month post-intervention. Ethical approval was obtained from the Department of Psychology Ethics Committee at the University of Sheffield (034442). The study was registered at clinicaltrials.gov: NCT04450862. CONSORT guidelines were used.
Eligibility criteria
Participants were required to be aged 18 years or over; have a diagnosis of PH; provide informed consent; complete a series of self-report questionnaires independently in English; and self-report difficulties with anxiety. Participants could be living in the UK or outside of the UK (see results for the list of countries where participants were living). Individuals were not eligible if they experienced thoughts of self-harm or suicide.
Procedure
A convenience sampling method was used; participants were recruited via advertisements from pulmonary hypertension associations. Participants were recruited between August and April 2021 Before being randomised, participants were first asked to complete a consent form, demographic and health-related questionnaires.
Our goal was to eventually make the intervention available to all members of PHA UK. Although this is a UK based charity, they are contacted by people outside of the UK with whom it is more practical to correspond electronically. Therefore, in accordance with how the intervention may be used in practice, participants in the UK were sent a paper version of the intervention, while non-UK participants received an electronic version.
Two weeks after, participants were contacted by telephone (UK participants) or email (non-UK participants), to assess adherence and acceptability, using a semi-structured questionnaire. Phone calls lasted on average 12.36 min (sd 12.25 min).
Participants randomised to the wait-list condition were informed that they would be contacted again in 4 weeks.
After 4 weeks, participants were asked to complete the health-related questionnaires, which were repeated 1 month later. Participants in the intervention group were then asked to complete a semi-structured acceptability questionnaire. Participants in the control group were informed if the intervention was acceptable, they would receive a copy in the future. Questionnaires were hosted by Qualtrics (https://www.qualtrics.com).
Intervention
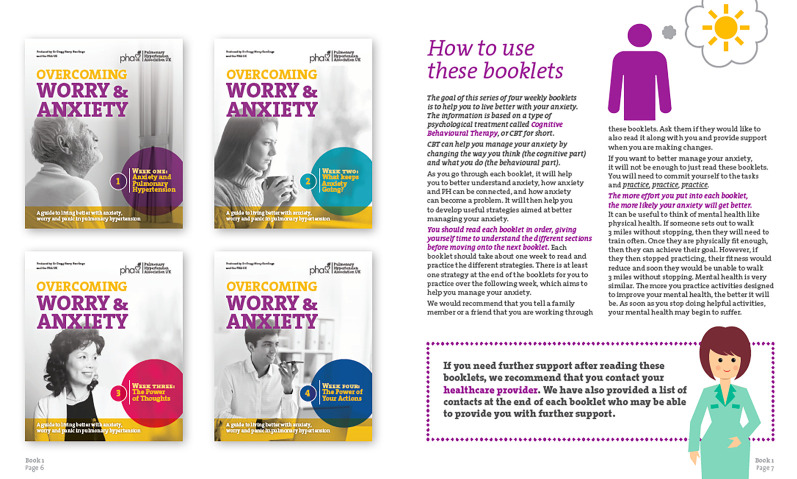
The intervention consisted of a four-week programme corresponding to four individual booklets (figure 1 and table 1). A multi-disciplinary stakeholders’ group was established comprising of adults living with PH and caregivers (n=4), clinical psychologists (n=2), PH nurse specialists (n=2), professionals from PHA UK (n=3), a cognitive behavioural therapist and graphic designer. The lead researcher developed the intervention guided by clinical experience and the evidence-base. For example, the intervention was guided by CBT-related theories on generalised anxiety disorder (GAD) [11], panic disorder [12] and health anxiety [13], which have all previously been documented as prevalent in this group [1, 14]. The lead researcher kept in regular contact with members of the stakeholders’ group through a series of meetings acting on suggestions until the intervention was finalised.
FIGURE 1.
Extract from booklet one showing the four booklets and providing participants with instructions.
TABLE 1.
Outline of the intervention (also see Supplement 1)
| Booklet | Contents | Exercises |
| 1 | Psychoeducation on CBT, anxiety and anxiety in PH | Develop a mini-CBT formulation and practice slow breathing exercises |
| 2 | Psychoeducation on maintenance factors for anxiety relevant to PH | Develop a broader CBT formulation focusing on short and long-term difficulties, and practice mindfulness exercises |
| 3 | Psychoeducation on cognitive biases and normalisation of difficulties though case vignettes | Practice thought monitoring and thought challenging exercises |
| 4 | Psychoeducation on graded exposure taking into consideration impact of fatigue. Information on other factors affecting anxiety and relapse prevention | Develop a anxiety hierarchy, create a plan to manage setbacks and progressive muscle relaxation exercise |
CBT: cognitive behavioural therapy; PH: pulmonary hypertension.
Measures
Participants provided demographics and information concerning their diagnosis of PH, PH functional class, duration of PH and whether they had received treatment for anxiety in the last twelve-months.
Anxiety, as the primary outcome measure, was measured using the GAD-7 questionnaire [15]. A score of 0–4 indicates “minimal difficulties”, 5–9 “mild”, 10–14 “moderate” and 15–21 “severe” anxiety. The clinical cut-off score is ≥8 with a reliable change of ≥4 [16]. Depression was measured using the PHQ-9 [17]. A score of 0–4 indicates “minimal difficulties”, 5–9 “mild”, 10–14 “moderate”, 15–19 “moderately severe” and ≥20 “severe” depression. The clinical cut-off score is ≥10, with a reliable change of ≥6 [16]. HRQoL was examined using the emPHAsis-10 [18]. Scores range from 0–50, with a higher score indicative of lower HRQoL. Breathing difficulties were explored using the Dyspnoea 12 (D12) [19]. Total scores range from 0–36 with a higher score indicating greater difficulty. Given the relationship between coping and anxiety in PH [8], coping was measured using the Self-Mastery Scale [20]. Total scores range from 7–49 with a higher score suggesting a greater perceived capacity to cope. To measure unhelpful cognitions and behaviours that may underlie anxiety, the Cognitive and Behavioural Processes Questionnaire (CBP-Q) was used. Total scores range from 0–120. Higher scores are associated with more unhelpful responses, which have been found to positively relate to anxiety and depression [21].
Two mixed-methods questionnaires were developed to assess adherence and acceptability part-way through and at the end of the study. Participants were asked about their experiences of anxiety in PH, the different aspects of the intervention and their engagement in the research trial.
Sample size
In accordance with sample size guidelines for a pilot trial [22], a sample size of 36 in each arm was required using 90% power and 5% significance level. This was based a standardised effect size of 0.53 (Hedges’ g), and average dropout rate of 16.5% reported in a meta-analysis of 54 self-help interventions for anxiety [23].
Data analysis
A series of independent samples t-tests and Pearson's chi-square tests were performed to investigate group differences between CBT versus control; UK versus non-UK participants, and completers versus non-completers.
A series of two-way mixed analysis of variance (ANOVA) were run for each health-related measure examining the interaction, with condition representing the between subjects factor and time the within subjects factor. Where the interaction was significant, a series of independent samples t-tests were performed to compare differences at each time point between the two groups. A series of repeated measures ANOVAs were then used to investigate effects of time for each condition for all outcome measures corrected using Bonferroni. The alpha level (0.05) was accepted for all other tests. G*Power-3 was used to perform a post hoc sample size calculation. Partial η2 was converted to Cohen's f (f=0.1 small, 0.25 medium and 0.4 large) [24].
A series of mediated regression analyses were performed to investigate whether the effects of condition on significant changes in health-outcomes were mediated by change in CBP-Q scores. Change in scores was calculated by subtracting scores at baseline from one-month follow-up. A Sobel test was performed and Cohen's benchmarks were used to interpret effect sizes (r2=0.02 small, 0.15 medium and 0.35 large) [24].
SPSS25 was used for all statistical analysis with Hayes’ process macro extension for the mediation analyses [25].
Qualitative data collected from the adherence and acceptability questionnaires were analysed using quantitative content analysis [26]. A coding scheme was developed by the authors corresponding to the questions asked, which was used to code the qualitative data before quantifying participants’ responses.
Results
Recruitment
Overall, n=138 individuals accessed the link to read the participant information sheet, of whom n=77 (55.8%) completed the baseline measures (figure 2).
FIGURE 2.
CONSORT flow diagram.
Randomisation
No significant differences in demographic or health-related outcomes were observed between participants in the self-help or control group (table 2).
TABLE 2.
Baseline data for participants randomised to the cognitive behavioural therapy (CBT) self-help or control group
| Characteristics | CBT self-help | Control | p-value |
| Number of participants | 37 | 40 | 0.73 |
| Demographics | |||
| Age (years) | 48.2±14.03 | 47.5±13.1 | 0.83 |
| Gender | 0.4 | ||
| Male | 1 | 3 | |
| Female | 35 | 37 | |
| Other | 1 | 0 | |
| Ethnicity | 0.57 | ||
| White | 25 | 10 | |
| Not reported or not clear | 12 | 12 | |
| Asian | 4 | 5 | |
| Hispanic | 0 | 1 | |
| Black | 0 | 1 | |
| Latina | 1 | 1 | |
| Education (years) | 15.3±4.7 | 15.6±3.8 | 0.77 |
| Employment | 0.73 | ||
| Employed | 14 | 13 | |
| Not employed | 8 | 14 | |
| Retired | 9 | 9 | |
| Student | 2 | 1 | |
| Other | 4 | 3 | |
| PH factors | |||
| PH type | 0.83 | ||
| Idiopathic PH | 19 | 16 | |
| Chronic thromboembolic PH | 7 | 7 | |
| Connective tissue disease | 2 | 4 | |
| Congenital PH | 2 | 2 | |
| Familial PH | 0 | 1 | |
| Other | 3 | 6 | |
| Not sure | 4 | 4 | |
| PH class | 0.27 | ||
| I | 6 | 2 | |
| II | 7 | 10 | |
| III | 12 | 12 | |
| IV | 2 | 0 | |
| Not sure | 10 | 13 | |
| Years since diagnosis | 9.48±10.02 | 7.84±7.6 | 0.42 |
| Psychological factors | |||
| Prescribed medication for anxiety | 9±24.3% | 13±32.5% | 0.43 |
| Received therapy for anxiety | 7±18.9% | 9±22.5% | 0.7 |
| Anxiety | 10.43±5.11 | 11.75±5.78 | 0.29 |
| Depression | 12.38±5.12 | 12.7±6 | 0.8 |
| HRQoL | 38.49±10.57 | 41.28±11.39 | 0.27 |
| Dyspnoea | 14.38±9.91 | 16.55±8.96 | 0.32 |
| Self-mastery | 25.95±7.08 | 24.33±7.75 | 0.34 |
| CBP-Q | 69.59±13.43 | 68.55±19.67 | 0.79 |
Data are presented as mean±sd unless otherwise stated. Results are from independent samples t-tests and Pearson's chi-square tests. PH: pulmonary hypertension; HRQoL: health-related quality of life; CBP-Q: cognitive and behavioural processes questionnaire.
UK versus non-UK participants
Non-UK participants lived in Canada (n=17), India (n=7), USA (n=5), the Netherlands (n=1) and Australia (n=1). No significant differences were observed between the two groups with the exception of ethnicity, as a greater number of UK participants self-identified as white. Given the ethnic composition of countries from where individuals were recruited (e.g. UK versus India), this may be expected (Supplement 2).
Completers versus non-completers
A dropout rate of 15.6% was observed (self-help=18.9%, control=12.5%). Non-completers were significantly younger, reported lower levels of anxiety and scored higher on self-mastery (p<0.05). There was a greater ratio of males who completed the study; however, males overall were greatly underrepresented accounting for 5% of the sample (Supplement 3).
Acceptability
Overall, 32/37 (86.5%) of participants in the intervention condition completed the Check-in Questionnaire at two-weeks. The majority of participants were working on booklet one (n=7) or two (n=17). The majority (>70%, 23 out of 32) understood most of the content, felt it could help and did not find the intervention difficult or distressing (Supplement 4).
In total, 25 out of 32 (78.1%) of participants completed the Final Acceptability Questionnaire. 10 participants rated the intervention as “Excellent”, 14 “Good” and one “Fair”. Nearly half reported the intervention as “Moderately” helpful. All participants would recommend the intervention to another person with PH. Most (>68%, 17 out of 25) found the different booklets “Extremely” or “Very Helpful”. At the end of the study, >80% (20 out of 25) felt more in control of their anxiety, supported during the intervention, valued that it was specific to PH and felt others would benefit from the resource (supplement 4).
Analysis of qualitative feedback revealed participants wanted to take part due to difficulties with their anxiety, which for some was linked to COVID-19 (n=10). The majority reported the benefits of learning more about their anxiety (n=17) and developing strategies to manage (n=22). Participants recognised the importance of continuing to practice the strategies and valued the ability to refer back to the booklets at a later date. The largest group (n=9) felt there was “nothing” they did not like about the intervention. For others, it seemed external sources of motivation could have helped them to engage better (supplement 5).
Effectiveness
Reliable change
Both groups scored above the clinical cut-off on the GAD-7 and PHQ-9 measures at baseline, scoring within the “moderate” range. While anxiety and depression symptomatology reduced below the clinical level and to the “mild” range following the self-help intervention and remained at this level at follow-up, those in the control group continued to report “moderate” and clinical levels throughout.
In the self-help group, 64.9% and 67.6% of participants scored above the clinical level on anxiety and depression, respectively, which by the end of treatment, reduced to 25% and 32.1%. Overall, 71.4% and 39.3% of participants reported a reliable change in anxiety and depression, respectively, at the end of the study, compared to baseline or post-intervention scores. In the control group, 44.1% of individuals reported a reliable change in anxiety at one-month follow up, although nearly two-thirds remained above the clinical cut-off. Similarly, over half of the participants in the control group experienced clinical levels of depression at the end of the study (supplement 6).
Statistical change
A series of two-way mixed ANOVAs revealed statistically significant interactions between group and time for anxiety, depression and CBP-Q (table 3).
TABLE 3.
Health outcomes and results of 2×3 mixed ANOVAs, partial η2 and Cohen's f in the cognitive behavioural therapy (CBT) (n=27) and control (n=30) groups
| Measure | Group | Baseline | Post | 1 month | Two-way mixed ANOVA (group×time) | |||
| F | p-value | η2 | Cohen’s f | |||||
| Anxiety | CBT | 11±5.03 | 7.56±3.93# | 5.89±4.4 | F(2,110)=4.23 | 0.017 | 0.07 | 0.28 |
| Control | 11.9±5.29 | 11.03±5.78# | 10.23±5.62 | |||||
| Depression | CBT | 12.41±5.47 | 8.11±4.21 | 7.48±5.11# | F(1.76,97.71)=3.26 HF | 0.048 | 0.06 | 0.24 |
| Control | 13.5±5.4 | 11.3±5.47 | 11.7±7.1# | |||||
| HRQoL | CBT | 37.7±11.16 | 35.59±10.69 | 34.37±10.14 | F(2,110)=0.1 | 0.9 | 0.002 | 0.04 |
| Control | 42.07±11.27 | 41.67±11.06 | 39.5±11.81 | |||||
| Dyspnoea | CBT | 14.93±10.6 | 14.85±10.07 | 12.63±8.54 | F(1.85, 101.67)=0.77 HF | 0.46 | 0.01 | 0.12 |
| Control | 16.77±8.74 | 15.77±8.92 | 15.3±9.29 | |||||
| Self-Mastery | CBT | 25.22±6.7 | 26.41±5.66 | 27.63±4.79 | F(2,110)=0.24¶ | 0.79 | 0.004 | 0.06 |
| Control | 24.2±7.59 | 25.63±5.3 | 25.67±4.73 | |||||
| CBP-Q | CBT | 69.56±14.3 | 57.59±15.93 | 50.26±18.8 | F(1.67,91.74)=8.55 HF¶ | 0.001 | 0.13 | 0.39 |
| Control | 67.77±17.88 | 63.87±16.47 | 64.17±22.28 | |||||
Data are presented as mean±sd unless otherwise stated. HF: Huynh-Feldt; HRQoL: health-related quality of life; CBP-Q: cognitive behavioural processes questionnaire. #: Levene's Test of Equality not met (p>0.05) for mixed ANOVA; ¶: Test of Equality of Covariance significant; f: ANOVA effect size.
While no statistical difference in anxiety was observed at baseline between the two groups (t(55)=−0.66, p=0.51), there was a statistical difference at the post-intervention (t(51.31)=−2.68, p=0.01) and follow-up stage (t(55)=−3.33, p=0.002), with those in the CBT group reporting lower scores. Similarly, for depression, differences at baseline was non-significant (t(55)=−0.76, p=0.45), but was at post-intervention (t(55)=−2.45, p=0.018) and follow-up (t(52.56)=−2.55, p=0.01) in the same direction. Finally, for the CBP-Q, differences were non-significant at baseline (t(55)=0.41, p=0.68) and post-intervention (t(55)=−1.46, p=0.15), however, at the one one-month stage there was a significant difference (t(55)=−2.53, p=0.014), with the controls reporting a greater number of unhelpful thoughts and behaviours.
A series of repeated measures ANOVAs revealed a statistically significant effect of time on anxiety, depression and CBP-Q in the CBT group, indicating reductions across time. A significant effect was also observed for depression in the control group; however, post hoc tests revealed this reduction was only temporary as there was no significant difference between baseline and 1-month follow-up (table 4).
TABLE 4.
Mean differences in the cognitive behavioural therapy (CBT) (n=27) and control (n=30) group for health outcomes and results of repeated measures ANOVAs and pairwise comparisons corrected using Bonferroni
| Measure | Group | Repeated measures ANOVA | Pairwise comparison | |||||
| F | p-value | η2 | Cohen’s f | Baseline versus post | Baseline versus 1 month | Post versus 1 month | ||
| Anxiety | CBT | F(2,52) =18.54 | <0.001 | 0.42 | 0.84 | −3.44 (p=0.003) | −5.11 (p<0.001) | −1.67 (p=0.045) |
| Control | F(2,58)=1.84 | 0.17 | 0.06 | 0.25 | −0.87 (p=0.92) | −1.67 (p=0.29) | −0.8 (p=1) | |
| Depression | CBT | F(1.63,42.25) =13.02 HF | <0.001 | 0.33 | 0.71 | −4.3 (p=0.002) | −4.93 (p=0.002) | −0.63 (p=1) |
| Control | F(2,58)= 5.43 | 0.007 | 0.16 | 0.43 | −2.2 (p=0.004) | −1.8 (p=0.11) | 0.4 (p=1) | |
| HRQoL | CBT | F(2,52)=2.54 | 0.09 | 0.09 | 0.31 | −1.11 (p=1) | −3.33 (p=0.2) | −2.22 (p=0.34) |
| Control | F(2,58)=2.85 | 0.07 | 0.09 | 0.31 | −0.4 (p=1) | −2.57 (p=0.15) | −2.17 (p=0.16) | |
| Dyspnoea | CBT | F(2,52)=2.45 | 0.1 | 0.09 | 0.31 | −0.07 (p=1) | −2.3 (p=0.34) | −2.22 (p=0.13) |
| Control | F(2,58)=1.64 | 0.2 | 0.05 | 0.24 | −1 (p=0.67) | −1.47 (p=0.39) | −0.47 (p=1) | |
| Self-mastery | CBT | F(2,52)=1.25 | 0.3 | 0.05 | 0.22 | 1.19 (p=1) | 2.41 (p=0.54) | 1.22 (p=1) |
| Control | F(2,58)=0.3 | 0.29 | 0.04 | 0.21 | 1.43 (p=0.79) | 1.47 (p=0.38) | 0.03 (p=1) | |
| CBP-Q | CBT | F(1.63,42.3)=18.38 HF | <0.001 | 0.41 | 0.83 | −11.9 (p=0.001) | −19.3 (p<0.001) | −7.33 (p=0.03) |
| Control | F(2,58)=2.04 | 0.14 | 0.07 | 0.27 | −3.9 (p=0.15) | −3.6 (p=0.52) | 0.3 (p=1) | |
HF: Huynh-Feldt; HRQoL: health-related quality of life; CBP-Q: cognitive behavioural processes questionnaire.
Sample size analysis
A sample size analysis was calculated using an observed effect size of f=0.28 for the primary outcome measure. Accepting 0.05 as the alpha level, a level of statistical power of 80%, two groups (self-help and wait-list) and three measurements (baseline, post-intervention and one-month) and sphericity not violated, a final sample size of n=68 is required. Taking into consideration a dropout rate of 15.6%, 80 participants are required for a definitive trial.
Mechanisms of change
Intervention group was significantly related to change in anxiety scores (b=3.62 (se=1.35), t(59)=2.69, p=0.009) and change in CBP-Q at one-month (b=14.86 (se=4.4), t(59)=3.37, p=0.001). Change in CBP-Q scores significantly predicted change in anxiety (b=0.13 (se=0.04), t(58)=3.52, p<0.001). Controlling for change in CBP-Q as a mediator, condition was not a significant predictor of change in anxiety (b=1.72 (se=1.35), t(58)=1.27, p=0.21). Overall, change in CBP-Q was a significant mediator of change in anxiety (effect 1.91 (se=0.82), 95% CI 0.56–3.67), which was confirmed by a Sobel test (Z=2.34 (se=0.82), p=0.02).
For depression, intervention group significantly predicted change in depression scores (b=3.31 (se=1.38), t(59)=2.4, p=0.02) and change in CBP-Q (b=14.86 (se=4.4), t(59)=3.37, p=0.001). Change in CBP-Q was a significant predictor of change in depression (b=0.19 (se=0.03), t(58)=5.87, p<0.001). When change in CBP-Q was controlled, condition was not a significant predictor of change in depression (b=0.46 (se=1.2), t(58)=0.38,p=0.7). As in anxiety, change in CBP-Q was a significant mediator of change in depression (effect 2.84 (se=1.23), 95% CI 0.78–5.6), which was further assessed using a Sobel test (Z=2.98 (se=0.95), p=0.003).
Discussion
Findings suggest that the intervention was feasible, acceptable and safe, as no adverse events were reported. The majority of participants reported the intervention as “Excellent” or “Good” and would recommend it to someone with PH. An overall attrition rate of 15.6% was observed, which is comparable to rates reported by a meta-analysis of 54 self-help interventions for anxiety (16.5%) [23], as well as a meta-analysis of 45 studies investigating face-to-face psychological therapies for adults with GAD (16.99%) [27].
Participants who completed the study were significantly older, scored higher on self-mastery and reported greater anxiety. This finding is consistent with research suggesting younger adults are more likely to drop out of psychological therapies [28]. It is plausible that people who were less affected by anxiety had lower motivation to engage. However, findings suggest that the intervention was helpful in reducing symptoms of anxiety in those with mild to severe symptoms, and therefore supporting patients with all levels of anxiety to engage with psychological care may be beneficial. Similarly, while it has been suggested that anxiety is greater in those recently diagnosed with PH [1], as participants had been living with PH for an average of seven-nine years, interventions targeting anxiety may be helpful to people across the clinical group. However, our current ability to explore anxiety in people with PH is likely to be impaired by the lack of standardised screening assessments. Research investigating the suitability, reliability and adaptation of non-PH and generic health-related questionnaires in this population is needed.
At baseline, 70.1% (n=54 out of 77) and 64.9% (n=50 out of 77) of participants scored above the clinical level on anxiety and depression, respectively, which is greater than previous studies [1]. Given that participants here had to be experiencing difficulties with anxiety, it is reasonable to suggest that rates are higher compared to the wider PH population. Nevertheless, it could also reflect the impact of the COVID-19 pandemic [29], as highlighted by ten participants who discussed the pandemic as a reason for their participation. While participants found the intervention was helpful in managing their anxiety during the pandemic, it is not known whether this was translated to COVID-19-related anxieties. Further research is required examining the psychosocial effects of the pandemic in people with PH and how best to support this group.
Participants in the CBT group reported a significant reduction in anxiety, depression and unhelpful cognitions and behaviours over time, compared to participants in the control group. As such, the results further justify a large-scale and definitive randomized controlled trial of the current intervention. Within-group differences revealed a large and significant reduction in the CBT group in symptoms of anxiety and depression, with participants scoring below the clinical level at the post-intervention stage with gains maintained, and significantly improved upon for anxiety, at follow-up. Taken together, the findings support the evidence concerning the benefits of psychological therapy, specifically CBT, in this population. Participants in the control group also experienced an improvement in depression at the post-intervention stage. While it is not unusual for control participants to report therapeutic gains [30]; the majority of participants remained above the clinical level and gains were only temporary.
Results from the mediation analyses indicate that the intervention had an indirect effect on improvement in mood outcomes, through changing cognitions and behaviours. Further research is required to examine the relationship between the cognitive and behavioural strategies that individuals use to cope, and health-related outcomes in PH. Identifying factors associated with positive health outcomes can help to recognise important therapeutic targets, and guide the development of services [3, 8].
Due to the modest sample size, differences in outcomes between participants receiving paper versus electronic versions of the intervention were not examined. Therefore, it is not clear what impact (if any) this had on observed effect sizes, especially given the difference in effectiveness between the two approaches observed [23].
Notwithstanding the female preponderance reported in PH [31], male were considerably underrepresented in the current sample, which is consistent with previous evidence suggesting females with PH are more likely to take part in research [32]. Further investigation is required to explore such gender differences (including the likelihood of males with PH engaging with psychological therapies) and develop strategies to help overcome barriers for males.
Finally, it could be a limitation that a wait-list control group was used as this could have inflated study effects than if an active treatment was used. However, this approach was utilised as it reflects the current support typically available to patients as information on anxiety in PH is limited.
Conclusion
We developed a self-help intervention for anxiety in PH, which was found to be acceptable, feasible and safe. Attrition was comparable to other psychological therapies, including face-to-face treatments. While only preliminary, participants in the self-help condition reported a significant and reliable reduction in symptoms of anxiety and depression, which were fully mediated by a change in cognitions and behaviours related to the intervention. Results add to the growing evidence supporting psychological therapies in people with PH. Self-help intervention offer an effective and accessible form of therapy that can be used as a stand-alone intervention or to supplement other treatments.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplement 1 00526-2021.SUPPLEMENT1 (91.3KB, pdf)
Supplement 2 00526-2021.SUPPLEMENT2 (14KB, pdf)
Supplement 3 00526-2021.SUPPLEMENT3 (13.8KB, pdf)
Supplement 4 00526-2021.SUPPLEMENT4 (73KB, pdf)
Supplement 5 00526-2021.SUPPLEMENT5 (128KB, pdf)
Supplement 6 00526-2021.SUPPLEMENT6 (61.7KB, pdf)
Footnotes
Provenance: Submitted article, peer reviewed.
This article has supplementary material available from openres.ersjournals.com
This study is registered at www.clinicaltrials.gov with identifier number NCT04450862. Data availability: The data that support the findings of this study are available from the corresponding author, G.H. Rawlings, upon reasonable request.
Conflict of interest: G.H. Rawlings has nothing to disclose.
Conflict of interests: N. Beail has nothing to disclose.
Conflict of interests: I. Armstrong has nothing to disclose.
Conflict of interests: A.R. Thompson has nothing to disclose.
Support statement: Costs associated with this project were funded by the Pulmonary Hypertension Association, UK. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Bussotti M, Sommaruga M. Anxiety and depression in patients with pulmonary hypertension: impact and management challenges. Vasc Health Risk Manag 2018; 14: 349–360. doi: 10.2147/VHRM.S147173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Somaini G, Hasler E, Muller-Mottet, S, et al. . Anxiety and depression are highly prevalent in pulmonary hypertension and might improve with target therapy. Eur Respir J 2015; 46: Suppl. 59, PA2112. [Google Scholar]
- 3.Wryobeck JM, Lippo G, McLaughlin V, et al. . Psychosocial aspects of pulmonary hypertension: a review. Phys Somat Psychog Disord 2007; 48: 467–475. [DOI] [PubMed] [Google Scholar]
- 4.Lowe B, Grafe K, Ufer C, et al. . Anxiety and depression in patients with pulmonary hypertension. Psychosom Med 2004; 66: 831–836. doi: 10.1097/01.psy.0000145593.37594.39 [DOI] [PubMed] [Google Scholar]
- 5.Pulmonary Hypertension Association UK . Impact of COVID19 on people with PH. Sheffield, PHA UK, 2021.
- 6.Schachinger H, Grob M, Ritz R, et al. . Mental stress increases right heart afterload in severe pulmonary hypertension. Clin Physiol 2000; 20: 483–487. doi: 10.1046/j.1365-2281.2000.00287.x [DOI] [PubMed] [Google Scholar]
- 7.Yorke J, Deaton C, Campbell M, et al. . Symptom severity and its effect on health- related quality of life over time in patients with pulmonary hypertension: a multisite longitudinal cohort study. BMJ Open Respir Res 2018; 5: e000263doi: 10.1136/bmjresp-2017-000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harzheim D, Klose H, Pinado F, et al. . Anxiety and depression disorders in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Respir Res 2013; 14: 104. doi: 10.1186/1465-9921-14-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webster R, Thompson A, Webb TL, et al. . Self-help treatments and stepped care, In: Emmelkamp P, Ehring T, eds. The Wiley handbook of anxiety disorders. West Chichester, John Wiley & Sons, 2014; pp. 1242–1255. [Google Scholar]
- 10.Pasterfield M, Clarke SA, Thompson AR. The development of a self-help intervention to build social confidence in people living with visible skin conditions or scars: a think-aloud study. Scars Burn Heal 2019; 5: 2059513118822954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dugas MJ, Robichaud M. Cognitive-Behavioral Treatment for Generalized Anxiety Disorder: From Science to Practice. New York, Routledge, 2007. [Google Scholar]
- 12.Clark DM. A cognitive approach to panic. Behav Res Ther 1986; 24: 461–470. doi: 10.1016/0005-7967(86)90011-2 [DOI] [PubMed] [Google Scholar]
- 13.Salkovskis PM, Rimes KA, Warwick H, et al. . The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med 2002; 32: 843–853. doi: 10.1017/S0033291702005822 [DOI] [PubMed] [Google Scholar]
- 14.Rawlings GH, Thompson AR, Armstrong I, et al. . Coping styles associated with health-anxiety, depression and health-related quality of life in pulmonary hypertension. Manuscript submitted for publication. 2021.
- 15.Spitzer RL, Kroenke K, Williams J, et al. . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 16.Clark D, Oates M. Improving Access to Psychological Therapies: Measuring improvement and recovery adult services (Version 2). Available at: www.oxfordahsn.org/wp-content/uploads/2015/11/measuring-recovery-2014.pdf, 2014.
- 17.Kroenke K, Spitzer RL, Williams J. The PHQ-9. J Gen Int Med 2001; 16: 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yorke J, Corris P, Gaine S, et al. . emPHasis-10: development of a health- related quality of life measure in pulmonary hypertension. Eur Respir J 2014; 43: 1106–1113. doi: 10.1183/09031936.00127113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yorke J, Moosavi SH, Shuldham C, et al. . Quantification of dyspnoea using descriptors: development and initial testing of the Dyspnoea- 12. Thorax 2010; 65: 21–26. doi: 10.1136/thx.2009.118521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pearlin LI, Schooler C. The structure of coping. J Health Social Behavior 1978; 19: 2–21. doi: 10.2307/2136319 [DOI] [PubMed] [Google Scholar]
- 21.Patel T, Mansell W, Veale D. The cognitive behavioural processes questionnaire: a preliminary analysis within student, mixed clinical and community samples and the identification of a core transdiagnostic process. Cognitive Ther Res 2015; 39: 193–203. doi: 10.1007/s10608-014-9641-9 [DOI] [Google Scholar]
- 22.Whitehead AL, Julious SA, Cooper CL, et al. . Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res 2016; 25: 1057–1073. doi: 10.1177/0962280215588241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haug T, Nordgreen T, Öst LG, et al. . Self-help treatment of anxiety disorders: a meta- analysis and meta- regression of effects and potential moderators. Clin Psychol Rev 2012; 32: 425–445. doi: 10.1016/j.cpr.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 24.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 25.Hayes AF. Introduction to Mediation, Moderation and Conditional Process Analysis. Available at: https://processmacro.org/index.html. [DOI] [PubMed]
- 26.Huxley K. Content analysis, quantitative. London, SAGE Publications, 2020. [Google Scholar]
- 27.Gersh E, Hallford D, Rice SM, et al. . Systematic review and meta-analysis of dropout rates in individual psychotherapy for generalized anxiety disorder. J Anxiety Disord, 2017; 52: 25–33. doi: 10.1016/j.janxdis.2017.10.001 [DOI] [PubMed] [Google Scholar]
- 28.Matthew Prina A, Marioni RE, Hammond CG,et al. . Improving access to psychological therapies and older people: Findings from the Eastern Region. Behav Res Ther 2014; 56: 75–81. doi: 10.1016/j.brat.2014.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godinas L, Iyer K, Meszaros G, et al. . PH CARE COVID survey: an international patient survey on the care for pulmonary hypertension patients during the early phase of the COVID-19 pandemic. Orphanet J Rare Dis 2021; 16: 196. doi: 10.1186/s13023-021-01752-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ 2015; 351: h4672. doi: 10.1136/bmj.h4672 [DOI] [PubMed] [Google Scholar]
- 31.Hoeper MM, Gibbs SR, The changing landscape of pulmonary arterial hypertension and implications for patient care. Eur Respir Rev 2014; 23: 450–457. doi: 10.1183/09059180.00007814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halimi L, Marin G, Molinari N, et al. . Impact of psychological factors on the health-related quality of life of patients treated for pulmonary arterial hypertension. J Psychosomatic Research 2018; 105: 45–51. doi: 10.1016/j.jpsychores.2017.12.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplement 1 00526-2021.SUPPLEMENT1 (91.3KB, pdf)
Supplement 2 00526-2021.SUPPLEMENT2 (14KB, pdf)
Supplement 3 00526-2021.SUPPLEMENT3 (13.8KB, pdf)
Supplement 4 00526-2021.SUPPLEMENT4 (73KB, pdf)
Supplement 5 00526-2021.SUPPLEMENT5 (128KB, pdf)
Supplement 6 00526-2021.SUPPLEMENT6 (61.7KB, pdf)