Abstract
Background
The microbial community affects the occurrence, development, metastasis and treatment response of cancers. But the detailed role and characteristics of lung microbiota (LM) in non-small cell lung cancer (NSCLC) are not fully known. For NSCLC associated microbiota analysis, it is valuable to combine multiple levels of detection, e.g., tumor, blood plasma, and bronchoalveolar fluid (BALF), but not single tissues.
Methods
This study collected above three sample types from NSCLC patients free from lung infection and aimed to describe their LM features using sequencing techniques. All patients diagnosed at the Department of Oncology in Shijiazhuang People’s Hospital with stage III or IV NSCLC from May 2019 to April 2020 were enrolled. All 37 pieces of tumor tissues and 6 blood samples were sent for pathogen targeted sequencing; for the BALF samples, 4 were used for pathogen targeted sequencing and 2 were sent for 16S ribosomal DNA (rDNA) sequencing.
Results
We detected 49 pathogenic microorganisms (PMs) in the 37 tumor samples, 28 PMs in the 4 BALF samples, and 14 PMs in the 6 plasma samples. Overall, there were 5 common PMs in 3 types of samples. Between the tumor and BALF samples, there were another 11 common elements. In the 5 tumor-plasma pairs, the presence of a specific PM in blood was not necessarily consistent with that in the tumor. In the tumor-BALF pairs, the PM diversity was dramatically higher in the BALF than in the tumor. The PMs detected in the BALF could largely cover the PMs in the tumor. In the BALF 16S rDNA sequencing, there were 82 common operational taxonomic units (OTUs), and the microbiota in the BALF of advanced NSCLC patients exhibited some similarity.
Conclusions
This study showed the unique features of LM. The amount of intra-tumoral PMs was not necessarily consistent with that in the blood, but there was an obvious correlation between the intra-tumoral microbiota and that in the BALF. It is convenient and non-invasive to obtain BALF. Detection of LM classification and abundance in the BALF may help evaluate the severity of NSCLC.
Keywords: Non-small cell lung cancer (NSCLC), intra-tumoral microbiota, bronchoalveolar fluid (BALF), pathogen targeted sequencing, microbial classification
Introduction
Non-small cell lung cancer (NSCLC), the main type of lung cancer (LC), is among the top causes of cancer deaths worldwide. In terms of pathological classification, adenocarcinomas (ADC) and squamous cell carcinomas (SCC) are two major subtypes of NSCLC. Recently, studies have confirmed that the lung microbiome (LM) differs among clinicopathology types (1), and lung microbial flora may impact the development of NSCLC (2). However, the detailed role and characteristics of LM in NSCLC are not fully known (3). In addition, existing studies commonly presented the comorbidity of respiratory infection and NSCLC onset. If a patient does not have a definite respiratory infection, studies that examine the chronic impacts of LM on NSCLC development are still scarce. Furthermore, existing studies mainly focus on the LC tissues. However, LM composition can vary among lung segments (3). Therefore, it is more valuable to combine multiple levels of detection, e.g., tumor tissues, blood plasma, and bronchoalveolar fluid (BALF), but not single tissues. Currently, most studies use NSCLC tumors alone or in combination with distal samples (e.g., intestinal flora, which should have a low correlation with NSCLC development and progression) (4). Previously, scholars have paid more attention to the gut microbiota mainly because these samples are easier to obtain in comparison with lung samples. However, local samples can directly modulate NSCLC development and influence the treatment efficacy. For example, local tumor microbial signatures are markers for immunotherapy response in NSCLC (5). So far, very limited studies have applied different sample types form LC patients to conduct the comprehensive analysis of LM features. Therefore, we collected three types of samples (tumors, BALF, and blood plasma) in this study and applied sequencing to describe the features of NSCLC-associated LM. We present the following article in accordance with the MDAR reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-92/rc).
Methods
Patients
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of Shijiazhuang People’s Hospital (No. 2019015). Initially, from May 2019 to April 2020, all NSCLC (ADC or SCC) patients in stage III or stage IV at the Department of Oncology in Shijiazhuang People’s Hospital were enrolled. Before sampling, written informed consent was obtained from all participants. At the time of lung biopsy, surgery, or bronchoscopy, samples were obtained, numbered, and stored at −80 °C. Three types of samples, including the tumor tissue (through surgery or biopsy), BALF, or blood were collected, and then these samples were sent for pathogen targeted sequencing or 16S ribosomal DNA (rDNA) sequencing. The following patients were excluded: (I) those with a confirmed lung infection; or (II) for whom no sequencing result was obtained. Finally, 54 patients (28 in stage III and 26 in stage IV) were included (Table 1). There were 38 males and 16 females, with an average age of 66.1 years (±8.66). The ratio of ADC, SCC, adenosquamous carcinoma (ASC), and other types of NSCLCs were 50.0%, 38.9%, 5.6%, and 5.6%, respectively. About 60% of patients were smokers, and their annual consumption was 664.06 (±400.85) cigarettes. The pathological results showed that there were 14 PD-L1 positive cases and 13 patients with EGFR mutation. From these patients, we collected 37 pieces of tumor tissues, 6 BALF samples, and 6 blood plasma samples. Within these, there were 5 matched samples of tumor-plasma pairs and 2 matched samples of tumor-BALF pairs. All tumor samples and blood samples were sent for pathogen targeted sequencing; for the 6 BALF samples, 4 were used for pathogen targeted sequencing and 2 were sent for 16S rDNA sequencing.
Table 1. Clinical characteristics of enrolled stage III and IV NSCLC patients.
| Characteristics | Case number | %/mean (SD) |
|---|---|---|
| Total cases | 54 | 100 |
| Gender | ||
| Male | 38 | 71.7 |
| Female | 16 | 28.3 |
| Smoking history | ||
| No | 22 | 40.74 |
| Yes | 32 | 59.26 |
| Major stage | ||
| III | 28 | 51.9 |
| IV | 26 | 48.1 |
| Pathological type | ||
| ADC | 27 | 50.0 |
| SCC | 21 | 38.9 |
| ASC | 3 | 5.6 |
| Others | 3 | 5.6 |
| PD-L1 positive | 14 | 25.9 |
| EGFR mutation | 13 | 24.1 |
| Age (years) | 54 | 66.1 (8.66) |
| Cigarettes per year | 32 | 664.06 (400.85) |
NSCLC, non-small cell lung cancer; ADC, adenocarcinomas; SCC, squamous cell carcinomas; ASC, adenosquamous carcinoma.
Pathogen targeted sequencing and 16S rDNA sequencing
We used all the collected tumor samples to perform the pathogen targeted sequencing. The sequencing process was performed in the Pathogeno One Pan-Infectious Pathogen High-Throughput Sequencing system by the Shanghai Bingyuan Medical Technology Co., Ltd. cat ID Pathogeno 090118. Two rounds of polymerase chain reaction (PCR) were conducted. The report of each patient was acquired and documented in the dataset. For each known pathogenic microorganism (PM), 2 fields were used for analysis: the readings of known bacteria, and the presence of each microorganism. The intersections of detected PM in different samples were expressed by a Venn diagram. Another 2 BALF samples were sent for 16S rDNA sequencing and microbial classification. This step was performed by Sangon Biotech. Co., Ltd. The DNA was extracted by the EZNATM Mag-Bind Soil DNA Kit according to the official instructions. The abundance and taxonomic of terms were reported, and two samples were analyzed comparatively.
Statistical analysis
Data were analyzed using SPSS 22.0 software. For desperation and comparison of frequencies of the categorical data, Pearson χ2 test or Fisher’s exact test were used. Quantitative data were compared between the two groups using t-test (in normal distribution) or a non-parametric test (Mann-Whitney test, not in normal distribution). Heatmaps of the LM counts were generated by the heatmap R package. A Venn diagram was drawn to show the microorganism intersection of three sample types.
Results
Common PMs in different NSCLC samples
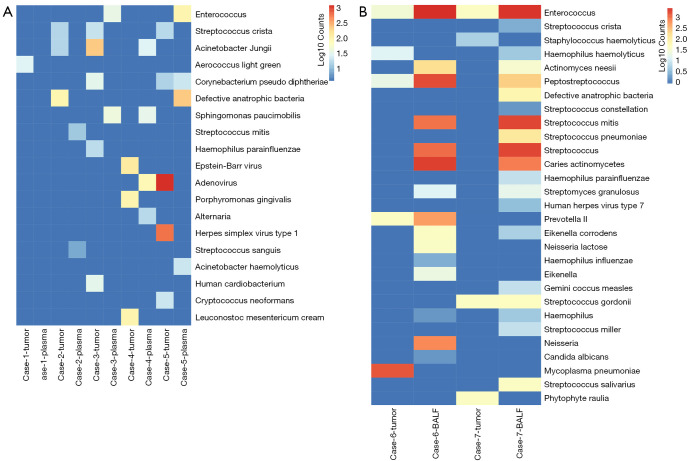
The frequency of each positive PM in pathogen targeted sequencing is listed in Figure 1. Together, we detected 49 PMs in the 37 tumor samples (Figure 1A), 28 PMs in the 4 BALF samples (Figure 1B), and 14 PMs in the plasma samples (Figure 1C). In tumors, the high-frequency PMs that we identified were Streptococcus pneumoniae, Acinetobacter Jungii, Haemophilus parainfluenzae, Enterococcus, and Haemophilus haemolyticus. In BALF, Streptococcus mitis, Enterococcus, Actinomyces Neesii, Peptostreptococcus, and Streptococcus constellatus were frequently observed. In blood, Enterococcus, Sphingomonas paucimobilis and Adenovirus were identified as high-frequency PMs. A Venn diagram was drawn to show the microorganism intersection of three sample types (Figure 1D). Overall, there were 5 common PMs in 3 types of samples, which were Haemophilus parainfluenzae, Enterococcus, Staphylococcus haemolyticus, Peptostreptococcus, and Defective anatrophic bacteria. Between the tumor and BALF samples, there were other 11 common elements, which were Streptococcus pneumoniae, Haemophilus haemolyticus, Streptococcus crista, Prevotella II, Haemophilus, Haemophilus influenzae, Actinomyces Neesii, Streptococcus constellatus, Streptococcus gordonii, human herpes virus type 7, and Neisseria lactose. Theoretically, these common PMs can cause lung infections when the immune system is compromised, and thus deserve more attention in LC development.
Figure 1.
Common PMs in different NSCLC samples. (A) There were 49 PMs in the 37 tumor samples. (B) There were 28 PMs in the 4 BALF samples. (C) There were 14 PMs in the plasma samples. (D) The Venn diagram showing the intersection of the 3 sample types: there were 5 common PMs in the 3 types of samples: Haemophilus parainfluenzae, Enterococcus, Staphylococcus haemolyticus, Peptostreptococcus, and Defective anatrophic bacteria. PMs, pathogenic microorganisms; NSCLC, non-small cell lung cancer; BALF, bronchoalveolar fluid.
Next, the paired comparison of different samples from the sample’s patient was performed. In the 5 tumor-plasma pairs, the diversities of PMs were similar in blood to the tumor tissue. But the presence of a specific PM in blood was not necessarily consistent with that in the tumor (Figure 2A). In the 2 tumor-BALF pairs (Figure 2B), the correlation was more obvious, and we found that the diversity was dramatically higher in BALF than in the tumor, which differed from plasma samples. The PMs detected in BALF could cover the PMs in the tumor. In addition, enterococcus was observed in both types of samples in 2 patients. This result suggests that the exact role of Enterococci in the development of LC is worthy of in-depth study.
Figure 2.
PM analysis of 5 tumor-plasma pairs (A) and 2 tumor-BALF pairs (B). (A) The diversities of PMs were similar in blood and in the tumor tissue. But the presence of a specific PM in blood was not necessarily consistent with the presence in the tumor. (B) There was a similarity between tumor and BALF, but the diversity was higher in BALF than in the tumor, and the PMs detected in BALF could largely cover the PMs in the tumor. PM, pathogenic microorganism; BALF, bronchoalveolar fluid.
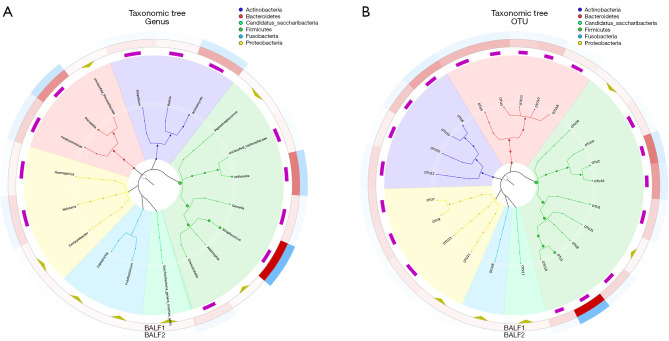
Microbial classification of the BALF samples
Two BAFL samples derived from 2 male advanced NSCLC patients were used for 16S rDNA sequencing. Based on the microbial classification results, there were 104 operational taxonomic units (OTUs) found in 1 BALF sample and 127 OTUs in the other BALF sample, between which there were 82 common OTUs. At the genus level and the OTU level, the graphic taxonomic trees are shown in Figure 3A,3B. Although only 2 samples were collected, their abundance of microbiota exhibited some similarity. Overall, Firmicutes and Bacteroidetes (at the phylum level), Bacteroidia and Bacilli (at the class level), Streptococcaceae and Prevotellaceae (at the phylum level), Streptococcus and Prevotella (at the genus level), and OTU 1, 3, 4, and 10 (at the OTU level) were commonly abundant in the LC BALF.
Figure 3.
Microbial classification based on 16S rDNA sequencing in BALF. Two BAFL samples derived from 2 male advanced NSCLC patients were used for 16S rDNA sequencing. (A) The graphic taxonomic trees of genus. (B) The graphic taxonomic trees of OTUs. rDNA, ribosomal DNA; BALF, bronchoalveolar fluid; NSCLC, non-small cell lung cancer; OTUs, operational taxonomic units.
Discussion
In recent years, metagenomics tools have revealed some important PMs related to LC, such as Haemophilus influenzae, Granulicatella, Abiotrophia, Streptococcus pneumoniae, Acidotrophic bacteria, Klebsiella, Moraxella catarrhalis, and Mycobacterium tuberculosis, among others (6-9). In support, the gut-lung axis may also impact the outcome of chemotherapy and later survival through the impact of microbiota. Patients with chronic respiratory diseases often have alteration of the composition and function of intestinal microbiota besides LM. Gut microbiota can affect respiratory immunity and barrier function through the lung-gut microbiota, resulting in altered prognosis of chronic respiratory diseases (10). However, if the patient also has a lung infection, the influence of PM on NSCLC development is obscured. In this work, we depicted the microbiota features of stage III and IV NSCLC patients without a lung infection We found that: (I) the abundance of intra-tumoral microbiota was rich, and the composition of flora was unique; (II) the intra-tumoral PMs were not necessarily consistent with PMs in the blood; and (III) there was an obvious correlation between the intra-tumoral microbiota and that in the BALF, and detection of microbial classification and abundance in the BALF may help evaluate the NSCLC tumor condition. To summarize, an overview diagram of the influence of LM is shown in Figure 4. These results suggest that the alteration of PMs may cause a change in the lung microenvironment, and the chronic toxicity in this microenvironment may drive the tumorigenesis.
Figure 4.
An overview diagram of the influence of LM on LC development. LM, lung microbiota; LC, lung cancer.
The causal role of microbiome in tumor development has always been controversial. However, the detailed mechanisms in this carcinogenic environment are complex. The direct toxicity of lung PMs and the inflammation induced by PMs are two major risk factors related to LC development. PMs and other infectious agents contribute to 20% of cancers (11). Their dysbiosis can cause direct damage and reactive oxygen species production (12). Moreover, chronic PM related inflammatory mechanisms (e.g., TLRs, NF-κB, and STAT3) can greatly impact invasion and angiogenesis, which are known risk factors of malignant progression (13-15). Besides these direct mechanisms, locally entrenched LM may impact pulmonary immunity. LM may impact the immune system, and the immunosuppressive environment can also accelerate LC development (12). The microbiota-immune cross talk can activate tissue-resident lymphocytes to establish a protumorigenic microenvironment (16). For example, it has been reported that microbiota influences tissue residency and peripheral recruitment of the suppressor T regulatory cell/NK cell axis by shaping a specific tumor microbiome microenvironment (17). However, most of these findings were observed in gastrointestinal cancers, and the characteristics of LM in the advanced and middle-advanced stages of NSCLC patients are yet to be investigated. Whether or not bacteria play a causal role in tumorigenesis, it is necessary to explore the interaction between LM and cancer phenotypes, immune system, and the molecular interactions with tumor cells.
In the limited existing studies, 9 bacteria were recently found to be enriched in the lungs of NSCLC patients (18), and these may change the infiltration rate of T and B cells in LC tissues. A descriptive study used 3 types of samples and observed some common PMs shared by 3 types, such as Haemophilus parainfluenzae, Enterococcus, Staphylococcus haemolyticus, Peptostreptococcus, and Defective anatrophic bacteria. This study found that these PMs may have close links to NSCLC development. In particular, Enterococcus was repeatedly detected in tumor tissues and liquid samples, and its presence in the BALF was highly consistent with the presence of a tumor. Enterococcus (in lung or gut) has been suggested to be a bacterial biomarker in the screening of LC (19,20). However, this conclusion can be questioned. A Chinese study published in 2020 showed a decreased abundance of Prevotella, Streptococcus, Enterococcus, and Roseburia in the LC patients versus healthy subjects. This shows that different populations may have different may trends of PMs during LC development. For example, some scholars reported that Streptococcus and Acinetobacter were enriched in LC tissue and sputum samples (9,19). Therefore, LM may have different roles in promoting carcinogenesis and maintaining homeostasis under different conditions. During LC development, if the microenvironment is altered by tumor, which is unfavorable for LMs, the LMs may exert an anti-tumoral effect in all probability.
The value of this study is that our findings may provide some reference for not only LC diagnosis but also the further treatment and prognosis. The further study can apply the differential LMs to establish LC screening models. Besides, the detailed impacts of common LMs in different samples can be further investigated, towards which the rational use of antibiotics may help improve the treatment effect of LC. Our study had some limitations. First, as a descriptive study, the difficulties between NSCLC and normal controls were unknown. We will conduct comparative studies to deepen the understanding of the influence of LMs. Second, due to the limited sample size, the matched pairs (tumor-BALF, tumor-plasma, or pathogen targeted sequencing -16S rDNA sequencing) were not sufficient to support a consistency of LMs between different sample types. Third, due to the small sample size, it was not feasible to observe differences in microbiome composition among different clinicopathologies, stages, and treatment outcomes. In particular, it merits more attention in the prognostic role of LMs in LC. The knowledge of this field is very limited. For example, Haemophilus parainfluenzae has been regarded as an indicator of LM changes triggered by preoperative prophylaxis in LC patients (21). In our pilot observation, we also noticed that the presence of Haemophilus parainfluenzae was related to the poorer PFS of stage-IV patients and Staphylococcus haemolyticus infection was linked to the longer PFS. But the conclusion is still to be drawn after enough samples have been collected.
Conclusions
This study showed the unique features of LM and their abundance in patients with NSCLC. The intra-tumoral PMs were not necessarily consistent with the PMs in the blood, but there was a correlation between the intra-tumoral microbiota and the PMs in the BALF. Detection of microbial classification and abundance in the BALF may help to evaluate the severity of NSCLC.
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of Shijiazhuang People’s Hospital (No. 2019015) and informed consent was taken from all the patients.
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-92/rc
Data Sharing Statement: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-92/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-92/coif). The authors have no conflicts of interest to declare.
(English Language Editor: C. Mullens)
References
- 1.Huang D, Su X, Yuan M, et al. The characterization of lung microbiome in lung cancer patients with different clinicopathology. Am J Cancer Res 2019;9:2047-63. [PMC free article] [PubMed] [Google Scholar]
- 2.Liu G, Gu A, Mechanism E M. and Research Progress of Microbiome in the Development of Lung Cancer. Zhongguo Fei Ai Za Zhi 2020;23:948-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zheng L, Sun R, Zhu Y, et al. Lung microbiome alterations in NSCLC patients. Sci Rep 2021;11:11736. 10.1038/s41598-021-91195-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu H, Gao NL, Tong F, et al. Alterations of the Human Lung and Gut Microbiomes in Non-Small Cell Lung Carcinomas and Distant Metastasis. Microbiol Spectr 2021;9:e0080221. 10.1128/Spectrum.00802-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boesch M, Baty F, Albrich WC, et al. Local tumor microbial signatures and response to checkpoint blockade in non-small cell lung cancer. Oncoimmunology 2021;10:1988403. 10.1080/2162402X.2021.1988403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin FC, Huang JY, Tsai SC, et al. The association between human papillomavirus infection and female lung cancer: A population-based cohort study. Medicine (Baltimore) 2016;95:e3856. 10.1097/MD.0000000000003856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greathouse KL, White JR, Vargas AJ, et al. Interaction between the microbiome and TP53 in human lung cancer. Genome Biol 2018;19:123. 10.1186/s13059-018-1501-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang LX, Ren HY, Zhou HJ, et al. Simultaneous Detection of 13 Key Bacterial Respiratory Pathogens by Combination of Multiplex PCR and Capillary Electrophoresis. Biomed Environ Sci 2017;30:549-61. [DOI] [PubMed] [Google Scholar]
- 9.Hosgood HD, 3rd, Sapkota AR, Rothman N, et al. The potential role of lung microbiota in lung cancer attributed to household coal burning exposures. Environ Mol Mutagen 2014;55:643-51. 10.1002/em.21878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi CY, Yu CH, Yu WY, et al. Gut-Lung Microbiota in Chronic Pulmonary Diseases: Evolution, Pathogenesis, and Therapeutics. Can J Infect Dis Med Microbiol 2021;2021:9278441. 10.1155/2021/9278441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vande Voorde J, Balzarini J, Liekens S. Mycoplasmas and cancer: focus on nucleoside metabolism. EXCLI J 2014;13:300-22. [PMC free article] [PubMed] [Google Scholar]
- 12.Keren N, Konikoff FM, Paitan Y, et al. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environ Microbiol Rep 2015;7:874-80. 10.1111/1758-2229.12319 [DOI] [PubMed] [Google Scholar]
- 13.García-Castillo V, Sanhueza E, McNerney E, et al. Microbiota dysbiosis: a new piece in the understanding of the carcinogenesis puzzle. J Med Microbiol 2016;65:1347-62. 10.1099/jmm.0.000371 [DOI] [PubMed] [Google Scholar]
- 14.Sethi V, Kurtom S, Tarique M, et al. Gut Microbiota Promotes Tumor Growth in Mice by Modulating Immune Response. Gastroenterology 2018;155:33-7.e6. 10.1053/j.gastro.2018.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wei MY, Shi S, Liang C, et al. The microbiota and microbiome in pancreatic cancer: more influential than expected. Mol Cancer 2019;18:97. 10.1186/s12943-019-1008-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi R, Li Y, Liu H, et al. Lung microbiota: Unexploited treasure hidden in the immune microenvironment of lung cancer. Thorac Cancer 2021;12:2964-6. 10.1111/1759-7714.14159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajagopala SV, Vashee S, Oldfield LM, et al. The Human Microbiome and Cancer. Cancer Prev Res (Phila) 2017;10:226-34. 10.1158/1940-6207.CAPR-16-0249 [DOI] [PubMed] [Google Scholar]
- 18.Chang YS, Hsu MH, Tu SJ, et al. Metatranscriptomic Analysis of Human Lung Metagenomes from Patients with Lung Cancer. Genes (Basel) 2021;12:1458. 10.3390/genes12091458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cameron SJS, Lewis KE, Huws SA, et al. A pilot study using metagenomic sequencing of the sputum microbiome suggests potential bacterial biomarkers for lung cancer. PLoS One 2017;12:e0177062. 10.1371/journal.pone.0177062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhuang H, Cheng L, Wang Y, et al. Dysbiosis of the Gut Microbiome in Lung Cancer. Front Cell Infect Microbiol 2019;9:112. 10.3389/fcimb.2019.00112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kosikowska U, Biernasiuk A, Rybojad P, et al. Haemophilus parainfluenzae as a marker of the upper respiratory tract microbiota changes under the influence of preoperative prophylaxis with or without postoperative treatment in patients with lung cancer. BMC Microbiol 2016;16:62. 10.1186/s12866-016-0679-6 [DOI] [PMC free article] [PubMed] [Google Scholar]