Abstract
COVID-19, resulting from the SARS-CoV-2 virus, is a major pandemic that the world is fighting. SARS-CoV-2 primarily causes lung infection by attaching to the ACE2 receptor on the alveolar epithelial cells. However, the ACE2 receptor is also present in intestinal epithelial cells, suggesting a link between nutrition, virulence and clinical outcomes of COVID-19. Respiratory viral infections perturb the gut microbiota. The gut microbiota is shaped by our diet; therefore, a healthy gut is important for optimal metabolism, immunology and protection of the host. Malnutrition causes diverse changes in the immune system by repressing immune responses and enhancing viral vulnerability. Thus, improving gut health with a high-quality, nutrient-filled diet will improve immunity against infections and diseases. This review emphasizes the significance of dietary choices and its subsequent effects on the immune system, which may potentially impact SARS-CoV-2 vulnerability.
Keywords: gut microbiota, SARS-CoV-2, immunotoxicity, nutrition, diet, malnutrition
1. Introduction
Since its outbreak in China, the coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has dramatically disseminated throughout the world. This highly pathogenic positive-sense RNA virus consists of structural proteins, namely spike, membrane, nucleocapsid and envelope proteins [1,2]. A vital factor of viral pathogenesis involves the angiotensin-converting enzyme-2 (ACE2) cellular receptor [3], which facilitates entry of the virus into susceptible cells. The receptor-binding domain of the spike protein binds to the ACE2 receptor activating membrane fusion of the virus to the host cell. Subsequently, viral RNA is released into the cytoplasm, and the infection is established [4]. Interestingly, apart from the lungs, the ACE2 receptor is also expressed in the kidney, gastrointestinal tract [5] and the enterocytes of the ileum and colon [6]. COVID-19 mainly targets the respiratory tract; however, it may fatally progress to multiple organ failure [7]. Although effective vaccines are now available, they do not provide 100% protection against COVID-19 infection; therefore, other intervention strategies should be explored to reduce the severity of the disease. Since certain foods demonstrate beneficial immune responses to respiratory viruses, the diet may be proposed to ease the adverse health consequences of COVID-19 [8,9].
The consequence of viral infections is highly dependent on the host’s nutritional status, as the body is exposed to a significant energetic effort to endure the defences [10]. The gut and commensal microbiota can regulate and be regulated by invasive infections, inducing a positive or suppressive result on the host [11]. To overcome the response to pathogens, a healthy gut microbiome is vital for maintaining an optimal immune system and avoiding immune responses that can prove deleterious to the lungs and other organs [12]. Therefore, it may be plausible to consider the gut for a solution to mitigate SARS-CoV-2 infection. It is also evident that the intestinal tract is a COVID-19 infection target as some infected patients present with vomiting and diarrhoea [13], while infected patients recently presented the SARS-CoV-2 RNA in their stool samples [14].
Diet maintains a vital role in human health as it can either affect the gut microbiota by altering physiological responses of the host or by directly attacking the host response [15]. The complex and dynamic mammalian gut microbial community is important for the maturation and development of mucosal and systemic immune responses [15]. The interplay among the microbiota, consumed nutrients and the immune system thus serve as regulators for homeostasis maintenance and protection from invasive pathogens [15]. During the infection process, it is presumed that the enterocytes are infected, thereby compromising the function of intestinal membranes. The intestine acts as a barrier to inhibit microorganisms and its products from leaking into the bloodstream, which is associated with the cytokine storm [16]. Bacteria in the gut produce pathogen-activated molecular patterns (PAMPs), which induce different immune responses via Toll-like receptors (TLRs) [17], depending on the cell, ligand or receptor type [12]. Inflammatory cytokines are released during SARS-CoV-2 injury, leading to a cytokine storm, which initiates an immune dysregulation through T cells and inflammatory monocytes [18]. Cytokines regulate the body’s response to infections and inflammation, and the production of cytokines is impacted by the gut microbial metabolic processes [19]. Modern lifestyles, which include sleep deprivation, daily stress and unbalanced diets, can influence the onset of a chronic low-inflammation, affecting the immune system negatively [20]. The highest COVID-19 morbidity and mortality are in the elderly, especially those with underlying health conditions related to inflammation and other disorders such as cardiovascular disease and diabetes [21]. Additionally, individuals with these underlying health conditions show a less diverse gut microbiome [22], suggesting a link between aging and shifts in gut diversity and pro-inflammatory states. Nutrition is also directly linked to inflammation and subsequently to immune responses. Malnutrition is a global problem that should not be ignored during the COVID-19 pandemic [23,24]. In malnutrition, the consumption of monotonous diets, abundant in highly processed foods, renders inadequate vitamins and minerals to the host, weakening the immune system and enhancing SARS-CoV-2 susceptibility [10]. Hence, controlling the inflammatory response may, therefore, be a potential strategy to combat the virus.
This review outlines existing literature on the effects of various diets and nutrient consumption on the immune responses to viral pathogens such as the SARS-CoV-2 infection.
2. Regulation of the Gut Microbiota
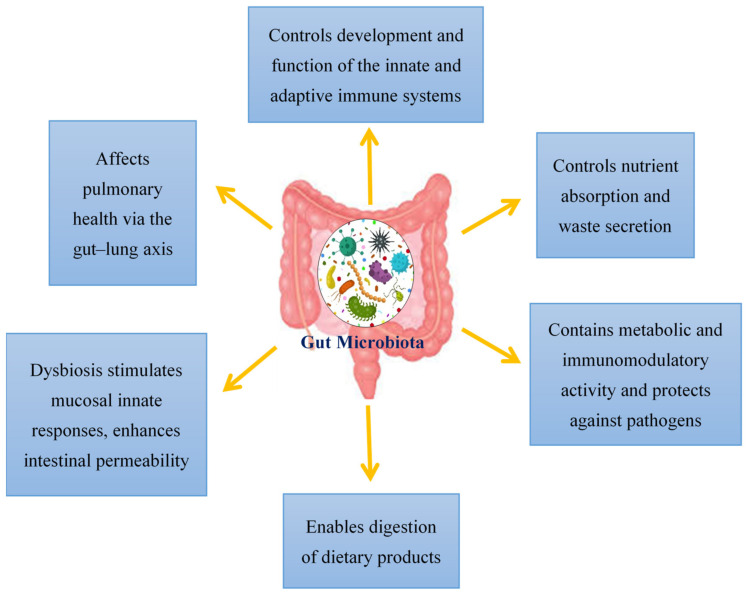
Viral infections have mostly been documented in terms of the virus, the host cell and the host immune system. However, over the past decade, viral infections have been affiliated with the term “microbiota revolution”, which links several pathological manifestations to the gut microbiota and its alterations [25]. The microbiota is a complex group of microorganisms that colonize the mucosal surfaces and are responsible for nutrient absorption and waste secretion [25]. The human gut microbiota contains 1014 resident microorganisms, including fungi, viruses, bacteria and archaea [26]. These microorganisms perform a vital role in health and disease attributing to its metabolic and immunomodulatory activity and protection against pathogens [27]. Commensal bacteria are particularly important for shaping the host immune system and triggering its responses [28,29]. The gut controls the formation and action of the adaptive and innate immune system by tuning immune cells for inflammatory responses and maintaining immune homeostasis [30]. This affects the host’s susceptibility to various diseases; therefore, in SARS-CoV-2 infection, a healthy gut microbiota is crucial for sustaining an optimum immune system which averts uncontrolled inflammatory responses [30]. Modifications of the gut microbiota are characterized by multiple factors, with the main cause being viral infections [25]. Additionally, the gut microbiota also affects pulmonary health via a crosstalk of the lungs and gut microbiota, known as the gut–lung axis [31]. This gut–lung axis is bidirectional; therefore, when microbial endotoxins affect the lungs via the blood causing inflammation, and the gut microbiota may also be affected [32]. The hosts gut microbiota enables the digestion of various dietary products. Dysbiosis of the gut microbiota stimulates mucosal innate immune responses and enhances the permeability of the intestine. This leads to the transfer of pathogenic organisms, allowing detrimental metabolites to access the intestinal epithelium and promoting disease severity [33]. Additionally, a link between ACE2 and the gut microbiota has also been documented. In a mouse model, ACE2 deficiency impaired tryptophan homeostasis, which altered the gut microbiome and inflammatory response [34]. In intestinal epithelial cells, the ACE2 receptor may also control nutrient uptake by attaching to amino acid transporters, suggesting that SARS-CoV-2 may compete against protein nutrients and disrupt absorption via the ACE2 receptor [35,36]. This brings about a possible link between SARS-CoV-2 infections and how the gut microbiota may impact infection severity (Figure 1).
Figure 1.
An overview of the functions of the gut microbiota in the host.
3. The Role of ACE2 in the Gut
The type I membrane-anchored glycoprotein, ACE2, encloses 805 amino acids and contains an N-terminal peptidase domain along with a C-terminal collectrin-like domain [37]. ACE2 is a negative regulator of the Renin–Angiotensin System (RAS), thus providing relief from the harmful effects facilitated by angiotensin (Ang) II signalling via the Ang II receptor type I (AT1R) [38]. ACE2 also demonstrates RAS-independent roles which promote intestinal dysbiosis through loss of ACE2 expression or function [39]. This supports the gastrointestinal symptoms experienced by COVID-19 patients [40]. The gut microbiota also controls ACE2 expressions and therefore plays a role in COVID-19 severity and contagion [41].
Activity of intracrine gut ACE2 encompasses modulation of electrolyte homeostasis, gastrointestinal epithelial fluid, gastrointestinal mucosal inflammation, smooth muscle control and gut-specific fibrosis [42]. In the gut, ACE2 shares a site with B0AT1 and functions as a membrane trafficking chaperone of B0AT1, which controls the sodium-dependent uptake of tryptophan and glutamine (neutral amino acids) into intestinal cells [41]. Animal ACE2-knockout studies displayed altered gut microbial composition, decreased tryptophan serum levels and reduced small intestinal antimicrobial peptide (AMPs) expression [34] in addition to reduced AMP results in dysbiosis, enhanced pathogen levels and impaired gut microbiota [43]. It is proposed that AMP expression and composition of the gut microbiota are regulated by mTOR activation via the tryptophan-nicotinamide pathway and/or nutrient sensing (Figure 2) [34,39].
Figure 2.
The role of ACE2 in the intestine. ACE2 is required for B0AT1 amino acid transporter that mediates tryptophan uptake. Tryptophan triggers antimicrobial peptide secretion via the mTOR pathway, which can alter the gut microbiota composition. Upon SARS-CoV-2 infection, ACE2 is downregulated, leading to aberrant absorption of tryptophan and antimicrobial peptides. This subsequently alters the gut microbiota, conferring susceptibility to inflammation (created with BioRender.com, accessed on 25 October 2021).
During SARS-CoV-2 infection, luminal ACE2 levels are downregulated, impacting gut permeability, nutrient transport and local and systemic inflammation. In the luminal surface of enterocytes, ACE2 deficiency enhances Ang II and reduces Ang1-7. This Ang1-7 decrease in turn activates AT1R and increases gut permeability linked to leaky gut syndrome [39], which may facilitate a cytokine storm [44]. In addition, ACE2 deficiency downregulates ACE2-B0AT1 complexes, hindering neutral amino acid uptake, which are critical for T-cell function, Toll-like receptor signaling and NF-kβ activation and inflammation [44]. Tryptophan also triggers incretins, which regulate glucose homeostasis and promotes hypoglycemia. Furthermore, loss of ACE2-Mas receptor binding in the gut halts glucose transport mediated by SGLT1 and GLUT luminal glucose transporters [41]. In enterocytes’ luminal surfaces, ACE2 deficiency also involves digestive enzyme degradation to produce free amino acids [41].
4. The Influences of Various Diets and Nutrient Consumption on Viral Infections
Various dietary plans are known to effect the gut microbiota compositional patterns [12]. The gut contains an equilibrium of bacterial species, some of which are required for digestion of dietary fibres [45], while others produce essential nutrients [46]. The current understanding of how the microbiome is altered by dietary fat involves TLR4-mediated inflammation, resulting in impaired immune cell membrane function and shifts in nutrient availability [47,48]. Dietary simple sugars may cause dysbiosis via fluctuations in nutrient concentrations and bacterial functions—thus favouring injurious taxa [46,49,50]. Preliminary animal and culture-based research has demonstrated the ability of the gut microbiome to digest artificial sweeteners, which are deemed non-caloric for humans. Sweeteners can be metabolized into short-chain fatty acids (SCFA) by gut bacteria, which carry various consequences [51]. Although some SCFAs may be favourable, their production may alter the bacterial equilibrium [52,53], activate the TLR4 pathway and/or be converted to absorbable by-products that produce calories [51,54]. In vitro studies propose that processed, simple sugars also enhance blood inflammatory cytokine markers and decrease white blood cell phagocytosis [55]. A high fibre diet increased SCFA levels in the intestine and blood, and decreased lung injury from the respiratory syncytial virus infection [30]. The same effect was seen in mice fed water supplemented with acetic acid [56,57]. A westernized diet, classified by excessive ingestion of red meat, processed food and sugary beverages along with minimal fruit, vegetable and fibre intake, increases the frequency of metabolic diseases like diabetes and obesity, which are linked to systemic low-grade inflammation [58,59] (Table 1). Commonly consumed in developing countries, the western diet is also high in saturated fatty acids, which poses the risk of impairing the adaptive immune system while chronically activating the innate immune system [60]. Wild type mice given diets high in sucrose and fat presented reduced gut microbiota diversity and increased sensitivity to opportunistic pathogens, leading to a reduced occurrence of specific gut barrier protective bacteria [61]. Additionally, enhanced lung tissue macrophage infiltration, specifically in the alveoli, was observed in mice fed a diet high in saturated fat [62]. This is particularly applicable to COVID-19 patients, owing to the role of alveolar damage, inflammation of lung tissue and the increased infection rate in alveolar lung epithelial cells in COVID-19 pathology [63]. In humans, the comparison of the microbial shifts between a vegan, vegetarian and omnivore diet showed a significant increase in β-diversity within 24 h of changing to an animal-derived diet [64]. While saturated fats are highly inflammatory [65,66], excess omega-6 poly-unsaturated fats, found in cooking oils, are implicated in immune responses via various mechanisms including effects on TLR4 [67] and acting as precursors for inflammatory mediators [68,69]. Polyunsaturated fatty acids (PUFAs) are key inflammatory and adaptive immunity mediators, of which omega-3 and omega-6 stimulate anti- and pro-inflammatory effects [70]. Omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) that are known to possess beneficial immunity and inflammation effects. These PUFAs are enriched in fish oils and aid in the production of strong bioactive anti-inflammatory lipid mediators, namely protectins, resolvins and maresins [71]. In a study, the DHA-derived lipid mediator protectin D1 attenuated nucleoprotein mRNA expression of the influenza virus by more than 30%, thus impairing viral replication. Additionally, influenza infected mice were relieved from death upon co-treatment of protectin D1 with peramivir, 48 h after the infection [71]. In another study, DHA and EPA displayed potent anti-Hepatitis C virus activities at 100 µM [72]. Furthermore, based on an expert statement by the European Society for Parenteral and Enteral Nutrition, omega-3 fatty acids may be employed in COVID-19 patients to improve oxygenation [73]. On the contrary, others have expressed caution over the use of omega-3 in COVID-19 patients as evidence showed that increased susceptibility to cellular membrane damage promoted oxidative stress and inflammation [74]. Despite these findings, validated trial data are required for the use of omega-3. Several foods have antioxidant properties [75] and may interact with transcriptional factors that have antioxidant effects, such as nuclear factor erythroid 2–related factor 2 (Nrf2) [9]. Nrf2 can be activated by natural compounds in vegetables, fungi, plants and micronutrients [76], as well as foods containing lactobacillus [77]. Fermentation processes can promote the antioxidant activity of cereals, milk, fruit, fish, vegetables and meat [78] (Table 1). In rural households and village communities, fermented foods like alcoholic drinks, bread, vegetables and cheese have been made and consumed by millions of people for several years [79]. Fermented foods are produced by enzymatic conversions in food and controlled microbial growth [80]. Fermented foods contain live microorganisms and are known to regulate the intestinal microbiome [80,81,82]. Throughout the world, the composition of the microbiome varies among different regions. Genetic predisposition and diet contribute to the inter-individual variability of the gut microbiota, whereas lactobacillus spp. contributes to its diversity and regulates the gastrointestinal tract via oxidative stress [79]. In sub-Saharan Africa, commonly consumed fermented foods include maize, millet, sorghum, fruit and vegetables, some of which make up over 50% of the diet [79]. Kimchi, a staple Korean dish, is made from several fermented vegetables and shows anti-diabetic properties [83]. In vitro and in vivo studies have classified kimchi and sauerkraut as functional foods due to their anti-obesity, anti-constipation and anti-cancer characteristics alongside their ability to improve the immune system [84] (Table 1). Plant-based fermented beverages such as vinegar and kombucha, made from sugared tea, possess several health benefits. Vinegar has anti-obesity, anti-diabetic, antioxidant, anti-hypertensive and anti-microbial properties [85], while the ancient beverage kombucha shows anti-cancer, antioxidant and anti-microbial activity [86]. Additionally, the homemade fermented milk drink, kefir, regulates host immunity and decreases susceptibility to bacterial and viral infections [87]. The Mediterranean diet is known to reduce insulin resistance [88] (Table 1), in which Nrf2 seems to play a role [89]. The European Food Safety Authority performed an ecological study to determine the impact of fermented foodstuffs in COVID-19 mortality. These foods included fermented pickled vegetables, vegetables, milk, yoghurt and sour milk [90]. Among all the foods considered, only fermented vegetables showed a statistically significant COVID-19 mortality rate. Interestingly, for each gram per day increase in fermented vegetable consumed, the COVID-19 death risk was decreased by 35.4% [90]. In an ecological study, the outcomes of cruciferous vegetables, such as broccoli, cauliflower, leafy brassica and head cabbage (white, red and savoy cabbage) were compared to courgette, spinach, cucumber, lettuce and tomato [90]. Among these, head cabbage and cucumber were the only vegetables that showed statistical significance in COVID-19 mortality rate. For each gram per day increase in head cabbage and cucumber consumed, COVID-19 mortality risk decreased by 11–13.6% [90]. Western diets usually lack fermented foods and urbanization in western countries has resulted in changes to the gut microbiome and reduced intestinal diversity [91,92]. In Japan, westernized diets led to microbiome and insulin resistance changes [93]. Consumption of fast foods are characterized to reduce lactobacilli, which is essential for the breaking down of food, nutrient absorption and fighting diseases, in the microbiome [94]. Frequent snacking especially in between meals could lead to gut dysbiosis; therefore, it should be minimized or rather consist of fruit and vegetables [19].
Table 1.
The source of various nutrients and diets and their effects on health.
| Type of Diet/Nutrient | Source | Characteristics |
|---|---|---|
| Mediterranean diet | Vegetables, fruit, nuts, legumes, unprocessed cereals | Reduces insulin resistance. |
| Western diet | Red meat, processed foods, sugary drinks | Increases frequency of metabolic diseases and systemic low-grade inflammation. Impairs adaptive immune system. |
| Fermented foods | Cereals, milk, fruits, vegetables, meat | Antioxidant activity. |
| Kimchi | Anti-obesity, anti-cancer, anti-diabetic and antioxidant. | |
| Sauerkraut | Anti-obesity, anti-cancer and antioxidant. | |
| Fast foods | Take away restaurants | Reduces lactobacilli. |
| Vitamin A | Carrot, sweet potato, green leafy vegetables | Sustains T cells. |
| Vitamin C | Orange, strawberry, mango, red peppers, broccoli, lemon, vegetables | Anti-inflammatory and antioxidant. |
| Vitamin D | Sunlight | antibody-secreting cell functions, Increases anti-inflammatory cytokines and decreases pro-inflammatory cytokines. |
| Vitamin E | Vegetable oils, nuts, seeds, broccoli, spinach | Anti-inflammatory and antioxidant |
| Zinc | Beans, lentils, nuts, sesame, pumpkin seeds, red meat, poultry | Regulates pro-inflammatory responses via NF-κβ |
Vitamins play a role in adaptive and innate immune reactions, with vitamin A and D being primary contributors [95]. Vitamin A sustains T-cell growth while vitamin D maintains antibody-secreting cell functions [96] (Table 1). In hypo-nutritional states, immune dysfunction is related to deficiencies of these vitamins, resulting from monotonous diets that are low in vitamin sources. Among these, other micronutrients also play a role in the immunocompetency of the host against infections, which include vitamins C, E, zinc, iron and selenium [97]. Vitamin A is abundantly found in carrots, sweet potatoes and green leafy vegetables [98]. Although there is minimal information on its role in preventing COVID-19, Briguglio, Pregliasco [10] reported that a vitamin A deficit is predominant in individuals with malnutrition, increasing their vulnerability to SARS-CoV-2 infection. Owing to its anti-inflammatory and antioxidant action, the maintenance of vitamin C levels in the body is vital for protection against pulmonary infections [99] (Table 1). Vitamin C can be acquired in the diet from oranges, strawberries, mango, red peppers, broccoli, lemon and vegetables [98]. Early intravenous and oral administration of high doses of vitamin C has been recommended for COVID-19 treatment and can be used as a preventative measure without any adverse side effects [100]. Vitamin D levels can be affected by limited exposure to the sun and outdoor physical activities [101]. Vitamin D has anti-inflammatory effects (Table 1); thus, administration of this vitamin lowers pro-inflammatory cytokine expressions and increases anti-inflammatory cytokine expressions [102] and may, therefore, effectively suppress the COVID-19 cytokine storm in patients [103]. Due to its protective properties against lung injury and acute respiratory infections, vitamin D2 or D3 supplementation may be used as an approach to inhibit moderate and severe respiratory infection symptoms like those seen in COVID-19 patients [104]. Vitamin E deficiency is observed in malnutrition and obesity and may be a factor for SARS-CoV-2 susceptibility [10]. Vitamin E is primarily acquired from vegetable oils, nuts, seeds, broccoli and spinach, and has been shown to have antioxidant and anti-inflammatory characteristics [105] (Table 1). Vitamin E also plays a role in respiratory tract infections [23]. A study displayed that men with higher serum α-tocopherol (a type of vitamin E) showed reduced mortality from respiratory diseases [106].
Meat, beans, eggs and dark green leafy vegetables provide a source of iron [99]. The link between iron and infections is not yet fully elucidated; however, some studies have documented that iron deficiency predisposes individuals to infections [107], while other studies suggest a protective role [108]. Therefore, the maintenance of iron homeostasis seems prudent in preventing COVID-19. Zinc is another important dietary compound required for optimal immune function, development and maintenance of immune cells [99]. Zinc controls pro-inflammatory responses via NF-κβ while its deficiency alters inflammatory responses (Table 1), increasing inflammation and damage to host tissue [109]. Individuals with insufficient zinc intake show a higher occurrence of obstructive lung disorder [99]. Recently, zinc was identified as a COVID-19 adjuvant, owing to its ability to regulate antiviral immunity and reduce inflammation [110]. For SARS-CoV-2 treatment, certain molecules were examined to prevent the viral enzyme RNA-dependent RNA polymerase affinity. These molecules serve as zinc ionophores, prevent mRNA capping, block elongation of RNA polymerase and promote mutations in viral replication [111,112], thereby acting as a SARS-CoV-2 antagonist. Zinc is sourced in foodstuffs of the Mediterranean diet, including beans, lentils, nuts, sesame, pumpkin seeds, red meat and poultry [99]. Among the Chinese population, preliminary reports indicate a positive link between selenium and COVID-19 cure rates [70], and this is consistent with previous studies showing the antiviral effects of selenium [113]. However, tests are still underway to find the suitable selenium dose required for COVID-19 prevention [99].
Probiotics are a promising tool in clinical research that have been proposed for the use in several pathological conditions. Probiotics contain live organisms; therefore, when administered in adequate amounts, it confers positive effects to patients [114]. Although not fully proven, probiotics has been recommended to combat viral infections and protect the host [115]. Attachment of the virus to the host cell is an important step in infections. Probiotic bacteria may potentially attach to the virus directly, thereby preventing the infectious process [25]. Reports show that lactobacilli can bind to and inactivate viruses via adsorptive and/or trapping mechanisms [25]. Lactobacilli contain immunomodulatory properties and protect from infections by promoting cytokine antiviral responses in the intestinal mucosa, immune cells and respiratory cells [116,117]. Administration of lactobacilli via the nose proved effective against viral respiratory infections, inducing innate immune responses in the epithelium of the airways [118]. In mice, lactobacillus improved defence against respiratory infections by inducing respiratory immune responses and increasing inflammatory signals [119]. Furthermore, lactobacillus casei promotes killing and phagocytosis in alveolar macrophages, which increases expressions of IgA, IFN-γ and TNF-α, thereby aiding the hosts battle against influenza virus [120]. Supplementation of probiotics has been proposed as a complementary remedy for gastrointestinal symptoms and to lower secondary COVID-19 infection risks from microbial translocation in acute cases [121]. Direct evidence of probiotics in COVID-19 treatment is yet to be proven; however, it is suggested that probiotics could serve as a complementary treatment to reduce SARS-CoV-2-induced inflammation and repair damaged intestinal mucosa by modulating the gut microbiota [25].
Another major concern is that the detrimental effects of diet can be passed on to future generations. Maternal diets may shape a child’s flavour preferences, skewing their palette to foods that could influence the tendency towards obesity and unhealthy diets [122]. Furthermore, children also inherit their microbiome from their mother. When the maternal diet has a harmful bacterial imbalance, this imbalance is passed to the child, failing to provide the ideal commensals for immune education during the child’s developmental period [47].
Although research is limited on the direct impact of food choices in COVID-19 prognosis, it is evident from the aforementioned data that diet plays a key role in host immunity. While westernized, sugar rich and high fibre diets impose a negative outcome on immune responses, diets rich in fruit, vegetables, fermented foodstuff, vitamins and probiotics are beneficial for efficient immune function against viral infections. Taking these findings into consideration, we propose that diet could be a key target in the combat and prevention against COVID-19 infections. However, extensive research is required to confirm the direct links between the diet and COVID-19.
5. The Effects of Dietary Choices on ACE2 Expression
A crucial step in SARS-CoV-2 viral entry involves the viral protein attaching to the host cell receptor. The human ACE2 receptor mediates SARS-CoV-2 viral entry as it binds with high affinity to the SARS-CoV-2 spike protein, resulting in the viral envelope and the host cell membrane merging together [123]. Emerging research has demonstrated that the ACE2 gene function and expression can be impacted by dietary intake [124,125]. Preliminary studies have examined the effects of diets rich in fructose on ACE2 protein levels [126] and the effects of high dietary sodium on ACE2 receptor expression [127]; however, this has only been tested in infants. Other research determined the effect of dietary fat consumption on ACE2 expression. Among these, the dietary fat content in high-fat diets varies from 50–60% of total energy consumed [125,128,129]. In a 10-week mice study, ACE2 gene activity was determined in a control group (10% lipids, 14%protein, 76% carbohydrate) versus a high-fat diet group (36% carbohydrates, 14% protein, 50% lipids). Upon assessing the mice liver, it was found that ACE2 levels were decreased in the high-fat diet compared to the control [128]. Similarly, research in retroperitoneal adipose tissue of postnatal rats showed a decrease in ACE2 gene expression after being fed a high-fat diet [125]. Additionally, a diet rich in fats in male mice led to decreased kidney ACE2 activity, while the ovariectomy of female mice fed a high-fat diet resulted in decreased adipose ACE2 activity [129]. There is also consistent research on the role of resveratrol to influence ACE2 expression. This polyphenolic compound is present in plant-derived foods such as grapes, berries, cocoa and red wine, and is known for its protective role in cardiovascular disease, cancer and respiratory illnesses [130,131]. Rats fed a resveratrol diet (50 mg·kg−1/day) displayed upregulated ACE2 protein expression [132]. In another experiment, mice given a combined diet of high-fat and resveratrol significantly upregulated ACE2 expression, in contrast to mice fed a diet high in fat alone [124]. This suggests that dietary resveratrol may assist in preventing the harmful impacts of a high-fat diet on the ACE2 mRNA expression [124]. In a human in vitro study, aortic smooth muscle cells incubated for 24 h with resveratrol displayed a significant increase in ACE2 gene and protein expressions [133].
6. The Risks Imposed by Malnutrition
Worldwide, malnutrition is the main cause of immunodeficiency [134] as it alters both the adaptive and innate immune responses which protect against viral proliferation [135]. Chronic diseases, considered as contributors of severe COVID-19, are frequently linked to protein–energy malnourishment, impairing immune cell activation [136], thereby permitting viral persistence and enhanced inflammatory cell transfer to the lungs [137]. Increased metabolism and extreme nitrogen loss are allied with infectious states; therefore, malnourished persons are disadvantaged due to reduced body reserves [10]. For instance, mice fed protein, zinc and iron in amounts lower than the optimal requirement encountered a drop in effector CD4+ T cells and body weight as compared to normal nourished mice [138]. Various researchers have documented that malnutrition alters immune responses [139], with the most evident change being the functional and structural involution of the thymus, thereby decreasing the T cell response [139,140]. Research also reveals that malnutrition hinders phagocytic functions and altered cytokine and antibody production [141]. Despite the robust relation between infections and malnutrition, the mechanisms driving this association are not entirely understood [142,143]. This limited understanding may be due to the complex interactions between nutrition and infections, which lead to a vicious cycle [144]. During this vicious cycle, infections prompt an inflammatory response, resulting in fever, appetite loss, increased catabolism and intestinal absorption anomalies. These modifications enhance nutritional needs and initiate or aggravate malnutrition [143]. Malnutrition then reduces the gut barrier function and increases the chance of infections [143,145]. This modifies the intestinal microbiota [146] and compromises the activation and generation of immune cells, altering inflammatory adipocytokine regulation and limiting macro- and micronutrient uptake [147,148]. Undernutrition decreases lipid tissue, impairing adipokine production and inducing innate and adaptive immunity restrictions. In malnourished states, production of leptin was downregulated while adiponectin production was upregulated [99]. Adiponectin enhances alternative macrophage activity and secretion of anti-inflammatory cytokines, lowering T cell responses and production of B cells [99]. In addition, the pro-inflammatory responses of immune cells are limited by impaired production of stress hormones in combination with downregulated leptin and upregulated adiponectin production in malnutrition [148]. Ultimately, in malnutrition, pro-inflammatory cytokines (TNF-α, IL-6, IL-8), which are essential for killing pathogens, are reduced, while anti-inflammatory cytokines (IL-10, IL-33) are increased [148]. The prevalence of severe diseases was increased in undernourished children with lower respiratory tract and respiratory syncytial viral infections [149]. Experimental studies on influenza infections revealed that energy and protein malnutrition also prompted the risks of acute infections [137], decreasing virus-specific antibodies and responses of CD8+ T cells [137]. In a cross-sectional study with COVID-19 patients, Li, Zhang [150] indicated that the elderly are often malnourished. They revealed that 27.5% of patients, aged over 65 years, were in danger of malnutrition, while 52.7% were already malnourished [150]. In these cases, the fear of contracting COVID-19, prolonged social isolation during lockdown and the yearning to resume normal routine life caused anxiety, which compromises appetite and promotes malnutrition [150]. Currently, little is known about the impact of malnutrition in COVID-19 patients; however, symptoms such as breathlessness, loss of taste and smell, hyper-metabolism, vomiting and diarrhea present in infected patients may result in malnutrition and loss of body weight [151]. One of the prime roots of immunodeficiency is malnutrition, with 38–78% of ICU patients being malnourished [152]. A study assessing malnutrition in 114 COVID-19 patients revealed that 47 patients were malnourished, with ICU patients showing a significantly high prevalence of malnutrition (66.7%) [151]. In a similar study, Rouget, Vardon-Bounes [153] found that 30 out of 80 admitted COVID-19 patients were malnourished, of which 70% presented severe malnutrition. Furthermore, Abate, Chekole [154] summarized the findings from 14 studies reporting the prevalence of malnutrition in hospitalized COVID-19 patients. Among 4187 hospitalized COVID-19 participants, meta-analysis revealed a pooled prevalence of 49.11% malnutrition, with the highest prevalence seen in the critically ill patients [154]. A retrospective study in China consisting of 139 patients revealed that malnutrition also contributed to prolonged hospitalization of COVID-19 patients [155]. In a cohort of 136 severely ill, ICU admitted COVID-19 patients, 61% had a high nutritional risk [152]. Similarly, 77% of an Italian cohort of elderly hospitalized COVID-19 patients were at nutritional risk, while 50% were malnourished [156]. In France, 42.1% of non-ICU patients were identified with malnutrition, whereas the prevalence of malnutrition in ICU admitted patients reached 66.7% [151]. In Morocco, 14.6% and 65.9% of ICU admitted COVID-19 patients presented malnutrition and were at nutritional risk, respectively [157] (Figure 3).
Figure 3.
The impact of various nutrients and foodstuffs on the immune system of the host (created with BioRender.com, accessed on 25 October 2021).
7. Conclusions
The COVID-19 pandemic imposes a social and economic impact on the world. Social isolation, although being an effective strategy to avoid the spread of the virus, causes anxiety and depression from limited interaction with friends and family. In such situations, sleep deprivation, everyday stress and unbalanced diets induce chronic inflammation that adversely impacts the immune system. Although there are safe and efficient vaccines, it is necessary to explore other potentially useful approaches to ameliorate disease severity. Generally, inflammatory stimuli include viral and bacterial infections, endocrine, toxic, genetic and metabolic factors. However, diet and lifestyle may influence inflammation and subsequently alter functions of the immune system. Research on the gut microbiota has expanded our understanding on infectious and chronic diseases. The diversity of the gut microbiota and its residing beneficial microorganisms may determine the course of infections and diseases. A balanced nutritional status and healthy eating choices are important to manage viral infections, such as those triggered by SARS-CoV-2 in malnutrition. Although there are limited data on the nutritional management of SARS-CoV-2 infection, interventions must be made to decrease inflammation and strengthen the immune system. Some recommendations to enhance host nutrition include increased vitamins, probiotics, high-fibre food, vegetable and fruit consumption but minimized consumption of high-sugar food, processed food, fast foods and high-fat foods, to balance the immune function and suppress the cytokine storm. In addition to the conventional COVID-19 control measures such as social distancing, wearing a mask and sanitizing, it is proposed that fermented vegetables and foods with antioxidant properties may help limit infection severity. While nutrition is a promising tool for COVID-19 management, a better understanding concerning nutrition and SARS-CoV-2 is imperative, as the pathogen fitness might depend on host resource availability. Hence, the relationship between nutritional status, microbiome effects, susceptibility and severity of infections requires further clinical research data to support this claim. While the risk of contracting the virus is not dependent on nutritional status, the degree of severity and response to the pathogen depends on nutritional health. This review thus provides a rationale that the gut microbiota partially mediates the consequences of SARS-CoV-2 on the host’s immune response and may therefore be a COVID-19 treatment and prevention target.
Author Contributions
A.F.: Conceptualization and writing—original draft preparation; T.G.: Conceptualization and writing—review and editing; A.A.C.: Conceptualization and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Research Foundation Grantholder-Linked Stu.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A., et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–292. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ni W., Yang X., Yang D., Bao J., Li R., Xiao Y., Hou C., Wang H., Liu J., Yang D., et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care. 2020;24:422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung W.K., To K.F., Chan P.K., Chan H.L., Wu A.K., Lee N., Yuen K.Y., Sung J.J. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125:1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H., Kang Z., Gong H., Xu D., Wang J., Li Z., Li Z., Cui X., Xiao J., Zhan J., et al. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69:1010–1018. doi: 10.1136/gutjnl-2020-320953. [DOI] [Google Scholar]
- 7.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cena H., Chieppa M. Coronavirus Disease (COVID-19–SARS-CoV-2) and Nutrition: Is Infection in Italy Suggesting a Connection? Front. Immunol. 2020;11:944. doi: 10.3389/fimmu.2020.00944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iddir M., Brito A., Dingeo G., Fernandez Del Campo S.S., Samouda H., La Frano M.R., Bohn T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12:1562. doi: 10.3390/nu12061562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briguglio M., Pregliasco F.E., Lombardi G., Perazzo P., Banfi G. The Malnutritional Status of the Host as a Virulence Factor for New Coronavirus SARS-CoV-2. Front. Med. 2020;7:146. doi: 10.3389/fmed.2020.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li N., Ma W.-T., Pang M., Fan Q.-L., Hua J.-L. The Commensal Microbiota and Viral Infection: A Comprehensive Review. Front. Immunol. 2019;10:1551. doi: 10.3389/fimmu.2019.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhar D., Mohanty A. Gut microbiota and Covid-19- possible link and implications. Virus Res. 2020;285:198018. doi: 10.1016/j.virusres.2020.198018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin L., Jiang X., Zhang Z., Huang S., Zhang Z., Fang Z., Gu Z., Gao L., Shi H., Mai L., et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y., Guo C., Tang L., Hong Z., Zhou J., Dong X., Yin H., Xiao Q., Tang Y., Qu X., et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Statovci D., Aguilera M., MacSharry J., Melgar S. The Impact of Western Diet and Nutrients on the Microbiota and Immune Response at Mucosal Interfaces. Front. Immunol. 2017;8:838. doi: 10.3389/fimmu.2017.00838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Groschwitz K.R., Hogan S.P. Intestinal barrier function: Molecular regulation and disease pathogenesis. J. Allergy Clin. Immunol. 2009;124:3–20. doi: 10.1016/j.jaci.2009.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beutler B. Inferences, questions and possibilities in Toll-like receptor signalling. Nature. 2004;430:257–263. doi: 10.1038/nature02761. [DOI] [PubMed] [Google Scholar]
- 18.Zhou Y., Fu B., Zheng X., Wang D., Zhao C., Qi Y., Sun R., Tian Z., Xu X., Wei H. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl. Sci. Rev. 2020;7:998–1002. doi: 10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalantar-Zadeh K., Ward S.A., Kalantar-Zadeh K., El-Omar E.M. Considering the Effects of Microbiome and Diet on SARS-CoV-2 Infection: Nanotechnology Roles. ACS Nano. 2020;14:5179–5182. doi: 10.1021/acsnano.0c03402. [DOI] [PubMed] [Google Scholar]
- 20.Haspel J.A., Anafi R., Brown M.K., Cermakian N., Depner C., Desplats P., Gelman A.E., Haack M., Jelic S., Kim B.S., et al. Perfect timing: Circadian rhythms, sleep, and immunity—An NIH workshop summary. JCI Insight. 2020;5:e131487. doi: 10.1172/jci.insight.131487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao Q., Hu Y., Dai Z., Xiao F., Wang J., Wu J. The epidemiological characteristics of 2019 novel coronavirus diseases (COVID-19) in Jingmen, Hubei, China. Medicine. 2020;99:e20605. doi: 10.1097/MD.0000000000020605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karst S.M. The influence of commensal bacteria on infection with enteric viruses. Nat. Rev. Microbiol. 2016;14:197–204. doi: 10.1038/nrmicro.2015.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calder P.C., Carr A.C., Gombart A.F., Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020;12:1181. doi: 10.3390/nu12041181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinheiro T.A., Barcala-Jorge A.S., Andrade J.M.O., Pinheiro T.A., Ferreira E.C.N., Crespo T.S., Batista-Jorge G.C., Vieira C.A., Lelis D.F., Paraíso A.F., et al. Obesity and malnutrition similarly alter the renin-angiotensin system and inflammation in mice and human adipose. J. Nutr. Biochem. 2017;48:74–82. doi: 10.1016/j.jnutbio.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Infusino F., Marazzato M., Mancone M., Fedele F., Mastroianni C.M., Severino P., Ceccarelli G., Santinelli L., Cavarretta E., Marullo A.G. Diet Supplementation, Probiotics, and Nutraceuticals in SARS-CoV-2 Infection: A Scoping Review. Nutrients. 2020;12:1718. doi: 10.3390/nu12061718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gill S.R., Pop M., DeBoy R.T., Eckburg P.B., Turnbaugh P.J., Samuel B.S., Gordon J.I., Relman D.A., Fraser-Liggett C.M., Nelson K.E. Metagenomic Analysis of the Human Distal Gut Microbiome. Science. 2006;312:1355. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lloyd-Price J., Abu-Ali G., Huttenhower C. The healthy human microbiome. Genome Med. 2016;8:51. doi: 10.1186/s13073-016-0307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hooper L.V., Gordon J.I. Commensal host-bacterial relationships in the gut. Science. 2001;292:1115–1118. doi: 10.1126/science.1058709. [DOI] [PubMed] [Google Scholar]
- 29.Chervonsky A. Innate receptors and microbes in induction of autoimmunity. Curr. Opin. Immunol. 2009;21:641–647. doi: 10.1016/j.coi.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He L.-H., Ren L.-F., Li J.-F., Wu Y.-N., Li X., Zhang L. Intestinal Flora as a Potential Strategy to Fight SARS-CoV-2 Infection. Front. Microbiol. 2020;11:1388. doi: 10.3389/fmicb.2020.01388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keely S., Talley N.J., Hansbro P.M. Pulmonary-intestinal cross-talk in mucosal inflammatory disease. Mucosal Immunol. 2012;5:7–18. doi: 10.1038/mi.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dumas A., Bernard L., Poquet Y., Lugo-Villarino G., Neyrolles O. The role of the lung microbiota and the gut–lung axis in respiratory infectious diseases. Cell. Microbiol. 2018;20:e12966. doi: 10.1111/cmi.12966. [DOI] [PubMed] [Google Scholar]
- 33.Collins S.M. A role for the gut microbiota in IBS. Nat. Rev. Gastroenterol. Hepatol. 2014;11:497–505. doi: 10.1038/nrgastro.2014.40. [DOI] [PubMed] [Google Scholar]
- 34.Hashimoto T., Perlot T., Rehman A., Trichereau J., Ishiguro H., Paolino M., Sigl V., Hanada T., Hanada R., Lipinski S., et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487:477–481. doi: 10.1038/nature11228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vuille-dit-Bille R.N., Camargo S.M., Emmenegger L., Sasse T., Kummer E., Jando J., Hamie Q.M., Meier C.F., Hunziker S., Forras-Kaufmann Z., et al. Human intestine luminal ACE2 and amino acid transporter expression increased by ACE-inhibitors. Amino Acids. 2015;47:693–705. doi: 10.1007/s00726-014-1889-6. [DOI] [PubMed] [Google Scholar]
- 36.Javed K., Bröer S. Mice Lacking the Intestinal and Renal Neutral Amino Acid Transporter SLC6A19 Demonstrate the Relationship between Dietary Protein Intake and Amino Acid Malabsorption. Nutrients. 2019;11:2024. doi: 10.3390/nu11092024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuba K., Imai Y., Rao S., Gao H., Guo F., Guan B., Huan Y., Yang P., Zhang Y., Deng W. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nat. Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perlot T., Penninger J.M. ACE2–From the renin–angiotensin system to gut microbiota and malnutrition. Microbes Infect. 2013;15:866–873. doi: 10.1016/j.micinf.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kotfis K., Skonieczna-Żydecka K. COVID-19: Gastrointestinal symptoms and potential sources of 2019-nCoV transmission. Anaesthesiol. Intensive Ther. 2020;40157:2020. doi: 10.5114/ait.2020.93867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sajdel-Sulkowska E.M. A Dual-Route Perspective of SARS-CoV-2 Infection: Lung- vs. Gut-specific Effects of ACE-2 Deficiency. Front. Pharmacol. 2021;12:684610. doi: 10.3389/fphar.2021.684610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garg M., Angus P.W., Burrell L.M., Herath C., Gibson P.R., Lubel J.S. The pathophysiological roles of the renin–angiotensin system in the gastrointestinal tract. Aliment. Pharmacol. Ther. 2012;35:414–428. doi: 10.1111/j.1365-2036.2011.04971.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang T., Santisteban M.M., Rodriguez V., Li E., Ahmari N., Carvajal J.M., Zadeh M., Gong M., Qi Y., Zubcevic J., et al. Gut dysbiosis is linked to hypertension. Hypertension. 2015;65:1331–1340. doi: 10.1161/HYPERTENSIONAHA.115.05315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ren W., Rajendran R., Zhao Y., Tan B., Wu G., Bazer F.W., Zhu G., Peng Y., Huang X., Deng J. Amino acids as mediators of metabolic cross talk between host and pathogen. Front. Immunol. 2018;9:319. doi: 10.3389/fimmu.2018.00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stecher B., Hardt W.-D. Mechanisms controlling pathogen colonization of the gut. Curr. Opin. Microbiol. 2011;14:82–91. doi: 10.1016/j.mib.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 46.Brown K., DeCoffe D., Molcan E., Gibson D.L. Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients. 2012;4:1095–1119. doi: 10.3390/nu4081095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myles I.A., Fontecilla N.M., Janelsins B.M., Vithayathil P.J., Segre J.A., Datta S.K. Parental dietary fat intake alters offspring microbiome and immunity. J. Immunol. 2013;191:3200–3209. doi: 10.4049/jimmunol.1301057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ghosh S., DeCoffe D., Brown K., Rajendiran E., Estaki M., Dai C., Yip A., Gibson D.L. Fish oil attenuates omega-6 polyunsaturated fatty acid-induced dysbiosis and infectious colitis but impairs LPS dephosphorylation activity causing sepsis. PLoS ONE. 2013;8:e55468. doi: 10.1371/journal.pone.0055468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chassard C., Lacroix C. Carbohydrates and the human gut microbiota. Curr. Opin. Clin. Nutr. Metab. Care. 2013;16:453–460. doi: 10.1097/MCO.0b013e3283619e63. [DOI] [PubMed] [Google Scholar]
- 50.Koropatkin N.M., Cameron E.A., Martens E.C. How glycan metabolism shapes the human gut microbiota. Nat. Rev. Microbiol. 2012;10:323–335. doi: 10.1038/nrmicro2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Payne A., Chassard C., Lacroix C. Gut microbial adaptation to dietary consumption of fructose, artificial sweeteners and sugar alcohols: Implications for host–microbe interactions contributing to obesity. Obes. Rev. 2012;13:799–809. doi: 10.1111/j.1467-789X.2012.01009.x. [DOI] [PubMed] [Google Scholar]
- 52.Geuns J.M. Stevioside. Phytochemistry. 2003;64:913–921. doi: 10.1016/S0031-9422(03)00426-6. [DOI] [PubMed] [Google Scholar]
- 53.Normén L., Lærke H.N., Jensen B.B., Langkilde A.M., Andersson H. Small-bowel absorption of D-tagatose and related effects on carbohydrate digestibility: An ileostomy study. Am. J. Clin. Nutr. 2001;73:105–110. doi: 10.1093/ajcn/73.1.105. [DOI] [PubMed] [Google Scholar]
- 54.Maslowski K.M., Vieira A.T., Ng A., Kranich J., Sierro F., Yu D., Schilter H.C., Rolph M.S., Mackay F., Artis D. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature. 2009;461:1282–1286. doi: 10.1038/nature08530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sørensen L.B., Raben A., Stender S., Astrup A. Effect of sucrose on inflammatory markers in overweight humans. Am. J. Clin. Nutr. 2005;82:421–427. doi: 10.1093/ajcn/82.2.421. [DOI] [PubMed] [Google Scholar]
- 56.Trompette A., Gollwitzer E.S., Yadava K., Sichelstiel A.K., Sprenger N., Ngom-Bru C., Blanchard C., Junt T., Nicod L.P., Harris N.L., et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat. Med. 2014;20:159–166. doi: 10.1038/nm.3444. [DOI] [PubMed] [Google Scholar]
- 57.Den Besten G., van Eunen K., Groen A.K., Venema K., Reijngoud D.J., Bakker B.M. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 2013;54:2325–2340. doi: 10.1194/jlr.R036012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cani P.D., Amar J., Iglesias M.A., Poggi M., Knauf C., Bastelica D., Neyrinck A.M., Fava F., Tuohy K.M., Chabo C., et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes. 2007;56:1761. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 59.Wellen K.E., Hotamisligil G.S. Inflammation, stress, and diabetes. J. Clin. Investig. 2005;115:1111–1119. doi: 10.1172/JCI25102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Butler M.J., Barrientos R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav. Immun. 2020;87:53–54. doi: 10.1016/j.bbi.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang C., Zhang M., Pang X., Zhao Y., Wang L., Zhao L. Structural resilience of the gut microbiota in adult mice under high-fat dietary perturbations. ISME J. 2012;6:1848–1857. doi: 10.1038/ismej.2012.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tashiro H., Takahashi K., Sadamatsu H., Kato G., Kurata K., Kimura S., Sueoka-Aragane N. Saturated fatty acid increases lung macrophages and augments house dust mite-induced airway inflammation in mice fed with high-fat diet. Inflammation. 2017;40:1072–1086. doi: 10.1007/s10753-017-0550-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.David L.A., Maurice C.F., Carmody R.N., Gootenberg D.B., Button J.E., Wolfe B.E., Ling A.V., Devlin A.S., Varma Y., Fischbach M.A., et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Laugerette F., Furet J.-P., Debard C., Daira P., Loizon E., Géloën A., Soulage C.O., Simonet C., Lefils-Lacourtablaise J., Bernoud-Hubac N. Oil composition of high-fat diet affects metabolic inflammation differently in connection with endotoxin receptors in mice. Am. J. Physiol. Endocrinol. Metab. 2012;302:E374–E386. doi: 10.1152/ajpendo.00314.2011. [DOI] [PubMed] [Google Scholar]
- 66.Liu J., Hu S., Cui Y., Sun M.-K., Xie F., Zhang Q., Jin J. Saturated fatty acids up-regulate COX-2 expression in prostate epithelial cells via toll-like receptor 4/NF-κB signaling. Inflammation. 2014;37:467–477. doi: 10.1007/s10753-013-9760-6. [DOI] [PubMed] [Google Scholar]
- 67.Galli C., Calder P.C. Effects of fat and fatty acid intake on inflammatory and immune responses. Ann. Nutr. Metab. 2009;55:123–139. doi: 10.1159/000228999. [DOI] [PubMed] [Google Scholar]
- 68.Calder P.C. Fatty acids and immune function: Relevance to inflammatory bowel diseases. Int. Rev. Immunol. 2009;28:506–534. doi: 10.3109/08830180903197480. [DOI] [PubMed] [Google Scholar]
- 69.Innis S.M. Dietary lipids in early development: Relevance to obesity, immune and inflammatory disorders. Curr. Opin. Endocrinol. Diabetes Obes. 2007;14:359–364. doi: 10.1097/MED.0b013e3282be90b9. [DOI] [PubMed] [Google Scholar]
- 70.Zhang L., Liu Y. Potential interventions for novel coronavirus in China: A systematic review. J. Med. Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morita M., Kuba K., Ichikawa A., Nakayama M., Katahira J., Iwamoto R., Watanebe T., Sakabe S., Daidoji T., Nakamura S., et al. The lipid mediator protectin D1 inhibits influenza virus replication and improves severe influenza. Cell. 2013;153:112–125. doi: 10.1016/j.cell.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 72.Leu G.Z., Lin T.Y., Hsu J.T. Anti-HCV activities of selective polyunsaturated fatty acids. Biochem. Biophys. Res. Commun. 2004;318:275–280. doi: 10.1016/j.bbrc.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 73.Barazzoni R., Bischoff S.C., Breda J., Wickramasinghe K., Krznaric Z., Nitzan D., Pirlich M., Singer P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020;39:1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shakoor H., Feehan J., Al Dhaheri A.S., Ali H.I., Platat C., Ismail L.C., Apostolopoulos V., Stojanovska L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19? Maturitas. 2021;143:1–9. doi: 10.1016/j.maturitas.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jain S., Buttar H.S., Chintameneni M., Kaur G. Prevention of Cardiovascular Diseases with Anti-Inflammatory and Anti- Oxidant Nutraceuticals and Herbal Products: An Overview of Pre-Clinical and Clinical Studies. Recent Pat. Inflamm. Allergy Drug Discov. 2018;12:145–157. doi: 10.2174/1872213X12666180815144803. [DOI] [PubMed] [Google Scholar]
- 76.Jiménez-Osorio A.S., González-Reyes S., Pedraza-Chaverri J. Natural Nrf2 activators in diabetes. Clin. Chim. Acta. 2015;448:182–192. doi: 10.1016/j.cca.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 77.Senger D.R., Li D., Jaminet S.C., Cao S. Activation of the Nrf2 Cell Defense Pathway by Ancient Foods: Disease Prevention by Important Molecules and Microbes Lost from the Modern Western Diet. PLoS ONE. 2016;11:e0148042. doi: 10.1371/journal.pone.0148042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Melini F., Melini V., Luziatelli F., Ficca A.G., Ruzzi M. Health-Promoting Components in Fermented Foods: An Up-to-Date Systematic Review. Nutrients. 2019;11:1189. doi: 10.3390/nu11051189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bousquet J., Anto J.M., Czarlewski W., Haahtela T., Fonseca S.C., Iaccarino G., Blain H., Vidal A., Sheikh A., Akdis C.A., et al. Cabbage and fermented vegetables: From death rate heterogeneity in countries to candidates for mitigation strategies of severe COVID-19. Allergy. 2020;76:735–750. doi: 10.1111/all.14549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Marco M.L., Heeney D., Binda S., Cifelli C.J., Cotter P.D., Foligné B., Gänzle M., Kort R., Pasin G., Pihlanto A., et al. Health benefits of fermented foods: Microbiota and beyond. Curr. Opin. Biotechnol. 2017;44:94–102. doi: 10.1016/j.copbio.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 81.Dimidi E., Cox S.R., Rossi M., Whelan K. Fermented Foods: Definitions and Characteristics, Impact on the Gut Microbiota and Effects on Gastrointestinal Health and Disease. Nutrients. 2019;11:1806. doi: 10.3390/nu11081806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Filippis F., Pasolli E., Ercolini D. The food-gut axis: Lactic acid bacteria and their link to food, the gut microbiome and human health. FEMS Microbiol. Rev. 2020;44:454–489. doi: 10.1093/femsre/fuaa015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.An S.Y., Lee M.S., Jeon J.Y., Ha E.S., Kim T.H., Yoon J.Y., Ok C.O., Lee H.K., Hwang W.S., Choe S.J., et al. Beneficial effects of fresh and fermented kimchi in prediabetic individuals. Ann. Nutr. Metab. 2013;63:111–119. doi: 10.1159/000353583. [DOI] [PubMed] [Google Scholar]
- 84.Peñas E., Martinez-Villaluenga C., Frias J. Chapter 24—Sauerkraut: Production, Composition, and Health Benefits. In: Frias J., Martinez-Villaluenga C., Peñas E., editors. Fermented Foods in Health and Disease Prevention. Academic Press; Boston, MA, USA: 2017. pp. 557–576. [Google Scholar]
- 85.Ho C.W., Lazim A.M., Fazry S., Zaki U.K.H.H., Lim S.J. Varieties, production, composition and health benefits of vinegars: A review. Food Chem. 2017;221:1621–1630. doi: 10.1016/j.foodchem.2016.10.128. [DOI] [PubMed] [Google Scholar]
- 86.Muhialdin B.J., Zawawi N., Abdull Razis A.F., Bakar J., Zarei M. Antiviral activity of fermented foods and their probiotics bacteria towards respiratory and alimentary tracts viruses. Food Control. 2021;127:108140. doi: 10.1016/j.foodcont.2021.108140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gasmi A., Tippairote T., Mujawdiya P.K., Peana M., Menzel A., Dadar M., Benahmed A.G., Bjørklund G. The microbiota-mediated dietary and nutritional interventions for COVID-19. Clin. Immunol. 2021;226:108725. doi: 10.1016/j.clim.2021.108725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mirabelli M., Chiefari E., Arcidiacono B., Corigliano D.M., Brunetti F.S., Maggisano V., Russo D., Foti D.P., Brunetti A. Mediterranean Diet Nutrients to Turn the Tide against Insulin Resistance and Related Diseases. Nutrients. 2020;12:1066. doi: 10.3390/nu12041066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martucci M., Ostan R., Biondi F., Bellavista E., Fabbri C., Bertarelli C., Salvioli S., Capri M., Franceschi C., Santoro A. Mediterranean diet and inflammaging within the hormesis paradigm. Nutr. Rev. 2017;75:442–455. doi: 10.1093/nutrit/nux013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fonseca S., Rivas I., Romaguera D., Quijal-Zamorano M., Czarlewski W., Vidal A., Fonseca J., Ballester J., Antó J., Basagana X., et al. Association between consumption of fermented vegetables and COVID-19 mortality at a country level in Europe. medRxiv. 2020 doi: 10.1101/2020.07.06.20147025. [DOI] [Google Scholar]
- 91.Bibbò S., Ianiro G., Giorgio V., Scaldaferri F., Masucci L., Gasbarrini A., Cammarota G. The role of diet on gut microbiota composition. Eur. Rev. Med. Pharmacol. Sci. 2016;20:4742–4749. [PubMed] [Google Scholar]
- 92.Wilson A.S., Koller K.R., Ramaboli M.C., Nesengani L.T., Ocvirk S., Chen C., Flanagan C.A., Sapp F.R., Merritt Z.T., Bhatti F., et al. Diet and the Human Gut Microbiome: An International Review. Dig. Dis. Sci. 2020;65:723–740. doi: 10.1007/s10620-020-06112-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yamashita M., Okubo H., Kobuke K., Ohno H., Oki K., Yoneda M., Tanaka J., Hattori N. Alteration of gut microbiota by a Westernized lifestyle and its correlation with insulin resistance in non-diabetic Japanese men. J. Diabetes Investig. 2019;10:1463–1470. doi: 10.1111/jdi.13048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mitsou E.K., Kakali A., Antonopoulou S., Mountzouris K.C., Yannakoulia M., Panagiotakos D.B., Kyriacou A. Adherence to the Mediterranean diet is associated with the gut microbiota pattern and gastrointestinal characteristics in an adult population. Br. J. Nutr. 2017;117:1645–1655. doi: 10.1017/S0007114517001593. [DOI] [PubMed] [Google Scholar]
- 95.Mora J.R., Iwata M., von Andrian U.H. Vitamin effects on the immune system: Vitamins A and D take centre stage. Nat. Rev. Immunol. 2008;8:685–698. doi: 10.1038/nri2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ertesvag A., Engedal N., Naderi S., Blomhoff H.K. Retinoic acid stimulates the cell cycle machinery in normal T cells: Involvement of retinoic acid receptor-mediated IL-2 secretion. J. Immunol. 2002;169:5555–5563. doi: 10.4049/jimmunol.169.10.5555. [DOI] [PubMed] [Google Scholar]
- 97.Gombart A.F., Pierre A., Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020;12:236. doi: 10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Muscogiuri G., Barrea L., Savastano S., Colao A. Nutritional recommendations for CoVID-19 quarantine. Eur. J. Clin. Nutr. 2020;74:850–851. doi: 10.1038/s41430-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Morais A., Aquino J., da Silva-Maia J.K., Vale S., Maciel B.L.L., Passos T.S. Nutritional status, diet and viral respiratory infections: Perspectives for severe acute respiratory syndrome coronavirus 2. Br. J. Nutr. 2021;125:851–862. doi: 10.1017/S0007114520003311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cheng R.Z. Can early and high intravenous dose of vitamin C prevent and treat coronavirus disease 2019 (COVID-19)? Med. Drug Discov. 2020;5:100028. doi: 10.1016/j.medidd.2020.100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Carter S.J., Baranauskas M.N., Fly A.D. Considerations for Obesity, Vitamin D, and Physical Activity Amid the COVID-19 Pandemic. Obesity. 2020;28:1176–1177. doi: 10.1002/oby.22838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lin Z., Li W. The Roles of Vitamin D and Its Analogs in Inflammatory Diseases. Curr. Top. Med. Chem. 2016;16:1242–1261. doi: 10.2174/1568026615666150915111557. [DOI] [PubMed] [Google Scholar]
- 103.Daneshkhah A., Agrawal V., Eshein A., Subramanian H., Roy H.K., Backman V. The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients. medRxiv. 2020 doi: 10.1101/2020.04.08.20058578. [DOI] [Google Scholar]
- 104.Kow C.S., Hadi M.A., Hasan S.S. Vitamin D Supplementation in Influenza and COVID-19 Infections Comment on: “Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths Nutrients 2020, 12(4), 988”. Nutrients. 2020;12:1626. doi: 10.3390/nu12061626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Reiter E., Jiang Q., Christen S. Anti-inflammatory properties of alpha- and gamma-tocopherol. Mol. Asp. Med. 2007;28:668–691. doi: 10.1016/j.mam.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Huang J., Weinstein S.J., Yu K., Männistö S., Albanes D. Relationship Between Serum Alpha-Tocopherol and Overall and Cause-Specific Mortality. Circ. Res. 2019;125:29–40. doi: 10.1161/CIRCRESAHA.119.314944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tansarli G.S., Karageorgopoulos D.E., Kapaskelis A., Gkegkes I., Falagas M.E. Iron deficiency and susceptibility to infections: Evaluation of the clinical evidence. Eur. J. Clin. Microbiol. Infect. Dis. 2013;32:1253–1258. doi: 10.1007/s10096-013-1877-x. [DOI] [PubMed] [Google Scholar]
- 108.Wander K., Shell-Duncan B., Brindle E. Lower incidence of respiratory infections among iron-deficient children in Kilimanjaro, Tanzania. Evol. Med. Public Health. 2017;2017:109–119. doi: 10.1093/emph/eox010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gammoh N.Z., Rink L. Zinc in Infection and Inflammation. Nutrients. 2017;9:624. doi: 10.3390/nu9060624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Skalny A.V., Rink L., Ajsuvakova O.P., Aschner M., Gritsenko V.A., Alekseenko S.I., Svistunov A.A., Petrakis D., Spandidos D.A., Aaseth J., et al. Zinc and respiratory tract infections: Perspectives for COVID-19 (Review) Int. J. Mol. Med. 2020;46:17–26. doi: 10.3892/ijmm.2020.4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xue J., Moyer A., Peng B., Wu J., Hannafon B.N., Ding W.-Q. Chloroquine is a zinc ionophore. PLoS ONE. 2014;9:e109180. doi: 10.1371/journal.pone.0109180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chien M., Anderson T.K., Jockusch S., Tao C., Kumar S., Li X., Russo J.J., Kirchdoerfer R.N., Ju J. Nucleotide Analogues as Inhibitors of SARS-CoV-2 Polymerase. bioRxiv. 2020 doi: 10.1101/2020.03.18.997585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Guillin O.M., Vindry C., Ohlmann T., Chavatte L. Selenium, Selenoproteins and Viral Infection. Nutrients. 2019;11:2101. doi: 10.3390/nu11092101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Marchesi J.R., Adams D.H., Fava F., Hermes G.D., Hirschfield G.M., Hold G., Quraishi M.N., Kinross J., Smidt H., Tuohy K.M., et al. The gut microbiota and host health: A new clinical frontier. Gut. 2016;65:330–339. doi: 10.1136/gutjnl-2015-309990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sanders M.E., Merenstein D.J., Reid G., Gibson G.R., Rastall R.A. Probiotics and prebiotics in intestinal health and disease: From biology to the clinic. Nat. Rev. Gastroenterol. Hepatol. 2019;16:605–616. doi: 10.1038/s41575-019-0173-3. [DOI] [PubMed] [Google Scholar]
- 116.Biliavska L., Pankivska Y., Povnitsa O., Zagorodnya S. Antiviral Activity of Exopolysaccharides Produced by Lactic Acid Bacteria of the Genera Pediococcus, Leuconostoc and Lactobacillus against Human Adenovirus Type 5. Medicina. 2019;55:519. doi: 10.3390/medicina55090519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Waki N., Yajima N., Suganuma H., Buddle B.M., Luo D., Heiser A., Zheng T. Oral administration of Lactobacillus brevis KB290 to mice alleviates clinical symptoms following influenza virus infection. Lett. Appl. Microbiol. 2014;58:87–93. doi: 10.1111/lam.12160. [DOI] [PubMed] [Google Scholar]
- 118.Harata G., He F., Hiruta N., Kawase M., Kubota A., Hiramatsu M., Yausi H. Intranasal administration of Lactobacillus rhamnosus GG protects mice from H1N1 influenza virus infection by regulating respiratory immune responses. Lett. Appl. Microbiol. 2010;50:597–602. doi: 10.1111/j.1472-765X.2010.02844.x. [DOI] [PubMed] [Google Scholar]
- 119.Yoda K., He F., Miyazawa K., Kawase M., Kubota A., Hiramatsu M. Orally administered heat-killed Lactobacillus gasseri TMC0356 alters respiratory immune responses and intestinal microbiota of diet-induced obese mice. J. Appl. Microbiol. 2012;113:155–162. doi: 10.1111/j.1365-2672.2012.05316.x. [DOI] [PubMed] [Google Scholar]
- 120.Hori T., Kiyoshima J., Shida K., Yasui H. Effect of intranasal administration of Lactobacillus casei Shirota on influenza virus infection of upper respiratory tract in mice. Clin. Diagn. Lab. Immunol. 2001;8:593–597. doi: 10.1128/CDLI.8.3.593-597.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Xu K., Cai H., Shen Y., Ni Q., Chen Y., Hu S., Li J., Wang H., Yu L., Huang H., et al. Management of corona virus disease-19 (COVID-19): The Zhejiang experience. J. Zhejiang Univ. Med. Sci. 2020;49:147–157. doi: 10.3785/j.issn.1008-9292.2020.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Beauchamp G.K., Mennella J.A. Flavor perception in human infants: Development and functional significance. Digestion. 2011;83((Suppl. S1)):1–6. doi: 10.1159/000323397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chaudhary M. COVID-19 susceptibility: Potential of ACE2 polymorphisms. Egypt. J. Med. Hum. Genet. 2020;21:54. doi: 10.1186/s43042-020-00099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Oliveira Andrade J.M., Paraíso A.F., Garcia Z.M., Ferreira A.V., Sinisterra R.D., Sousa F.B., Guimarães A.L., de Paula A.M., Campagnole-Santos M.J., dos Santos R.A., et al. Cross talk between angiotensin-(1-7)/Mas axis and sirtuins in adipose tissue and metabolism of high-fat feed mice. Peptides. 2014;55:158–165. doi: 10.1016/j.peptides.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 125.Yu H.-R., Tain Y.-L., Tiao M.-M., Chen C.-C., Sheen J.-M., Lin I.C., Li S.-W., Tsai C.-C., Lin Y.-J., Hsieh K.-S., et al. Prenatal dexamethasone and postnatal high-fat diet have a synergistic effect of elevating blood pressure through a distinct programming mechanism of systemic and adipose renin-angiotensin systems. Lipids Health Dis. 2018;17:50. doi: 10.1186/s12944-018-0701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bundalo M.M., Zivkovic M.D., Romic S., Tepavcevic S.N., Koricanac G.B., Djuric T.M., Stankovic A.D. Fructose-rich diet induces gender-specific changes in expression of the renin-angiotensin system in rat heart and upregulates the ACE/AT1R axis in the male rat aorta. J. Renin Angiotensin Aldosterone Syst. 2016;17:1470320316642915. doi: 10.1177/1470320316642915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mao C., Liu R., Bo L., Chen N., Li S., Xia S., Chen J., Li D., Zhang L., Xu Z. High-salt diets during pregnancy affected fetal and offspring renal renin-angiotensin system. J. Endocrinol. 2013;218:61–73. doi: 10.1530/JOE-13-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Graus-Nunes F., Santos F.d.O., Marinho T.d.S., Miranda C.S., Barbosa-da-Silva S., Souza-Mello V. Beneficial effects of losartan or telmisartan on the local hepatic renin-angiotensin system to counter obesity in an experimental model. World J. Hepatol. 2019;11:359–369. doi: 10.4254/wjh.v11.i4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gupte M., Thatcher S.E., Boustany-Kari C.M., Shoemaker R., Yiannikouris F., Zhang X., Karounos M., Cassis L.A. Angiotensin converting enzyme 2 contributes to sex differences in the development of obesity hypertension in C57BL/6 mice. Arterioscler. Thromb. Vasc. Biol. 2012;32:1392–1399. doi: 10.1161/ATVBAHA.112.248559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Bonnefont-Rousselot D. Resveratrol and Cardiovascular Diseases. Nutrients. 2016;8:250. doi: 10.3390/nu8050250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rauf A., Imran M., Butt M.S., Nadeem M., Peters D.G., Mubarak M.S. Resveratrol as an anti-cancer agent: A review. Crit. Rev. Food Sci. Nutr. 2018;58:1428–1447. doi: 10.1080/10408398.2016.1263597. [DOI] [PubMed] [Google Scholar]
- 132.Tiao M.M., Lin Y.J., Yu H.R., Sheen J.M., Lin I.C., Lai Y.J., Tain Y.L., Huang L.T., Tsai C.C. Resveratrol ameliorates maternal and post-weaning high-fat diet-induced nonalcoholic fatty liver disease via renin-angiotensin system. Lipids Health Dis. 2018;17:178. doi: 10.1186/s12944-018-0824-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moran C.S., Biros E., Krishna S.M., Wang Y., Tikellis C., Morton S.K., Moxon J.V., Cooper M.E., Norman P.E., Burrell L.M., et al. Resveratrol Inhibits Growth of Experimental Abdominal Aortic Aneurysm Associated With Upregulation of Angiotensin-Converting Enzyme 2. Arterioscler. Thromb. Vasc. Biol. 2017;37:2195–2203. doi: 10.1161/ATVBAHA.117.310129. [DOI] [PubMed] [Google Scholar]
- 134.Katona P., Katona-Apte J. The interaction between nutrition and infection. Clin. Infect. Dis. 2008;46:1582–1588. doi: 10.1086/587658. [DOI] [PubMed] [Google Scholar]
- 135.Alwarawrah Y., Kiernan K., MacIver N.J. Changes in Nutritional Status Impact Immune Cell Metabolism and Function. Front. Immunol. 2018;9:1055. doi: 10.3389/fimmu.2018.01055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gerriets V.A., MacIver N.J. Role of T Cells in Malnutrition and Obesity. Front. Immunol. 2014;5:379. doi: 10.3389/fimmu.2014.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Taylor A.K., Cao W., Vora K.P., De La Cruz J., Shieh W.J., Zaki S.R., Katz J.M., Sambhara S., Gangappa S. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J. Infect. Dis. 2013;207:501–510. doi: 10.1093/infdis/jis527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pilotos J., Smith M.R., Johnson C.M., Campbell L., Ibitokou S., Stephens R., Opata M.M. Malnutrition Decreases both Effector and Memory CD4 T cells in Malaria Infection. J. Immunol. 2018;200:52.39. [Google Scholar]
- 139.Nájera O., González C., Toledo G., López L., Ortiz R. Flow cytometry study of lymphocyte subsets in malnourished and well-nourished children with bacterial infections. Clin. Diagn. Lab. Immunol. 2004;11:577–580. doi: 10.1128/CDLI.11.3.577-580.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Savino W., Dardenne M., Velloso L.A., Dayse Silva-Barbosa S. The thymus is a common target in malnutrition and infection. Br. J. Nutr. 2007;98((Suppl. S1)):S11–S16. doi: 10.1017/S0007114507832880. [DOI] [PubMed] [Google Scholar]
- 141.Cunningham-Rundles S., McNeeley D.F., Moon A. Mechanisms of nutrient modulation of the immune response. J. Allergy Clin. Immunol. 2005;115:1119–1128. doi: 10.1016/j.jaci.2005.04.036. quiz 1129. [DOI] [PubMed] [Google Scholar]
- 142.Holzmann H., Hengel H., Tenbusch M., Doerr H.W. Eradication of measles: Remaining challenges. Med. Microbiol. Immunol. 2016;205:201–208. doi: 10.1007/s00430-016-0451-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Guerrant R.L., DeBoer M.D., Moore S.R., Scharf R.J., Lima A.A.M. The impoverished gut--a triple burden of diarrhoea, stunting and chronic disease. Nat. Rev. Gastroenterol. Hepatol. 2013;10:220–229. doi: 10.1038/nrgastro.2012.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Scrimshaw N.S., Taylor C.E., Gordon J.E., World Health Organization . In: Interactions of Nutrition and Infection. Nevin S.S., Carl E.T., John E.G., editors. World Health Organization; Geneva, Switzerland: 1968. Prepared in Consultation with Seventeen Specialists in Various Countries. [PubMed] [Google Scholar]
- 145.Lima A.A.M., Leite Á.M., Di Moura A., Lima N.L., Soares A.M., Abreu C.B., Filho J.Q., Mota R.M.S., Lima I.F.N., Havt A., et al. Determinant Variables, Enteric Pathogen Burden, Gut Function and Immune-related Inflammatory Biomarkers Associated With Childhood Malnutrition: A Prospective Case-Control Study in Northeastern Brazil. Pediatr. Infect. Dis. J. 2017;36:1177–1185. doi: 10.1097/INF.0000000000001569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Raman A.S., Gehrig J.L., Venkatesh S., Chang H.W., Hibberd M.C., Subramanian S., Kang G., Bessong P.O., Lima A.A.M., Kosek M.N., et al. A sparse covarying unit that describes healthy and impaired human gut microbiota development. Science. 2019;365:aau4735. doi: 10.1126/science.aau4735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.McCormick B.J.J., Murray-Kolb L.E., Lee G.O., Schulze K.J., Ross A.C., Bauck A., Lima A.A.M., Maciel B.L.L., Kosek M.N., Seidman J.C., et al. Intestinal permeability and inflammation mediate the association between nutrient density of complementary foods and biochemical measures of micronutrient status in young children: Results from the MAL-ED study. Am. J. Clin. Nutr. 2019;110:1015–1025. doi: 10.1093/ajcn/nqz151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gwela A., Mupere E., Berkley J.A., Lancioni C. Undernutrition, Host Immunity and Vulnerability to Infection Among Young Children. Pediatr. Infect. Dis. J. 2019;38:e175–e177. doi: 10.1097/INF.0000000000002363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Paynter S., Ware R.S., Lucero M.G., Tallo V., Nohynek H., Weinstein P., Williams G., Sly P.D., Simões E.A. Malnutrition: A risk factor for severe respiratory syncytial virus infection and hospitalization. Pediatr. Infect. Dis. J. 2014;33:267–271. doi: 10.1097/INF.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 150.Li T., Zhang Y., Gong C., Wang J., Liu B., Shi L., Duan J. Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur. J. Clin. Nutr. 2020;74:871–875. doi: 10.1038/s41430-020-0642-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bedock D., Bel Lassen P., Mathian A., Moreau P., Couffignal J., Ciangura C., Poitou-Bernert C., Jeannin A.-C., Mosbah H., Fadlallah J., et al. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin. Nutr. ESPEN. 2020;40:214–219. doi: 10.1016/j.clnesp.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Thomas S., Alexander C., Cassady B.A. Nutrition risk prevalence and nutrition care recommendations for hospitalized and critically-ill patients with COVID-19. Clin. Nutr. ESPEN. 2021;44:38–49. doi: 10.1016/j.clnesp.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rouget A., Vardon-Bounes F., Lorber P., Vavasseur A., Marion O., Marcheix B., Lairez O., Balardy L., Fourcade O., Conil J.-M., et al. Prevalence of Malnutrition in COVID-19 Inpatients: The Nutricov Study. Br. J. Nutr. 2021;126:1296–1303. doi: 10.1017/S0007114520005127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Abate S.M., Chekole Y.A., Estifanos M.B., Abate K.H., Kabthymer R.H. Prevalence and outcomes of malnutrition among hospitalized COVID-19 patients: A systematic review and meta-analysis. Clin. Nutr. ESPEN. 2021;43:174–183. doi: 10.1016/j.clnesp.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Yu Y., Ye J., Chen M., Jiang C., Lin W., Lu Y., Ye H., Li Y., Wang Y., Liao Q., et al. Malnutrition Prolongs the Hospitalization of Patients with COVID-19 Infection: A Clinical Epidemiological Analysis. J. Nutr. Health Aging. 2021;25:369–373. doi: 10.1007/s12603-020-1541-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Pironi L., Sasdelli A.S., Ravaioli F., Baracco B., Battaiola C., Bocedi G., Brodosi L., Leoni L., Mari G.A., Musio A. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin. Nutr. 2021;40:1330–1337. doi: 10.1016/j.clnu.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Haraj N.E., El Aziz S., Chadli A., Dafir A., Mjabber A., Aissaoui O., Barrou L., El Kettani El Hamidi C., Nsiri A., Al Harrar R., et al. Nutritional status assessment in patients with Covid-19 after discharge from the intensive care unit. Clin. Nutr. ESPEN. 2021;41:423–428. doi: 10.1016/j.clnesp.2020.09.214. [DOI] [PMC free article] [PubMed] [Google Scholar]