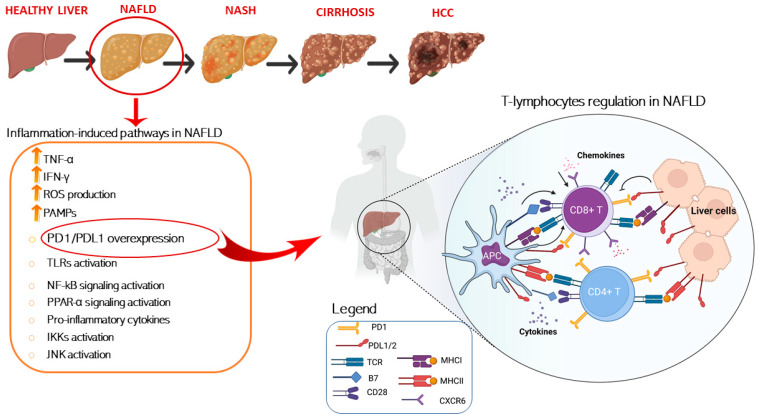
Figure 1.
Schematic representation of T cells immune regulation and inflammation-induced pathways upon liver disease. Liver inflammation is a key factor in NAFLD pathogenesis and is characterized by increased levels of several inflammation associated molecules, such as TNF-α and IFN-γ and inflammation-induced molecular pathways activation. T cell activation requires two signals, the first signal is specific and implies T cell receptor recognition and binding to MHC/antigen presented by an antigen-presenting cell or by tissue specific immunized cells. The second signal is nonspecific and involves the B7 ligand, exposed on the antigen-presenting cells to bind its receptor, CD28, on T cells. On the other hand, T cell are mainly inhibited trough the binding of the exhaustion marker PD-1 which is expressed on cell surface binding to its ligand PD-L1/2 present on APC and over-exposed on liver cell in HCC setting. Conversely, T cell activation is damped by increased levels of immunosuppressive cytokines such as IL-4, IL-8, and IL-10. Instead, IL-5 release induces chemokine receptor CXCR6 upregulation by increasing CD8+ T cells susceptibility to metabolic stimuli and triggering CD8+ auto-aggression of liver tissue. Antigen presenting cells (APCs); programmed cell death protein 1 (PD-1); programmed cell death 1 ligand 1/2 (PD-L1/2); T-cell receptor (TCR); major histocompatibility complexes I/II (MHC I/II); pathogen-associated molecular patterns (PAMPs); Toll-like receptors (TLR); nuclear factor kappa (NF-kB); peroxisome proliferator-activated receptors (PPAR-α); IκB kinases (IKK); c-Jun N-terminal kinases (JNK), tumor necrosis factor alpha (TNF-α), interferon gamma (IFN-γ).