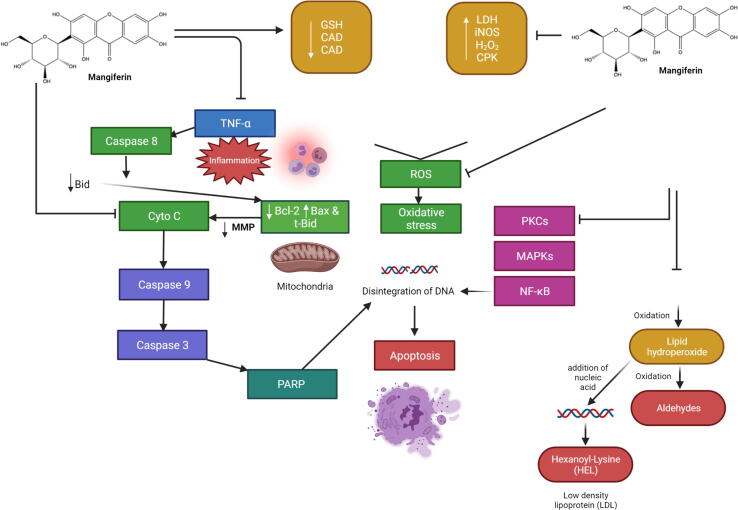
Fig. 3.
Effect of mangiferin in diabetic nephropathy. The pathophysiology of diabetic nephropathy is multifaceted, involving metabolic and hemodynamic alterations, chronic inflammation, activation of the renin-angiotensin system, and oxidative stress. The activation of AGEs, autoxidation of glucose, and xanthine oxidase activity are some of the most likely main sources of ROS production. PKC isoforms, TGF-β1 pathways, and NF-kB were found to be implicated in diabetic nephropathy's oxidative stress-mediated signaling cascades. In the hyperglycemic state, TNF-α was produced, which activated caspase 8, cleaved Bid to tBid, and finally activated the mitochondria-dependent apoptotic pathway. Following hyperglycemia, mangiferin therapy successfully suppressed all of these alterations and preserved the cells from apoptosis. Several novel markers for early disease detection have emerged from the pathologic processes of underlying renal dysfunction and damage. In normoalbuminuric patients with diabetes mellitus type 1, poor glycemic control is an independent predictor of progression to proteinuria (albuminuria). Abbreviations: AGEs, Advanced glycation end products; Bax, Bcl-2-associated X protein; Bcl-2, B-cell lymphoma 2; Bid, BH3-interacting domain death agonist; Cyto C, Cytochrome; cMAPKs, mitogen-activated protein kinases; MMP, Mitochondrial membrane potential; NF-κB, Nuclear factor kappa light chain enhancer of activated B cells; PKC, Protein kinase C; ROS, Reactive oxygen species; tBid, Truncated form of Bid; TGF-1β, Transforming growth factor beta 1; TNF-α, T necrosis factor α.