Abstract
Objectives
To assess the effect of sex differences on short-term and long-term mortality among patients with ST-segment elevation myocardial infarction (STEMI).
Design
Systematic review and meta-analysis of contemporary available evidence.
Setting
PubMed, Embase and Cochrane Library were searched for relevant studies reporting sex-specific outcomes among patients with STEMI published between 1 January 2010 and 1 August 2020. Risk ratios (RRs) and 95% CIs were measured using DerSimonian and Laird random-effects model. Sensitivity analyses were performed and publication bias was also checked. All statistical analyses were performed using STATA V.15.0.
Participants
Studies providing data about short-term or long-term mortality stratified by sex in patients with STEMI were included. Only study conducted in last 10 years were included.
Primary and secondary outcome measures
The primary outcome was all-cause death at short-term (in-hospital or 30 days) and long-term (at least 12 months) follow-up.
Results
A total of 15 studies involving 128 585 patients (31 706 (24.7%) female and 96 879 (75.3%) male) were included. In the unadjusted analyses, female were at a higher risk of short-term mortality (RR, 1.73; 95% CI 1.53 to 1.96, p<0.001, I2=77%) but not long-term mortality (RR, 1.23; 95% CI 0.89 to 1.69, p=0.206, I2=77.5%). When adjusted effect estimates from individual studies were used in meta-analysis, the association between female and higher risk of short-term mortality remained significant (RR, 1.24; 95% CI 1.11 to 1.38, p<0.001, I2=39.6%). And adjusted long-term mortality was also similar between female and male (RR, 1.11; 95% CI 0.42 to 1.80, p=0.670, I2=74.5%).
Conclusions
An increased short-term but not long-term mortality was found in female with STEMI. After adjustment for baseline cardiovascular risk factors and clinical profiles, short-term mortality remains higher in female with STEMI compared with male, indicating the need for further improvements in management in female patients.
Keywords: epidemiology, coronary heart disease, myocardial infarction
Strengths and limitations of this study.
We assessed the contemporary effect of sex differences on mortality among patients with ST-segment elevation myocardial infarction by meta-analysis of studies from the last decade.
A greater number of potentially eligible articles were screened and the large sample size ensures adequate statistical power to detect even a small effect of interest.
Sensitivity analyses by excluding one study at a time and restricting to studies with high quality or with large sample size got consistent results.
Substantial and non-negligible heterogeneity still exist in our meta-analysis and might result in potential bias.
Residual confounding bias could not be totally excluded due to the observational study design of most included studies.
Introduction
Acute myocardial infarction (MI) remains one of leading causes of mortality in both men and women worldwide despite improvement of acute cardiac care.1 Numerous studies have reported that women have a higher risk of in-hospital and long-term adverse outcomes following ST-segment elevation myocardial infarction (STEMI) compared with men.2 Confounders including advanced age and more frequent comorbidities, such as hypertension and diabetes mellitus,3 4 might contribute to excess mortality in women. Moreover, previous studies show lower rates of guideline directed medical therapy and revascularisation are also associated with poorer prognosis for women with STEMI.5
Sex discrepancies in management and outcomes after STEMI have been increasingly reported in the literature and raised public awareness.6 Major progress in therapy for MI and primary and secondary preventive interventions has been made to reduce cardiovascular mortality for women.1 7 And there have been marked reductions in cardiovascular disease mortality in women with acute MI in the past two decades.1 Conflicting results are noted in recent studies on sex differences following STEMI. It is unclear whether the sex differences still exist, in view of substantial improvements in prognosis of cardiovascular disease over the past decade.
In order to assess the contemporary effect of sex differences on short-term and long-term mortality among patients with STEMI, we performed a systematic review and meta-analysis of all available evidence from last decade reporting sex-specific outcomes after STEMI.
Methods
The present systematic review and meta-analysis was performed following the principle of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.8
Literature search
We conducted a comprehensive search of the PubMed, EMBASE and Cochrane Library from 1 January 2010 to 1 August 2020 to identify studies from the last decade that described sex differences in short-term or long-term mortality among patients with STEMI. Both observational studies and randomised clinical trials were eligible. We queried MeSH and the abstract text for the following three search terms: gender part (including “gender”, “female”, “male”, “gender differences”, “sex differences” or “sex characteristics”); outcome part (including “death”, “mortality”, “hospital mortality”, “cardiac death”, “sudden cardiac death”, “all-cause mortality”, “long term mortality”, “one year mortality”, “cardiovascular mortality” or “short term mortality”); MI part (including “myocardial infarction”, “acute myocardial infarction”, “myocardial necrosis”, “ST segment elevation myocardial infarction”, “primary PCI”, “primary percutaneous coronary intervention” or “primary angioplasty”) to identify relevant studies. There was no language restriction or age limit. The full search strategies were presented in online supplemental eTable 1.
bmjopen-2021-053379supp001.pdf (522.8KB, pdf)
Study selection
According to the aim of our analyses, studies were included in this systematic review if data about short-term (in-hospital or 30 days) or long-term (at least 12 months) mortality stratified by sex in patients with STEMI were reported. Two reviewers identified studies eligible for further review by performing an initial screen of titles or abstracts of the search results. Subsequently, a second screen of full texts eligibility was performed by another two reviewers. Studies had to fulfil the following criteria to be included in the present analyses: (i) studies reporting data on all-cause mortality specific to STEMI population; (ii) studies providing enough details to obtain numbers of events or incidence rates according to sex and (iii) enrolment starting not earlier than a decade ago. Editorials, letters, conference proceedings and abstracts were considered to be eligible only if sufficient information was available in abstracts or associated tables or figures. We excluded studies if they were review articles or case reports, or if they involved pregnant participants, critically ill patients or provided insufficient data to allow for risk estimates to be calculated. Any disagreement was reviewed by a third reviewer and resolved by consensus.
Data extraction
Detailed data from selected studies were extracted independently by two reviewers using a standardised form independently. Data about study and participants’ characteristics, including year of study, sample size, time of enrolment, geographical location, endpoints of study and follow-up duration were collected. Any discrepancies were reviewed by a third reviewer and resolved by consensus. The quality of included studies was evaluated by Newcastle-Ottawa scale using prespecified items comprised patients’ selection (representativeness and selection of patients, ascertainment of exposure), comparability of cohorts based on design or analysis, and outcome (assessment of outcomes, adequacy of follow-up).9 A quality score (0–9 points) was generated according to a maximum of 1 point for each item.
Patient and public involvement
Due to the nature of the systematic review and meta-analysis, this study did not involve patients and the public in the design, or conduct, or reporting or dissemination plans.
Statistical analysis
The risk ratios (RRs) and 95% CIs were primarily used to represent the effect of sex differences on mortality after STEMI. And data were combined using random-effects model of DerSimonian and Laird with inverse variance weighting. Random-effect model was used due to substantial clinical and statistical heterogeneity. Following analyses were performed: (i) unadjusted RRs for short-term and long-term all-cause mortality using raw number of death and total participants at risk for death specific to each sex, (ii) adjusted RRs for short-term and long-term all-cause mortality using adjusted RRs if they were described in those included studies. In terms of short-term mortality, the RRs for in-hospital and 30-day mortality were also calculated, respectively.
We assess heterogeneity across studies with Cochran’s Q-test and I2-test, with p<0.1 or I2>50% considered significant. We also performed meta-regression to identify the potential sources of heterogeneity in the included studies. The potential sources were differences in diabetes, hypertension, hyperlipidaemia, smoking, prior MI and prior percutaneous coronary intervention (PCI). Furthermore, stratified analysis was conducted as well by dividing the included studies into different subgroups based on the Newcastle-Ottawa scale scores (>7 points or ≤7 points) to assess the potential sources of heterogeneity. To assess the potential effect of publication bias, we inspected funnel plots for asymmetry and used Egger’s regression asymmetry test in which p<0.05 was considered to indicate significant publication bias.
Sensitivity analyses were conducted by excluding one study at a time and comparing the results with the complete one. In addition, we also performed sensitivity analyses by restricting to high-quality studies with a Newcastle-Ottawa scale of 5 points or more and restricting to studies with sample size bigger than 1000 participants. All statistical analyses were performed using STATA V.15.0 (Stata Corp). Differences were considered statistically significant at p<0.05 (two-sided).
Results
Literature search
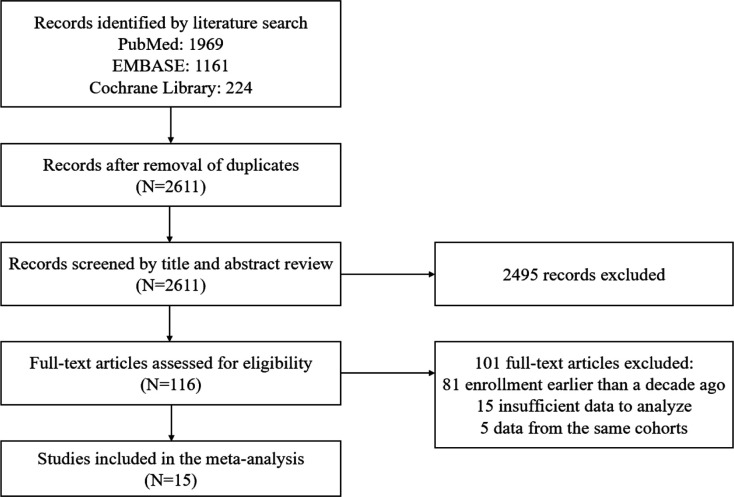
Study selection details were outlined in figure 1. The literature search identified 2611 potentially relevant articles. After screening based on title and abstract review, 2495 records were excluded. A total of 116 full-text were finally assessed for eligibility, with 96 papers excluded due to enrolment starting earlier than a decade ago or no sufficient gender-specific data to analyse. Another five papers reviewed in detail were excluded after due to data from the same cohorts. A total of 15 studies were finally included in the present systematic review and meta-analysis.10–24
Figure 1.
Flowchart of selection of studies included in meta-analysis.
Study characteristics
Of the 15 included studies, 8 were multicentre studies and 4 studies enrolled more than 10 000 patients with STEMI (see table 1 for further information on included studies). Baseline characteristics of participants were missing in some included studies, but all included studies provided sufficient data for analysis of sex differences in clinical outcomes. Except for 1 study, which was a prespecified gender analysis of randomised controlled trial, the remaining 14 were observational studies. Among the 10 included studies which reported adjusted analyses, most studied adjusted for age, diabetes mellitus, hypertension and prior MI/PCI, while some adjusted for renal insufficiency, cardiogenic shock, cardiac arrest at admission and occurrence time of symptom onset. Variables that were adjusted in the adjusted analyses from the included studies were presented in online supplemental eTable 2. Results of assessment of study quality using Newcastle-Ottawa scale were shown in online supplemental eTable 3.
Table 1.
Characteristics of included studies
| Author(s) | Year | Region | Study design | Data source | Multicentre | Time of enrolment | Patients with STEMI (n) | Female | Endpoint | Follow-up |
| Venetsanos et al10 | 2017 | 13 countries | Prospective | Clinical registry | Yes | September 2011–October 2013 | 1862 | 369 (20.0) | Major adverse cardiovascular events and definite stent thrombosis | 30 days |
| Ali et al11 | 2018 | Germany | Prospective | Administrative database | No | 2013–2017 | 312 | 101 (32.4) | All-cause in-hospital mortality | NA |
| Langabeer et al12 | 2018 | USA | Prospective | Clinical registry | Yes | January 2010-December 2015 | 9674 | 2569 (26.6) | In-hospital mortality | NA |
| Tang et al13 | 2018 | China | Prospective | Administrative database | No | January 2013–December 2013 | 1238 | 210 (1.9) | Major adverse cardiac and cerebrovascular events | 730±30 days |
| Cenko et al14 | 2019 | 12 European countries | Prospective | Clinical registry | Yes | January 2010–July 2018 | 10 443 | 3112 (29.8) | 30-day all-cause mortality | 30 days |
| Hao et al15 | 2019 | China | Prospective | Clinical registry | Yes | November 2014–June 2018 | 50 203 | 11 016 (21,9) | In-hospital mortality | NA |
| Hannan et al16 | 2019 | USA | Retrospective | Administrative database | Yes | January 2013–December 2015 | 23 809 | 7791 (32.7) | In-hospital/30-day mortality | 30 days |
| Maznyczka et al17 | 2019 | UK | Retrospective | Clinical registry | No | July 2011–November 2012 | 324 | 87 (26.9) | All-cause death/first heart failure hospitalisation | 5 years |
| Stehli et al18 | 2019 | Australia | Prospective | Clinical registry | Yes | 2013–2016 | 6431 | 1317 (20.5) | In-hospital/30-day major adverse events, and major bleeding | 30 days |
| Burgess et al19 | 2020 | Australia | Prospective | Administrative database | No | December 2010–April 2014 | 589 | 123 (21) | Cardiac death and myocardial infarction | 2 years |
| Dharma et al20 | 2020 | Indonesia | Retrospective | Administrative database | No | February 2011-August 2019 | 6557 | 929 (14.2) | All-cause mortality | 30 days and 1 year |
| Kerkman et al21 | 2020 | Netherlands | Retrospective | Administrative database | Yes | 2015–2016 | 787 | 229 (29) | All-cause mortality | 1 year |
| Siabani et al22 | 2020 | Iran | Prospective | Clinical registry | No | June 2016–May 2018 | 1484 | 311(21) | In-hospital mortality | NA |
| Tai et al23 | 2020 | China | Retrospective | Administrative database | No | January 2013–December 2017 | 182 | 56 (30.8) | In-hospital/1-year mortality | 1 year |
| Tizón-Marcos et al24 | 2020 | Spain | Prospective | Clinical registry | Yes | 2010–2016 | 14 690 | 3486 (23.7) | 30-day/1-year all-cause mortality | 1 year |
STEMI, ST-segment elevation myocardial infarction.
Patient characteristics
A total of 128 585 patients with STEMI (31 706 (24.7%) female and 96 879 (75.3%) male) were involved in the 15 included studies. Female tended to be older and had higher prevalence of diabetes mellitus in all included studies. And in most studies, other important comorbidities, including hypertension and hyperlipidaemia, were more frequent in female. Greater proportions of male were smokers and had prior PCI or MI. Besides, some studies reported that door-to-balloon time and symptom onset to balloon time were longer in female than male. Part of patient baseline characteristics were summarised in table 2.
Table 2.
Baseline characteristics of participants in included studies
| Authors | Year | Age, mean (SD), years | Diabetes, n (%) | Hypertension, n (%) | Hyperlipidaemia, n (%) | Smoking, n (%) | Prior MI, n (%) | Prior PCI, n (%) | |||||||
| Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | ||
| Venetsanos et al10 | 2017 | 69 (13.0) | 59 (11.0) | 48 (13.0) | 205 (13.7) | 190 (51.5) | 605 (40.5) | 117 (31.7) | 536 (35.9) | NA | NA | 24 (6.5) | 135 (9.0) | 16 (4.3) | 124 (8.3) |
| Ali et al11 | 2018 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Langabeer et al12 | 2018 | 62.5 (13.6) | 60.2 (12.5) | 759 (29.6) | 1975 (27.8) | NA | NA | 1265 (49.3) | 3693 (52.0) | 951 (37.0) | 2763 (38.9) | 435 (16.9) | 1304 (18.4) | NA | NA |
| Tang et al13 | 2018 | 64.5 (9.3) | 54.4 (10.7) | 66 (31.4) | 311 (25.1) | 141 (67.1) | 659 (53.3) | 125 (59.5) | 749 (60.3) | 33 (15.7) | 957 (77.3) | 10 (4.8) | 83 (6.7) | 60 (28.6) | 282 (22.8) |
| Cenko et al14 | 2019 | 66.1 (11.7) | 59.7 (11.7) | 925 (29.7) | 1531 (20.9) | 2322 (74.6) | 4502 (61.4) | 1353 (43.3) | 3100 (42.3) | 1010 (32.5) | 3714 (50.7) | 301 (9.7) | 842 (11.5) | 306 (9.8) | 762 (10.4) |
| Hao et al15 | 2019 | 69.0 (10.6) | 61.1 (12.4) | 10 141 (48.1) | 24 082 (39.4) | 15 607 (74.1) | 38 426 (62.9) | 17 996 (85.4) | 50 944 (83.3) | 1719 (8.2) | 32 377 (53.0) | NA | NA | NA | NA |
| Hannan et al16 | 2019 | 70.72 (14.73) | 62.11 (12.82) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 868 (11.1) | 2206 (13.8) |
| Maznyczka et al17 | 2019 | 61.2 (12.2) | 58.6 (11.2) | 8 (9.2) | 26 (11.0) | 32 (36.8) | 73 (30.8) | 28 (32.2) | 66 (27.8) | 57 (65.5) | 139 (58.6) | 5 (5.7) | 20 (8.4) | 2 (2.3) | 16 (6.8) |
| Stehli et al18 | 2019 | 66.5 (13.2) | 60.8 (12.2) | 245 (18.6) | 770 (15.1) | NA | NA | NA | NA | NA | NA | NA | NA | 104 (7.9) | 577 (11.3) |
| Burgess et al19 | 2020 | 62.7 (52.7–73.2) | 58.2 (50.6–65.7) | 39 (31.7) | 88 (18.9) | 84 (68.3) | 243 (52.1) | 83 (67.5) | 253 (52.3) | 64 (52.0) | 252 (54.1) | 9 (7.3) | 41 (8.8) | NA | NA |
| Dharma et al20 | 2020 | 60 (10) | 55 (10) | 403 (43.4) | 1548 (27.5) | 647 (69.6) | 2889 (51.3) | 299 (32.2) | 1779 (31.6) | 109 (11.7) | 4049 (71.9) | NA | NA | NA | NA |
| Kerkman et al21 | 2020 | 68 (14) | 61 (12) | 39 (17.6) | 66 (12.5) | 101 (45.7) | 178 (33.6) | 56 (25.9) | 110 (21.0) | 88 (41.1) | 258 (49.3) | 30 (13.6) | 79 (13.7) | 33 (14.4) | 77 (14.2) |
| Siabani et al22 | 2020 | 65.8 (11.3) | 59.0 (12.4) | 114 (37.7) | 187 (16.2) | 195 (63.7) | 410 (35.4) | 110 (36.7) | 208 (18.5) | 41 (13.2) | 655 (55.9) | NA | NA | NA | NA |
| Tai et al23 | 2020 | 78 (76–81) | 78 (76–80) | 96 (35.2) | 116 (26.5) | 217 (79.5) | 319 (72.8) | NA | NA | 14 (5.4) | 239 (56.5) | NA | NA | 36 (13.5) | 78 (18.1) |
| Tizón-Marcos et al24 | 2020 | 69.9 (13.7) | 60.9 (12.6) | 844 (24.2) | 1927 (17.2) | 1192 (34.2) | 2722 (24.3) | 878 (25.2) | 2375 (21.2) | 474 (13.6) | 2711 (24.2) | NA | NA | NA | NA |
MI, myocardial infarction; PCI, percutaneous coronary intervention.
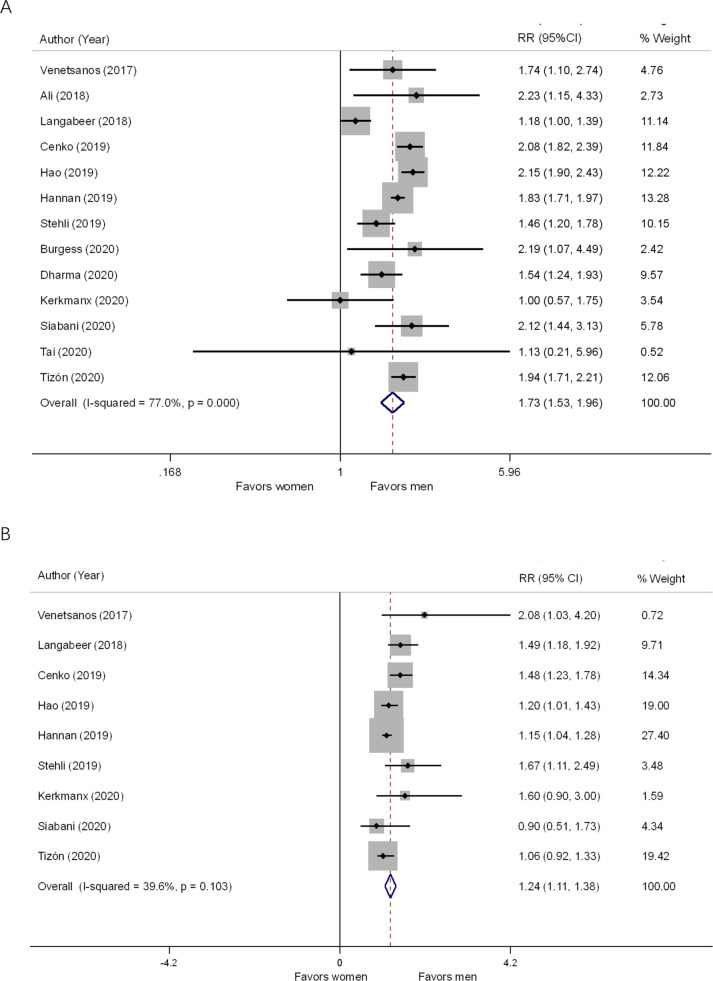
Short-term all-cause mortality
Thirteen studies reported sex-specific unadjusted short-term mortality (seven studies with 30-day mortality and six studies with in-hospital mortality) of patients with STEMI. There were 2873 of 31 409 (9.1%) cases of all-cause mortality in female compared with 4380 of 95 610 (4.6%) in male. Female were at a significantly higher risk of short-term mortality (RR, 1.73; 95% CI 1.53 to 1.96, p<0.001, I2=77%) compared with male (figure 2A). Nine studies involving 119 379 patients reported adjusted short-term mortality specific to sex. In adjusted analysis, the association between female and higher risk of short-term mortality remained significant (RR, 1.24; 95% CI 1.11 to 1.38, p<0.001, I2=39.6%) (figure 2B). However, the strength of association calculated with adjusted RRs from these nine studies was attenuated.
Figure 2.
Forest plots of relative risks of short-term all-cause mortality among women and men with ST-segment elevation myocardial infarction. Forest plots showing unadjusted (A) and adjusted (B) short-term all-cause mortality of women compared with men with ST-segment elevation myocardial infarction using random-effects model. RR, risk ratio.
Subgroup analysis demonstrated that the results of studies with Newcastle-Ottawa scale >7 points (RR, 1.90; 95% CI 1.73 to 2.09, p=0.018, I2=63.4%) and studies with ≤7 points (RR, 1.52; 95% CI 1.20 to 1.93, p=0.026, I2=58.1%) were consistent in unadjusted short-term mortality (see online supplemental eFigure 1). The impact of sex on in-hospital (RR, 1.71; 95% CI 1.27 to 2.31, p<0.001, I2=86.4%) and 30-day mortality (RR, 1.81; 95% CI 1.62 to 2.02, p<0.001, I2=56.6%) were consistent. The meta-analysis performed in studies of patients undergoing PCI for STEMI also showed increased unadjusted mortality (RR, 1.45; 95% CI 1.05 to 2.00, p=0.026, I2=39.5%) in female patients.
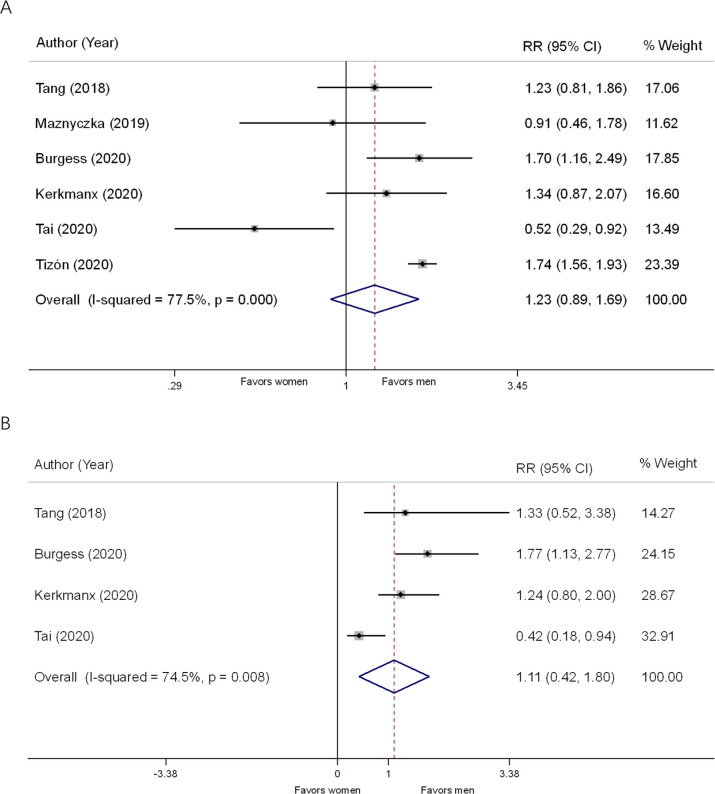
Long-term all-cause mortality
Six studies involved 18 018 patients with STEMI (4191 female and 13 827 male) and followed up for more than 1 year, and reported all-cause mortality for female and male. The incidence of long-term all-cause mortality was 13.9% (n=584) in female and 8.7% (n=1202) in male. In unadjusted analysis, no significant sex difference was found in long-term mortality (RR, 1.23; 95% CI 0.89 to 1.69, p=0.206, I2=77.5%) (figure 3A). The unadjusted long-term mortality was also similar between female and male patients undergoing PCI (RR, 1.28; 95% CI 0.95 to 1.73, p=0.108, I2=0.0%). And the adjusted analysis of the pooled results from four studies, also showed a similar risk of mortality at long-term follow-up in female compared with male (RR, 1.11; 95% CI 0.42 to 1.80, p=0.670, I2=74.5%) (figure 3B).
Figure 3.
Forest plots of relative risks of long-term all-cause mortality among women and men with ST-segment elevation myocardial infarction. Forest plots showing unadjusted (A) and adjusted (B) long-term all-cause mortality of women compared with men with ST-segment elevation myocardial infarction using random-effects model. RR, risk ratio.
Meta-regression analysis, sensitivity analyses and publication bias
According to meta-regression analysis, differences in prevalence of diabetes (β coefficient, 0.248; p=0.337; adjusted R2=1.31%; I2=80.86%; τ2=0.044), hypertension (β coefficient, −0.255; p=0.538; adjusted R2=24.22%; I2=41.04%; τ2=0.008), hyperlipidaemia (β coefficient, 0.260; p=0.415; adjusted R2=−1.84%; I2=83.59%; τ2=0.050), smoking (β coefficient, −0.040; p=0.255; adjusted R2=17.86%; I2=79.41%; τ2=0.045), prior MI (β coefficient, −2.725; p=0.126; adjusted R2=60.30%; I2=60.19%; τ2=0.032) and prior PCI (β coefficient, 0.109; p=0.896; adjusted R2=−58.31%; I2=61.73%; τ2=0.042) between sexes were not identified as significant sources of heterogeneity for short-term all-cause mortality. Given that not all included study provided information on confounders stratified by sex, the results of meta-regression analyses should be interpreted with caution.
Sensitivity analysis by excluding one study at a time (see online supplemental eFigure 2) or restricted to data from studies with sample size bigger than 1000 (RR, 1.75; 95% CI 1.54 to 1.99, p<0.001, I2=82.9%) both indicated that none of the studies affected the results of short-term mortality in this meta-analysis significantly. In analysis for long-term mortality, sensitivity analysis showed a possibly higher influence on the result attribute to the study of Tai et al (see online supplemental eFigure 3). After removing this study from meta-analysis, the association of female with increased long-term mortality became significant (RR, 1.50; 95% CI 1.23 to 1.83, p<0.001, I2=40.9%). We found no evidence of publication bias across studies based on visual inspection of funnel plots (see online supplemental eFigure 4) and the results from Egger’s tests for short-term mortality (p=0.462) and for long-term mortality (p=0.053).
Discussion
Our systematic review and meta-analysis of contemporary literature on sex differences among patients with STEMI demonstrate that female have a higher risk of short-term but not long-term mortality compared with male with STEMI. Furthermore, after adjustment for baseline cardiovascular risk factors and clinical profiles, the sex differences in short-term mortality are attenuated but remain significant, while female have the similar long-term mortality with male.
Our results are somewhat in accordance with several previously published meta-analysis.2 25 A considerable number of studies have consistently suggested that women were at a higher risk of short-term mortality after acute coronary syndrome (ACS). However, whether risk of long-term mortality is also higher in women with ACS remains under debate. Some studies indicated that women with STEMI had a higher 1-year rate of death compared with men,26 while the 1-year mortality rate was conversely lower in women than men in some other studies.23 24 In our study, with respect to short-term mortality, the analyses of studies with high or low quality, and big or small sample size yielded similar results. However, in terms of long-term mortality, caution is needed when interpreting our finding of non-significant increased long-term mortality in adjusted analyses, due to the results of sensitivity analysis which showed a significant association between female and increased long-term mortality after removing one study from adjusted analyses.
It is widely accepted that there are significant differences in outcomes of women and men with acute MI. In our study, after adjusted for participants’ baseline cardiovascular risk factors and clinical profiles, the strength of association between gender and short-term mortality was substantially attenuated, which suggested that poorer baseline cardiovascular risk profile partially explained the impact of sex differences on mortality. Multiple studies have shown that women with STEMI present at older age and have a higher burden of comorbidities, contributing to the sex differences in mortality after STEMI.27 All studies included in our meta-analysis demonstrate that female patients are older and with more diabetes mellitus as well as hypertension. In addition, some sex-specific studies found that certain risk factors and comorbidities were more potent in women.28 Diabetes mellitus, hypertension and smoking status are more strongly associated with increased risk of cardiac events in women compared with men.27 29
Notably, that these differences mentioned above still could not completely explain the gap in mortality between sexes. It has been proved that women with acute MI were less likely to be treated with guideline directed medical therapy and less likely to receive primary reperfusion therapy including primary PCI or fibrinolysis.30 Regarding medical therapy, numerous studies conducted around the world consistently demonstrate female survivors are receiving less optimal medical therapy after acute MI during hospitalisation or at discharge.31 32 Though there might be no differences in treatment adherence between men and women, some studies report significant sex disparities in initiation of appropriate pharmacotherapy after MI.33 Results from these observational studies have shown women are receiving less optimal medical therapy including aspirin, statins and ACE inhibitors in all age groups, especially young women, and suggested that clinicians and patients may benefit from better education and awareness of undertreatment of younger women.33 34
Lower rates of revascularisation are observed among women with STEMI compared with men in several studies despite proven benefit of this therapy.35 Moreover, the sex differences might be driven by delays in presentation to hospital and women with STEMI were more likely to experience longer delays than men. Although a great improvement in emergency medical services and timely revascularisation over the past decades, recent studies show that women with STEMI still present later and have a longer ischaemic time than men. Previous studies have shown consistently that women have longer door-to-balloon times and longer door-to-needle times.36 37 In addition, women are also more likely to exhibit longer prehospital delays in seeking medical care after the development of symptoms suggestive of MI. Although there have been significant reductions in patient and system delay in the last decade, women continue to have longer presentation and treatment times.38 Sex differences also exist in clinical presentation of STEMI. Although chest pain was the most common ACS symptom in both sexes, women were more likely to present without chest pain than men.39 40 Lower rates of typical chest pain reported among women with STEMI may also influence provider decision-making to pursue less aggressive care including invasive revascularisation.
Some included studies of our meta-analysis enrolled patients with STEMI in general,14–16 while some others enrolled patients undergoing PCI for STEMI.11 13 18 The different prognosis of patients receiving reperfusion therapy or no-reperfusion therapy might be a potential source of heterogeneity of our study. Nevertheless, our results are completely consistent with a previous meta-analysis from Pancholy et al, which investigated sex differences in mortality among patients with STEMI treated with primary PCI.2 Its results demonstrated that, when adjusted RRs were used, the increased risk for 1-year mortality in women was no longer significant and the risk of in-hospital mortality still significantly elevated. It should be noted that more than 50% of patients were treated with PCI in the most study conducted among the general patients with STEMI and included by our analysis, even more than 90% in some included studies.12 24 The increasing rate of primary PCI in recent years might be a reason for the consistency of our findings and previous studies conducted specifically among patients with STEMI undergoing PCI.
Complications including bleeding, heart failure and mechanical complications are more likely to develop in women with acute MI and increase the risk of mortality.14 41 42 Bleeding secondary to antithrombotic therapies and invasive procedures is more frequent in women.43 Three included studies reported incidence of bleeding following STEMI and they all found that women were at higher risk of bleeding.10 13 18 One study included in our analysis examined the relationships among sex, acute heart failure, and related outcomes after STEMI.14 Its results demonstrate that women are at higher risk to develop de novo heart failure after STEMI and women with de novo heart failure have worse survival compared with men. However, we could not compare the incidence of these complications due to the lack of sufficient data. Mechanical complications requiring surgical intervention are also much more common in women after acute MI and associated with high mortality rates.44
Several limitations of this meta-analysis should be considered. First, the included studies are all observational studies except one post hoc analysis of randomised controlled trial. Hence, there may be residual confounding bias inherent in the observational study design in our meta-analysis. Second, in adjusted analysis, not all included studies adjusted for the same confounders and not all studies reported adjusted RRs. The confounders which were adjusted in the included studies might differ greatly across studies. Third, there was substantial heterogeneity in our meta-analysis, which could partly be attributed to the wide variability in the sample sizes, locations and treatment regimens across included studies. Additionally, although we calculated adjusted RRs for all-cause mortality, it needed to be noted that relevant confounders might have differed across studies. Fourth, the analysis of long-term mortality, especially the adjusted analysis, included far fewer studies compared with analysis of short-term mortality. Hence, there might be significant bias in the results about long-term mortality.
In conclusion, our meta-analysis, pooling data from contemporary literature, shows that women with STEMI have a higher risk of short-term mortality but not long-term mortality. The effect of sex differences on mortality in patients with STEMI remain significant after adjustment for baseline cardiovascular risk factors and clinical profiles, suggesting that public awareness of increased risk and further improvements in management in women with STEMI are necessary.
Supplementary Material
Footnotes
Contributors: ZX: study concepts, study design, literature research, statistical analysis, manuscript preparation, manuscript editing. TG and YW: data acquisition, data analysis/interpretation. JL, YL, JZ and RG: manuscript revision/review. HQ: manuscript final version approval. ZX and HQ are the guarantors. All authors approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke Statistics-2020 update: a report from the American heart association. Circulation 2020;141:e139–596. 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 2.Pancholy SB, Shantha GPS, Patel T, et al. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis. JAMA Intern Med 2014;174:1822–30. 10.1001/jamainternmed.2014.4762 [DOI] [PubMed] [Google Scholar]
- 3.Wenger NK, Arnold A, Bairey Merz CN, et al. Hypertension Across a Woman's Life Cycle. J Am Coll Cardiol 2018;71:1797–813. 10.1016/j.jacc.2018.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters SAE, Woodward M. Sex differences in the burden and complications of diabetes. Curr Diab Rep 2018;18:33. 10.1007/s11892-018-1005-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huded CP, Johnson M, Kravitz K, et al. 4-Step Protocol for Disparities in STEMI Care and Outcomes in Women. J Am Coll Cardiol 2018;71:2122–32. 10.1016/j.jacc.2018.02.039 [DOI] [PubMed] [Google Scholar]
- 6.Mehta LS, Beckie TM, DeVon HA, et al. Acute myocardial infarction in women: a scientific statement from the American heart association. Circulation 2016;133:916–47. 10.1161/CIR.0000000000000351 [DOI] [PubMed] [Google Scholar]
- 7.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet 2017;389:197–210. 10.1016/S0140-6736(16)30677-8 [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 10.Venetsanos D, Sederholm Lawesson S, Alfredsson J, et al. Association between gender and short-term outcome in patients with ST elevation myocardial infraction participating in the International, prospective, randomised administration of ticagrelor in the catheterisation laboratory or in the ambulance for new ST elevation myocardial infarction to open the coronary artery (Atlantic) trial: a prespecified analysis. BMJ Open 2017;7:e015241. 10.1136/bmjopen-2016-015241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali M, Lange SA, Wittlinger T, et al. In-Hospital mortality after acute STEMI in patients undergoing primary PCI. Herz 2018;43:741–5. 10.1007/s00059-017-4621-y [DOI] [PubMed] [Google Scholar]
- 12.Langabeer JR, Henry TD, Fowler R, et al. Sex-Based differences in discharge disposition and outcomes for ST-segment elevation myocardial infarction patients within a regional network. J Womens Health 2018;27:1001–6. 10.1089/jwh.2017.6553 [DOI] [PubMed] [Google Scholar]
- 13.Tang X-F, Song Y, Xu J-J, et al. Effect of sex difference in clinical presentation (stable coronary artery disease vs unstable angina pectoris or non-ST-elevation myocardial infarction vs ST-elevation myocardial infarction) on 2-year outcomes in patients undergoing percutaneous coronary. J Interv Cardiol 2018;31:5–14. 10.1111/joic.12451 [DOI] [PubMed] [Google Scholar]
- 14.Cenko E, van der Schaar M, Yoon J, et al. Sex-Related Differences in Heart Failure After ST-Segment Elevation Myocardial Infarction. J Am Coll Cardiol 2019;74:2379–89. 10.1016/j.jacc.2019.08.1047 [DOI] [PubMed] [Google Scholar]
- 15.Hao Y, Liu J, Liu J, et al. Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome. Circulation 2019;139:1776–85. 10.1161/CIRCULATIONAHA.118.037655 [DOI] [PubMed] [Google Scholar]
- 16.Hannan EL, Wu Y, Tamis-Holland J, et al. Sex differences in the treatment and outcomes of patients hospitalized with ST-elevation myocardial infarction. Catheter Cardiovasc Interv 2020;95:196–204. 10.1002/ccd.28286 [DOI] [PubMed] [Google Scholar]
- 17.Maznyczka AM, Carrick D, Carberry J, et al. Sex-based associations with microvascular injury and outcomes after ST-segment elevation myocardial infarction. Open Heart 2019;6:e000979. 10.1136/openhrt-2018-000979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stehli J, Martin C, Brennan A, et al. Sex differences persist in time to presentation, revascularization, and mortality in myocardial infarction treated with percutaneous coronary intervention. J Am Heart Assoc 2019;8:e012161. 10.1161/JAHA.119.012161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burgess SN, Juergens CP, Nguyen TL, et al. Comparison of late cardiac death and myocardial infarction rates in women vs men with ST-elevation myocardial infarction. Am J Cardiol 2020;128:120–6. 10.1016/j.amjcard.2020.04.044 [DOI] [PubMed] [Google Scholar]
- 20.Dharma S, Dakota I, Andriantoro H, et al. Association of gender with clinical outcomes of patients with acute ST-segment elevation myocardial infarction presenting with acute heart failure. Coron Artery Dis 2021;32:17–24. 10.1097/MCA.0000000000000892 [DOI] [PubMed] [Google Scholar]
- 21.Kerkman T, Ten Brinke LBG, Huybrechts B, et al. Evaluation of sex differences in patients with ST-elevated myocardial infarction: an observational cohort study in Amsterdam and surrounding region. Neth Heart J 2020;28:595–603. 10.1007/s12471-020-01435-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siabani S, Davidson PM, Babakhani M, et al. Gender-Based difference in early mortality among patients with ST-segment elevation myocardial infarction: insights from Kermanshah STEMI registry. J Cardiovasc Thorac Res 2020;12:63–8. 10.34172/jcvtr.2020.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tai S, Li X, Yang H, et al. Sex differences in the outcomes of elderly patients with acute coronary syndrome. Cardiol Res Pract 2020;2020:1–8. 10.1155/2020/5091490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tizón-Marcos H, Vaquerizo B, Marrugat J, et al. Differences in 30-day complications and 1-year mortality by sex in patients with a first STEMI managed by the Codi IAM network between 2010 and 2016. Rev Esp Cardiol 2021;74:674–81. 10.1016/j.rec.2020.06.002 [DOI] [PubMed] [Google Scholar]
- 25.Bavishi C, Bangalore S, Patel D, et al. Short and long-term mortality in women and men undergoing primary angioplasty: a comprehensive meta-analysis. Int J Cardiol 2015;198:123–30. 10.1016/j.ijcard.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 26.Kosmidou I, Redfors B, Selker HP, et al. Infarct size, left ventricular function, and prognosis in women compared to men after primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: results from an individual patient-level pooled analysis of 10 randomized trials. Eur Heart J 2017;38:1656–63. 10.1093/eurheartj/ehx159 [DOI] [PubMed] [Google Scholar]
- 27.Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ 2018;363:k4247. 10.1136/bmj.k4247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 29.Harreiter J, Fadl H, Kautzky-Willer A, et al. Do women with diabetes need more intensive action for cardiovascular reduction than men with diabetes? Curr Diab Rep 2020;20:61. 10.1007/s11892-020-01348-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation 2019;139:1047–56. 10.1161/CIRCULATIONAHA.118.037137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao M, Woodward M, Vaartjes I, et al. Sex Differences in Cardiovascular Medication Prescription in Primary Care: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2020;9:e014742. 10.1161/JAHA.119.014742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eindhoven DC, Hilt AD, Zwaan TC, et al. Age and gender differences in medical adherence after myocardial infarction: Women do not receive optimal treatment - The Netherlands claims database. Eur J Prev Cardiol 2018;25:181–9. 10.1177/2047487317744363 [DOI] [PubMed] [Google Scholar]
- 33.Smolina K, Ball L, Humphries KH, et al. Sex disparities in post-acute myocardial infarction pharmacologic treatment initiation and adherence: problem for young women. Circ Cardiovasc Qual Outcomes 2015;8:586–92. 10.1161/CIRCOUTCOMES.115.001987 [DOI] [PubMed] [Google Scholar]
- 34.Nguyen HL, Goldberg RJ, Gore JM, et al. Age and sex differences, and changing trends, in the use of evidence-based therapies in acute coronary syndromes: perspectives from a multinational registry. Coron Artery Dis 2010;21:336–44. 10.1097/MCA.0b013e32833ce07c [DOI] [PubMed] [Google Scholar]
- 35.Pelletier R, Humphries KH, Shimony A, et al. Sex-Related differences in access to care among patients with premature acute coronary syndrome. CMAJ 2014;186:497–504. 10.1503/cmaj.131450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy AC, Yudi MB, Farouque O, et al. Impact of gender and door-to-balloon times on long-term mortality in patients presenting with ST-elevation myocardial infarction. Am J Cardiol 2019;124:833–41. 10.1016/j.amjcard.2019.06.008 [DOI] [PubMed] [Google Scholar]
- 37.D'Onofrio G, Safdar B, Lichtman JH, et al. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation 2015;131:1324–32. 10.1161/CIRCULATIONAHA.114.012293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bugiardini R, Ricci B, Cenko E, et al. Delayed care and mortality among women and men with myocardial infarction. J Am Heart Assoc 2017;6:e005968. 10.1161/JAHA.117.005968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan NA, Daskalopoulou SS, Karp I, et al. Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern Med 2013;173:1863–71. 10.1001/jamainternmed.2013.10149 [DOI] [PubMed] [Google Scholar]
- 40.Canto JG, Rogers WJ, Goldberg RJ, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012;307:813–22. 10.1001/jama.2012.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moscucci M, Fox KAA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the global registry of acute coronary events (grace). Eur Heart J 2003;24:1815–23. 10.1016/S0195-668X(03)00485-8 [DOI] [PubMed] [Google Scholar]
- 42.Kolte D, Khera S, Aronow WS, et al. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc 2014;3:e000590. 10.1161/JAHA.113.000590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nanna MG, Hajduk AM, Krumholz HM, et al. Sex-Based differences in presentation, treatment, and complications among older adults hospitalized for acute myocardial infarction: the SILVER-AMI study. Circ Cardiovasc Qual Outcomes 2019;12:e005691. 10.1161/CIRCOUTCOMES.119.005691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elbadawi A, Elgendy IY, Mahmoud K, et al. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction. JACC Cardiovasc Interv 2019;12:1825–36. 10.1016/j.jcin.2019.04.039 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053379supp001.pdf (522.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article.