Abstract
Objective:
To test the hypothesis that there is no difference in the accuracy of bracket placement produced by OrthoCAD iQ indirect bonding (IDB) and that of an in-house fabricated IDB system by measuring the quality of intra-arch dental alignment at the end of simulated orthodontic treatment.
Materials and Methods:
Twenty-eight artificial teeth were arranged to resemble a typical preorthodontic malocclusion. Forty-six sets of models were duplicated from the original malocclusion and randomly divided into two sample groups. Half of the models had their bracket positions selected by OrthoCAD, while the others were completed by a combination of faculty and residents in a university orthodontic department. Indirect bonding trays were fabricated for each sample and the brackets were transferred back to the original malocclusion following typical bonding protocol. The individual teeth were ligated on a .021 × .025-inch stainless steel archwire to simulate their posttreatment positions. The two sample groups were compared using the objective grading system (OGS) originally designed by the American Board of Orthodontics.
Results:
The mean total OGS score for the OrthoCAD sample group was 39.25 points, while the traditional IDB technique scored 41.00 points. No statistical difference was found between total scores or any of the four components evaluated. Similar ranges of scores were observed, with the OrthoCAD group scoring from 30 to 52 points and the traditional IDB group scoring from 33 to 53 points.
Conclusions:
The hypothesis is not accepted. OrthoCAD iQ does not currently offer a system that can position orthodontic brackets better or more reliably than traditional indirect bonding techniques.
Keywords: 3D models, Diagnostic, Indirect bonding, Orthodontics
INTRODUCTION
The process of integrating computers into orthodontics began a long time ago. As technology has developed and improved, the specialty has seen a growing dependence on the use of computers. Practice management software, radiographs, and diagnostic models are all transitioning to a completely digital format. Every day seems to bring an innovation, and companies are scrambling to find the next big breakthrough.
Thus, it is logical that technologic advances would find their way into a part of orthodontics wrought with human error, and yet critical to both treatment timing and results. With preadjusted orthodontic appliances, appropriate bracket placement is the single most important step. When positioned correctly, tooth movement can be swift and predictable. If misplaced, however, errors in first, second, and third order expression are unavoidable.1–2
Typically, orthodontic brackets are either directly bonded intraorally or indirectly bonded on stone models and then transferred to the mouth. Previous research comparing the accuracy of the two techniques, both to each other and to the prescribed bracket position, has left much to be debated.3–5 What has been fairly well agreed upon, however, is that neither technique provides the clinician with a consistent and accurate method of bracket placement.
OrthoCAD (Cadent Inc, Carlstadt, NJ) has developed OrthoCAD iQ, a system designed to select bracket positions digitally and then reproduce those positions intraorally using an indirect bonding technique. Based on the orthodontist's treatment plan, OrthoCAD produces a virtual diagnostic set-up with the teeth positioned in an ideal alignment. Bracket positions are then selected using these simulated posttreatment models. OrthoCAD iQ then uses a pen-sized “wand,” consisting of a tip, a miniature video camera, and eight LEDs, to transfer the brackets to the targeted tooth location on the plaster models.6 By accurately and reliably directing the brackets to their specified locations, OrthoCAD claims to reduce the frequency and number of wire bending and repositioning appointments, thus improving practice efficiency.7
Until now, no objective research has been conducted to evaluate the claims made that the OrthoCAD iQ system provides better or more reliable orthodontic bracket positioning than currently applied bonding techniques.
The purposes of this study are (1) to determine the quality of intra-arch dental alignment at the end of orthodontic treatment in cases utilizing OrthoCAD iQ, (2) to investigate the reliability of OrthoCAD iQ in bracket positioning, and (3) to identify potential strengths and weaknesses in bracket positioning when utilizing OrthoCAD iQ.
MATERIALS AND METHODS
Twenty-eight artificial teeth (Kilgore International Inc, Coldwater, Mich) were set in preformed wax rims, arranged in an Angle Class I malocclusion with minimal overjet, and moderate crowding in both arches. No teeth were aligned in such a manner as to prevent bracket placement at the center of the clinical crown.
One set of Kromopan (Lascod S.p.a., Florence, Italy) alginate impressions was taken of the original malocclusion and immediately poured up in low expansion white FlowStone (Whip Mix Corp, Louisville, Ky) following the manufacturer's water/powder ratio of 22 mL/100 g. Using a positive pressure thermal-forming Biostar (Great Lakes Orthodontics Ltd, Tonawanda, NY) to create a negative template of the original malocclusion, 46 duplicate models were fabricated and randomly divided into two sample groups.
For the purpose of the study, it was necessary to recreate the original malocclusion in a medium that allowed both easy removal and replacement of the artificial teeth. The 28 teeth were removed from the wax and separated into posterior and anterior groups. The posterior groups were further subdivided between premolars and molars to ensure correct orientation of each tooth. The groups were set into separate blocks of oven-set clay (Polyform Products Co, Elk Grove Village, Ill) and baked following the manufacturer's instructions. Exact recreation of each tooth's initial malposition was verified using different thicknesses of pressure-formed trays fabricated off the original malocclusion.
Forty-six cases of 3M Unitek twin metal brackets and molar tubes were donated for this study. Each bracket contained a slot size of 0.022 × 0.028 inches and a tip and torque following the MBT prescription (3M Unitek, Monrovia, Calif). Other than the molar tubes, no brackets had hooks to avoid any potential interference when the brackets were bonded to the plaster models.
Twenty-four sets of models were individually shipped to OrthoCAD on different days over an extended period of time. To improve the validity of the study, each set of models was disguised with a different patient name and treatment provider, in an attempt to keep the company as a blind participant. Following the protocol established by OrthoCAD, models were packaged along with a bite registration, brackets, and their treatment plan/instruction sheet. The exact same materials were included in all 24 cases sent to OrthoCAD. When the virtual set-up was returned for evaluation by the orthodontist, the case was accepted without modification, and indirect bonding (IDB) trays were ordered.
The remaining 22 sets of models were randomly distributed to participating faculty and residents at the University of Illinois at Chicago (UIC) Department of Orthodontics. Altogether, two faculty members who have been solely practicing indirect bonding for many years, and two senior residents who have been using the indirect bonding technique for more than 1 year consistently participated in this study. All clinicians used the same techniques in bracket placement. All clinicians were asked to bond the maxillary and mandibular arches in a time frame representative of their typical bonding and to utilize the tools they normally employed. All indirect bonding trays for this sample group were fabricated using a two-tray technique similar to that of OrthoCAD.
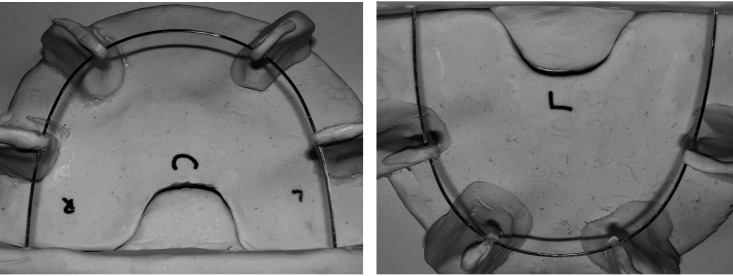
To simulate treatment outcome with the alignment of teeth based solely on the position of each bracket, it was necessary to design a “jig” that consistently positioned the dentition on the exact same rectangular archwire. To accomplish this, two 0.021 × 0.025-inch stainless steel archwires (3M Unitek) were coordinated and mounted on oven-baked clay (Figure 1). Each wire was elevated above the base to avoid root interferences, as well as braced at multiple points to limit deflection. A level was used to verify that the posterior segments were secured in the same plane of space.
Figure 1.
Mounted maxillary and mandibular archwires.
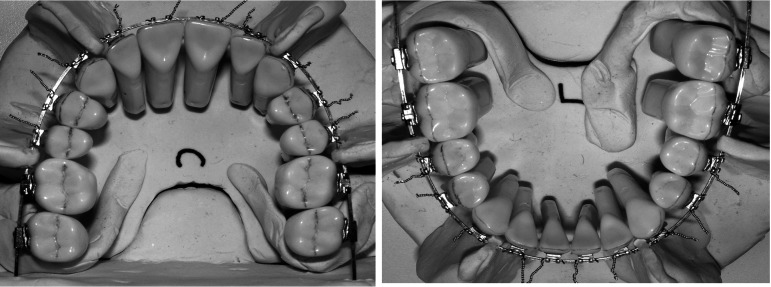
The entire complement of typodont teeth in each sample was then removed from their blocks and ligated on the mounted wires. The molar tubes were slid on the back of each wire until the mesial surface of the first molar contacted the distal surface of the second premolar (Figure 2). Any sample that had a bracket debond during ligation of the teeth was removed from the study. The examiner felt that there was too much inaccuracy in replacing the bracket in the IDB trays and rebonding to consider this an option in the study.
Figure 2.
Artificial teeth mounted on upper (left) and lower (right) archwires.
Simulated posttreatment set-ups were evaluated using the intra-arch components of the American Board of Orthodontics (ABO) objective grading system (OGS). The four components utilized were alignment, marginal ridges, buccolingual inclinations, and root angulations. A total score for each sample was also recorded, representing a sum of the components.
One investigator who has attended an ABO calibration course was responsible for scoring all of the posttreatment set-ups in this study. The first 10 samples were scored twice, with a minimum of 1 week between each recording. Total OGS scores and each corresponding component were compared using Pearson correlations to verify positive intraexaminer reliability.
All data gathered from the OGS scores of both sample groups were entered into a data file for statistical analysis using the Statistical Package for Social Sciences Version 10 (SPSS, Chicago, Ill). Independent sample t-tests were utilized to evaluate differences between total scores, the corresponding intra-arch components, as well as the ranges of scores. Individual teeth within each component were also compared to isolate potential strengths and weaknesses in bracket placement.
RESULTS
The first 10 posttreatment set-ups were tested for intraexaminer error. Each of the 10 pairings was found to be significantly correlated at a .01 or 99% level.
Six samples were removed from this study (four from the OrthoCAD group and two from the traditional IDB group) as a result of bonding failures on one or more teeth, leaving the sample to be exactly 20 in each group. Overall, however, the bond strength between bracket and artificial tooth proved high enough to avoid significant problems.
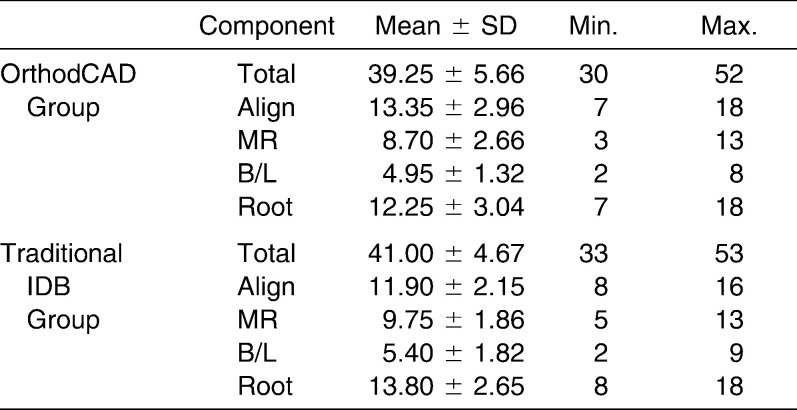
The overall mean score for posttreatment set-ups of the OrthoCAD group was 39.25 points with a standard deviation of 5.66 points and a range from 30 to 52 points. Alignment had the most points deducted at 13.35 points, followed by root angulations, marginal ridge discrepancies, and lastly, buccolingual inclinations at 4.95 points (Table 1).
Table 1.
OGS Scores
The overall mean for the posttreatment set-ups of the traditional IDB group was 41.00 points with a standard deviation of 4.67 points and a range from 33 to 53 points. Root angulations had the most points deducted at 13.80 points, followed by alignment, marginal ridge discrepancies, and buccolingual inclinations at 5.40 points (Table 2).
Table 2.
Comparsion of OGS Scores Between Sample Groups
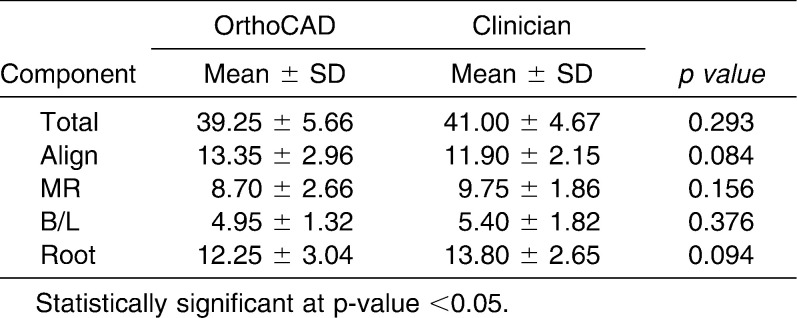
Independent sample t-tests revealed no statistically significant differences between total OGS scores or any of the individual intra-arch components (Figure 3). Differences in average point deductions per tooth were compared between sample groups as well.
Figure 3.
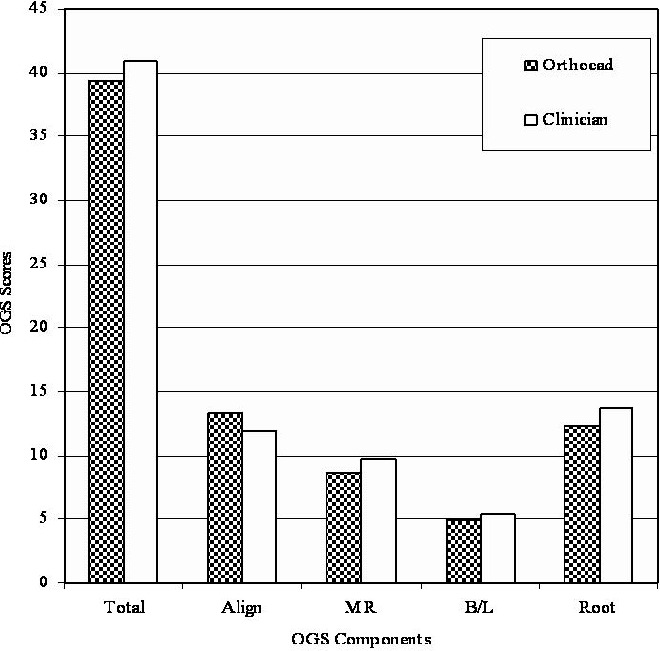
Comparison of total OGS scores and their components between posttreatment set-ups bonded by OrthoCAD and faculty/residents.
The average point deduction for alignment errors was 0.96 in the OrthoCAD sample and 0.85 in the traditional IDB sample. The upper canines scored the worst in both sample groups, while the lower centrals and lower second molars scored the best.
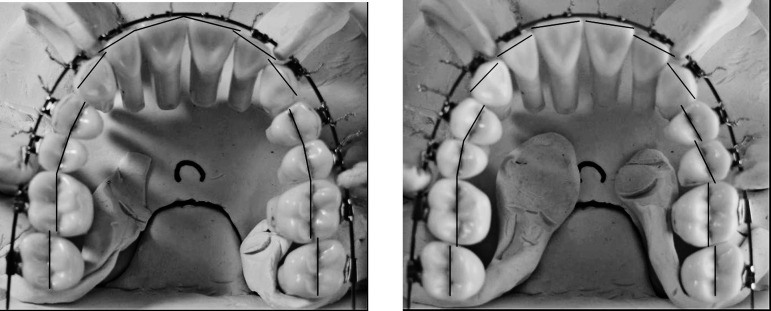
Both the upper and lower first premolars were found to score statistically higher in the OrthoCAD sample group than the traditional IDB group (Figures 4 and 5).
Figure 4.
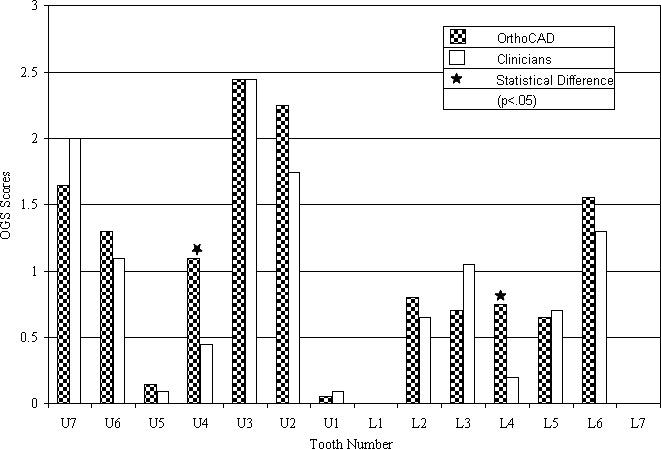
Comparison of mean point deductions of individual teeth within the alignment component of the OGS.
Figure 5.
Examples of simulated posttreatment set-ups with well aligned (left) and poorly aligned (right) maxillary arches, based on their OGS scores.
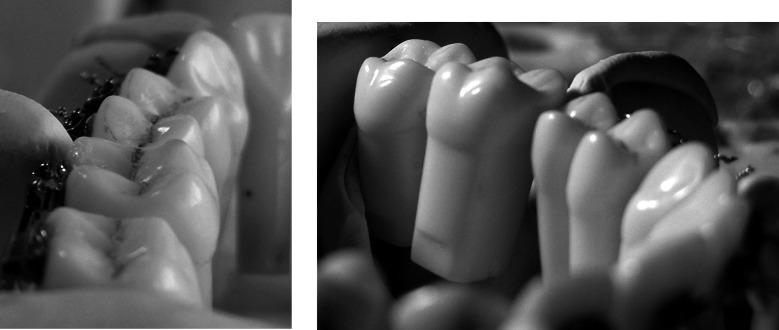
The average point deduction for marginal ridge discrepancies between posterior contacts was 1.44 in the OrthoCAD sample and 1.63 in the traditional IDB. The contact with the highest mean point loss in both sample groups was the upper first to second molars. The contact with the lowest mean point loss was the upper second premolars to first molars in the OrthoCAD group and the lower first to second premolars in the traditional IDB group. Independent t-tests revealed that two contacts in the OrthoCAD group had marginal ridge discrepancies that scored statistically lower than those of the traditional IDB group. The contacts between the upper first molars to second premolars and the upper first premolars to second premolars each had average point losses that were lower in the OrthoCAD sample group (Figures 6 and 7).
Figure 6.
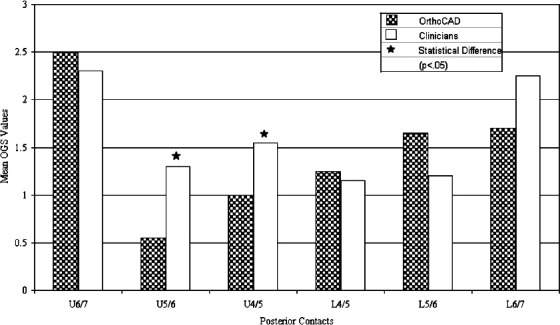
Comparison of mean point deductions of individual teeth within the marginal ridge component of the OGS.
Figure 7.
Examples of simulated posttreatment set-ups with well positioned (left) and poorly positioned (right) marginal ridges, based on their OGS scores.
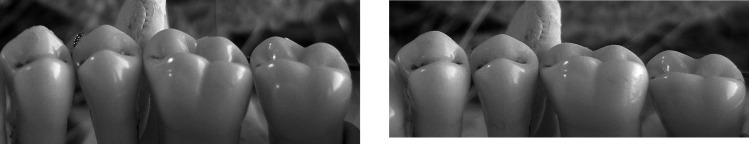
The average point deduction for improper buccolingual inclination of the posterior teeth was 0.71 in the OrthoCAD sample group and 0.77 in the traditional IDB group. The upper first premolars scored the worst in both sample groups while the upper second molars scored the best. Independent sample t-tests revealed that three teeth scored significantly different between the two sample groups. The mean point loss of the upper first premolars was statistically higher in the OrthoCAD group, while both the lower first and second molars were statistically lower. The results of these tests are in Table 7 (Figures 8 and 9).
Figure 8.
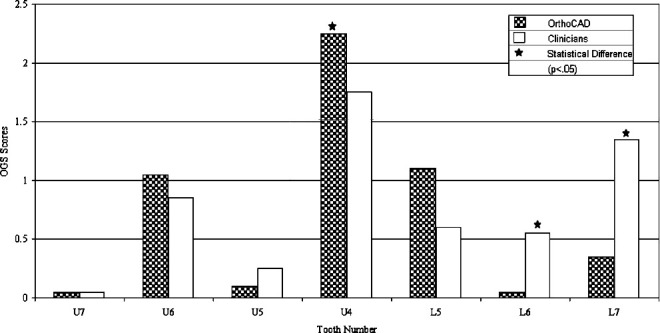
Comparison of mean point deductions of individual teeth within the buccolingual inclination component of the OGS.
Figure 9.
Examples of simulated posttreatment set-ups with proper (left) and poor (right) buccolingual inclination of the maxillary left first molars, based on their OGS scores.
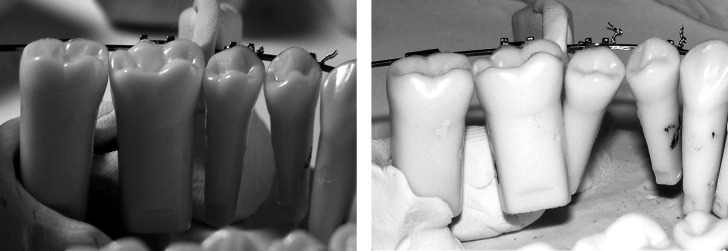
The average point deduction for errors in root angulation was 0.88 in the OrthoCAD sample group and 0.99 in the traditional IDB group. The teeth with the highest mean point loss in both sample groups were the upper first premolars. The upper central incisor had the lowest point loss in both groups, while the traditional IDB also scored well on the upper first molar. Independent sample t-tests revealed that OrthoCAD had a significantly lower mean point loss for angulation errors on the upper second premolars and the lower first molars. The lower lateral incisors, on the other hand, scored significantly higher within the OrthoCAD group than in the traditional IDB sample group (Figures 10 and 11).
Figure 10.
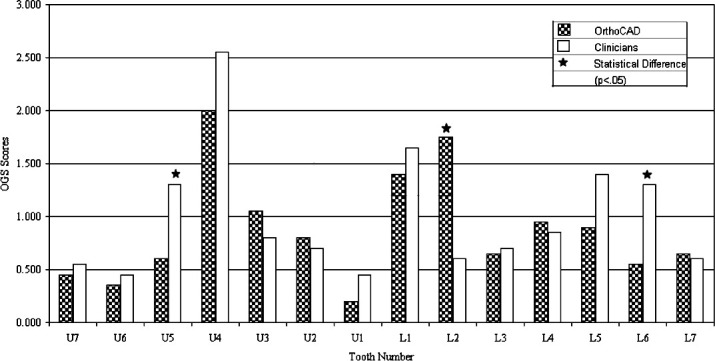
Comparison of mean point deductions of individual teeth within the root angulation component of the OGS.
Figure 11.
Examples of simulated posttreatment set-ups with well angulated (left) and poorly angulated (right) lower right posterior segments, based on their OGS scores.
DISCUSSION
OrthoCad iQ is a computer-based system that projects itself as the future of orthodontics. Advertisements clearly state that with the use of their product, orthodontists will decrease bracket repositions and wire bends needed to achieve excellent treatment. Simulated treatment outcomes based solely on bracket position, however, did not support these claims. Comparisons of the overall orthodontic “finish” between OrthoCAD and faculty/residents showed no statistical or clinical differences.
A suggested advantage of the OrthoCAD bracket placement system is that, with its capability for digital precision, the reliability in positioning orthodontic brackets should far surpass that of the human eye. OrthoCAD received the exact same models on 20 different occasions and was asked to produce the same treatment results with each. What was found, however, was a large range of posttreatment OGS scores that mirrored the range produced by the faculty and residents participating in the study. The variability observed in the traditional IDB group could have been predicted. Previous studies have demonstrated the poor reliability generally experienced by orthodontists when positioning brackets.3,5
The large range of OGS scores found in the OrthoCAD sample group is possible considering that several of the steps in the OBPS still involve human cooperation. Once the bracket position is finalized on the virtual set-up, a laboratory technician must use the company's “wand” to transfer the selected position to a stone model for fabrication of the indirect bonding tray. This step is technique sensitive and may introduce a high level of user error in the product.
It has been argued by some that comparing the digital bracket position with intra-oral photographs after bonding is evidence of the precision of their system.8 The results from the study did not find the two images to correlate nearly as well.
To identify potential strengths and weaknesses of the OrthoCAD system, individual bracket positions were assessed by further analysis within the OGS components. Methodologic differences, however, make it difficult to compare specific individual bracket errors with those of other studies.3–5
OrthoCAD had a significantly higher point average than the traditional IDB group on its upper premolars in both alignment and buccolingual inclination. The upper first premolars also received the highest point deductions for root angulation, though no statistical difference was found between sample groups. In assessing the original malocclusion, it is clear that the upper right first premolar is the most severely malaligned tooth in either arch. This may partially explain the inability of OrthoCAD to orient the tooth, although the traditional IDB group scored quite well in alignment of upper first premolars.
OrthoCAD also had difficulty in placing the brackets along the long axis of the four lower incisors. The mean point loss of the lower lateral incisors in the root angulation component was significantly higher than that of the traditional IDB group.
The marginal ridge component of the OGS looks at discrepancies between adjacent posterior teeth. This variable, unlike others, assesses vertical positioning errors between neighboring teeth. OrthoCAD was significantly better at positioning the upper premolars and first molars at the same level. This particular finding makes sense because OrthoCAD creates a diagnostic set-up before virtually positioning its brackets.
Visualizing differences in marginal ridges in a pretreatment malocclusion is one of the greatest challenges faced when bonding posterior teeth. Eliades et al.9 in their study on premolar bracket positioning showed that even aligning the bracket slot with the center of the clinical crown can consistently produce unbalanced proximal contacts in excess of 1 mm. The findings from this study agree with the conclusions of Eliades et al.9 The faculty/resident sample group averaged greater than one point per contact in both the upper and lower posterior segments. The virtual set-up allowed easier visualization of adjacent marginal ridges and a greater ability to position adjacent bracket slots along the same line.
The major limitation of this study was the inability to gather a larger sample size. Both time and expense did not allow the examiner to gather a size that could have minimized the potential for type II error. It is impossible, therefore, to conclude definitively that differences between the sample groups did not exist. Another limitation of this study was the inability to equally blind both sample groups. Though OrthoCAD, our test group, was unaware of their participation in this study, it was too difficult to equally blind the group of faculty and residents. In an attempt to reduce any bias that could arise from this group, each participating clinician was asked to perform their indirect bonding set-up in a time frame representative of a typical case.
CONCLUSIONS
No significant differences were found in total OGS scores or individual component scores of simulated posttreatment set-ups between OrthoCAD iQ and a group of faculty and residents at the UIC Department of Orthodontics.
OrthoCAD iQ produced a wide range of OGS scores with treatment of the same malocclusion, indicating a lower level of reliability than anticipated.
OrthoCAD iQ was significantly less successful at achieving proper alignment and buccolingual inclination of the upper first premolars and less successful at properly angulating the lower lateral incisors.
OrthoCAD iQ was significantly better at aligning the marginal ridges of the upper posterior segment from the first premolars to first molars, indicating a potential advantage to constructing a virtual diagnostic set-up before selecting bracket positions.
REFERENCES
- 1.Carlson S. K, Johnson E. Bracket positioning and resets: five steps to align crowns and roots consistently. Am J Orthod Dentofacial Orthop. 2001;119:76–80. doi: 10.1067/mod.2001.111220. [DOI] [PubMed] [Google Scholar]
- 2.McLaughlin R. P, Bennett J. C. Bracket placement with the preadjusted appliance. J Clin Orthod. 1995;29:302–311. [PubMed] [Google Scholar]
- 3.Aguirre M. J, King G. J, Waldron J. M. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1982;82:269–276. doi: 10.1016/0002-9416(82)90461-4. [DOI] [PubMed] [Google Scholar]
- 4.Hodge T. M, Dhopatkar A. A, Rock W. P, Spary D. J. A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J Orthod. 2004;31:132–137. doi: 10.1179/146531204225020427. [DOI] [PubMed] [Google Scholar]
- 5.Koo B. C, Chung C. H, Vanarsdall R. L. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116:346–351. doi: 10.1016/s0889-5406(99)70248-9. [DOI] [PubMed] [Google Scholar]
- 6.Mayhew M. Computer-aided bracket placement for indirect bonding. J Clin Orthod. 2005;39:653–660. [PubMed] [Google Scholar]
- 7.Redmond W. J, Redmond M. J, Redmond W. R. The OrthoCAD bracket placement solution. Am J Orthod Dentofacial Orthop. 2004;125:645–646. doi: 10.1016/j.ajodo.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Garino F, Garino G. B. Computer-aided interactive indirect bonding. Prog Orthod. 2005;6:214–223. [PubMed] [Google Scholar]
- 9.Eliades T, Gioka C, Papaconstantinou S, Bradley T. G. Premolar bracket position revisited: proximal and occlusal contacts assessment. World J Orthod. 2005;6:149–155. [PubMed] [Google Scholar]