Box 1.
Expert panel opinions
| Parameters | Expert opinion | |
|---|---|---|
| Risk and risk assessment | A CCT using either ultrasonic or optic is recommended for risk stratification | |
| There is no merit in using formulas or nomograms to convert IOP | ||
| In the absence of data on CCT and risk in Indian patients, the panellists did not suggest any range of CCT for risk profiling | ||
| Screening for glaucoma | Opportunistic glaucoma screening during cataract camps or a visit to an eye clinic is a possible method of screening glaucoma | |
| There is a lack of evidence on the cost effectiveness of screening, diagnosing, monitoring, and treating glaucoma in India. Hence, glaucoma screening may be done at the discretion of individual hospitals or ophthalmologists | ||
| Diagnosis | Despite a low level of evidence, the panelists agreed to strongly recommend using visual acuity and refractive errors, slit-lamp examination, gonioscopy, tonometry, visual field testing, and clinical assessment of ONH, RNFL, and macula | |
| The panelists do not recommend CCT adjusted IOP values because CCT-corrected algorithms based on IOP are not validated | ||
| Diagnosis of glaucoma should not be made on the OCT findings alone | ||
| Central corneal thickness can be considered in case of normal tension glaucoma or ocular hypertension | ||
| Goldmann applanation tonometry is the gold standard for diagnosing glaucoma, and hence it is recommended over other tonometers | ||
| The accuracy and precision of a tonometer should influence the choice for use in the clinic | ||
| Tonometer must be regularly calibrated. For more details, refer to the APGS guideline | ||
| Anterior chamber angle imaging cannot replace gonioscopy. | ||
| Gonioscopy should be performed in every patient being evaluated for glaucoma | ||
| Some form of photography or imaging of ONH and RNFL features is recommended as sequential photographs help to detect progression | ||
| If photos are unavailable, a disc drawing enumerating the disc is warranted | ||
| Diagnosis of glaucoma should not be made on the OCT findings alone | ||
| Do not rely only on the CDR to describe or document the disc | ||
| Setting target IOP | The IOP target must be individualized to the eye and revised at every visit | |
| Target IOP is the upper limit of IOP judged to be compatible with this treatment goal | ||
| Documentation of target IOP is up to the discretion of the ophthalmologist | ||
| In early glaucoma, an IOP of 18-20 mmHg with a reduction of at least 20% may be sufficient | ||
| In moderate glaucoma, an IOP of 15-17 mmHg with a reduction of at least 30% may be required | ||
| In advanced glaucoma, a reduction of at least 40% may be required | ||
|
|
||
| Glaucoma stages | Target IOP to be achieved | |
|
| ||
| Mild glaucoma | 18.20 mmHg | |
| Moderate glaucoma | 15.17 mmHg | |
| Advanced glaucoma | 10.12 mmHg | |
|
| ||
| Topical glaucoma therapy | Start with monotherapy (except in high IOP and severe disease) | |
|
||
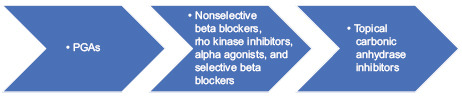
| The order of IOP lowering medications based on their IOP lowering efficacy is as follows: | ||
| Prostaglandin analogues are the most effective medications and are usually recommended as the first choice in OAG, provided the cost is not a limiting factor | ||
| Laser iridotomy | Laser iridotomy should be preferred over surgical iridotomy | |
| Laser trabeculoplasty | Selective laser trabeculoplasty is available in India in many ophthalmology departments. It could be tried as a first-line treatment in mild-to-moderate glaucoma, but it is not a universal recommendation | |
| Thermal laser peripheral iridoplasty | Once-daily pilocarpine can be used as an alternative to thermal laser peripheral iridoplasty (TLPI) for plateau iris syndrome and patent peripheral iridotomy | |
| Cyclodestructive procedures | Transcleral cyclophotocoagulation is the most commonly used method in India | |
| Incisional surgery | The commonly preferred surgical technique for penetrating glaucoma surgery is the nonpenetrating glaucoma surgery is not useful in the Indian context | |
| Minimally invasive glaucoma surgery | Minimally invasive glaucoma surgery is not widely available in India and hence no recommendations are made | |
| Antifibrotic agents in glaucoma management | Mitomycin C is the choice of drug in glaucoma surgery | |
| Antifibrotics should be judiciously used | ||
| Intraoperative mitomycin can be used at 0.1-0.4 mg/mL for 1-3 min, depending on the condition of the disease | ||
| Postoperatively both 5-FU and mitomycin-C can be used | ||
| 5-FU concentration: 0.1 mL injection of 50 mg/mL undiluted solution. It has to be administered as subconjunctival injection adjacent to but not into bleb (pH 9), with a small-caliber needle (e.g., 30 G needle on insulin syringe) Mitomycin C concentration: 0.1 mL injection of 0.1-0.5 mg/mL solution. It must be administered adjacent to but not into bleb, with a small-caliber needle (e.g., 30 G needle on insulin syringe) |
||
| Cataract and glaucoma surgery | In patients with cataract and PACG, phacoemulsification alone or combined phacoemulsification+glaucoma surgery is recommended. However, the decision should be made based on the disc and field damage and the status of the angle | |
| Open-angle glaucoma | Trabeculectomy augmented with antifibrotic agents is recommended as initial surgical treatment for OAG, provided the ophthalmologist is familiar with the use of antifibrotics. | |
| Antifibrotics should be used with caution | ||
| Alternatives like OlogenÒ should not be a preferred option due to a lack of evidence on its equality of superiority over trabeculectomy | ||
| Angle-closure disease | Treatment of PACG depends on the spectrum of disease and presence of cataract | |
| Laser peripheral iridotomy and surgery is combined with medical treatment should be considered in high-risk individuals below the age of 50 years, e.g., high hyperopia, and patients requiring repeated pupil dilation for retinal disease | ||
| Primary angle-closure suspect: LPI in high-risk individuals such as those with very high hyperopia, family history, or those requiring pupil dilatation due to retinal disease | ||
| PAC or PACG: Laser peripheral iridotomy is the first line of treatment | ||
| Visually significant cataract and PAC: Laser peripheral iridotomy to manage PAC or PACG and lens | ||
| extraction should be considered based on level and extent of angle closure and IOP | ||
| There may be a risk of aqueous misdirection or surgical complications if cataract surgery is done without LPI in patients with cataract and PAC or PACG | ||
| Ophthalmologists should be proficient in handling patients with cataract and PAC or PACG | ||
| Prostaglandin analogues are the most effective medications and are usually recommended as the first choice in PACG | ||
| In patients with phakic and PACG, phacoemulsification alone or combined phacoemulsification + glaucoma surgery is recommended. However, the decision should be made based on the disc and field damage and the status of the angle | ||
| Monitoring glaucoma progression | Despite a very low level of direct evidence, the panelists endorsed the EGS recommendations | |
| Keeping in view the goal of preventing vision impairment, the visual acuity, VF testing, clinical assessment of the optic disc and RNFL, tonometry is strongly recommended for monitoring glaucoma progression. | ||
| However, OCT of disc/RNFL/macula and repeat gonioscopy carries a weak recommendation | ||
| In preperimetric glaucoma, OCT is used for monitoring the disease progression. Visual field is mandatory for diagnosing and monitoring the progression of glaucoma | ||
| OCT is always complementary to visual field testing but cannot replace visual field testing in monitoring glaucoma progression | ||
CCT, Central corneal thickness; CDR, cup-to-disc ratio; OAG, open-angle glaucoma; OCT, optical coherence tomography; IOP, intraocular pressure; LPI, laser peripheral iridotomy; ONH, optic nerve head; PGAs, prostaglandin analogues RNFL, retinal nerve fiber layer; PAC, primary angle closure; PACG, primary angle-closure glaucoma.
