Abstract
Objective:
To describe the dentoskeletal and soft tissue effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions (Alt-RAMEC) in maxillary retrusion patients.
Materials and Methods:
The sample consisted of 15 patients with a mean skeletal age of 11.6 ± 1.59 years undergoing 8 weeks of Alt-RAMEC followed by maxillary protraction. Three hundred fifty to 400 g of force per side was applied to the facemask from the titanium miniplates inserted on the lateral nasal wall of the maxilla. Total treatment time was 9.9 ± 2.63 months. Treatment changes were evaluated cephalometrically and analyzed by means of the dependent t-test and the Wilcoxon signed rank test.
Results:
The miniplates withstood the orthopedic forces exerted during the treatment. Cephalometric findings showed that the maxilla moved forward by 2 mm, with an 0.8° counterclockwise rotation and without maxillary incisor movement. The mandible moved slightly in a downward and backward direction (1.2°). The inclinations of the mandibular incisors decreased significantly (2°). Statistically significant increases were observed in the vertical dimension (1°–1.3°). Soft tissue changes were more marked in the upper lip and soft tissue pogonion than in the lower lip.
Conclusions:
This treatment approach can offer an advantage for correcting mild/moderate maxillary retrusion in Class III patients.
Keywords: Facemask, Miniplate, Alt-RAMEC, Maxillary retrusion
INTRODUCTION
Facemask has been successfully used for the correction of Class III malocclusion since the late 1960s.1–3 The main effects of conventional facemask therapy are maxillary forward movement and sutural remodeling.4,5 Rapid maxillary expansion (RME) has been recommended for use in conjunction with facemask because it disrupts circummaxillary and intermaxillary sutures and facilitates the orthopedic effect of facemask.6,7 However, it has been reported8–11 that circummaxillary sutures may not be well disarticulated by use of RME alone and might be better managed by the use of alternate RME and constriction (Alt-RAMEC).
When using toothborne appliances in conjunction with facemask, some dental compensation (maxillary incisor proclination) is observed.12–14 The purpose of orthopedic treatment should be the achievement of skeletal changes rather than dental compensation. Thus, a more rigid anchorage is critical for a pure orthopedic-forward movement of the maxilla. Transferring the force to the maxilla with a rigid anchorage device has been attempted previously.15–21 Facemask treatment with miniplate anchorage has rarely been discussed.18–21 The literature concerning the facemask treatment anchored with miniplate comes in the form of case reports,19–21 except for one study18 with a small sample size. Therefore, the aim of this prospective study was to evaluate the dentoskeletal and soft tissue effects of the Delaire-type facemask treatment anchored with miniplates in maxillary retrusion patients.
MATERIALS AND METHODS
The study group consisted of 15 patients (nine females, six males) with a mean skeletal age of 11.6 ± 1.59 years, according to the atlas of Greulich and Pyle.22 The patients met the following criteria: no history of previous orthodontic/orthopedic treatment, no systemic diseases or congenital deformities, concave profile, skeletal and dental Class III malocclusion, edge-to-edge/reverse incisor relationship, and symptom-free temporomandibular joint function. This study was approved by the Ethical Committee of the Hacettepe University Medical School. (The Institutional Approval number for this study is LUT 06/91-20.) Parents and patients were informed about the treatment; they agreed to participate in the study and signed informed consent forms.
A bonded RME appliance was fabricated for each patient. The screw of the RME appliance was alternately opened and closed for 2-week periods over the course of 8 weeks in order to disarticulate the circummaxillary sutures. The treatment protocol began with expansion, followed by final constriction. Daily activation for the expansion/constriction course was 0.5 mm. After the final constriction course, surgical preparation was completed. While the patient was under local anesthesia, a vertical incision was made at the labial vestibule between the lateral incisors and canines on both sides. When necessary, horizontal incisions were made on the left and/or right sides of the vertical incisions. The mucoperiosteal flap was then elevated, and titanium miniplates designed by Erverdi et al.23 (Multipurpose Implant; Tasarimmed, Istanbul, Turkey) were adapted to the lateral nasal wall of the maxilla. Straight extensions of the miniplates were bent distally to avoid applying pressure to the attached gingiva and so that elastics could be applied. After predrilling with a 1.3-mm–diameter bur under copious irrigation, the miniplates were fixed with three screws (2-mm diameter, 5 or 7 mm in length; Mondeal, Tuttlingen, Germany) (Figure 1). Incisions were closed with 4/0 vicryl sutures. The patients were prescribed antibiotics, analgesics, and a 0.012% chlorhexidine rinse, which they were to use for 1 week. One week after surgery, the miniplates were examined via a panoramic radiograph (Figure 2).
Figure 1.

Titanium miniplate after attachment to the lateral nasal wall of the maxilla.
Figure 2.
Panoramic radiograph after surgery.
After soft tissue healing (10 days), a Delaire-type facemask was adjusted for the patients, and 100 g of force per side was applied via elastics between the miniplates and facemask. The force was increased by 350–400 g per side during the second week of treatment. The direction of force was 30° forward and downward to the occlusal plane, so that the force vector was closer to the center of the resistance of the nasomaxillary complex. The patients were advised to wear the facemask full time and were seen every 3 weeks to control the force. When the desired forward movement of the maxilla was achieved for a good profile, the miniplates and bonded RME appliance were removed. The total treatment time, including 8 weeks of the Alt-RAMEC protocol, measured 9.9 ± 2.63 months.
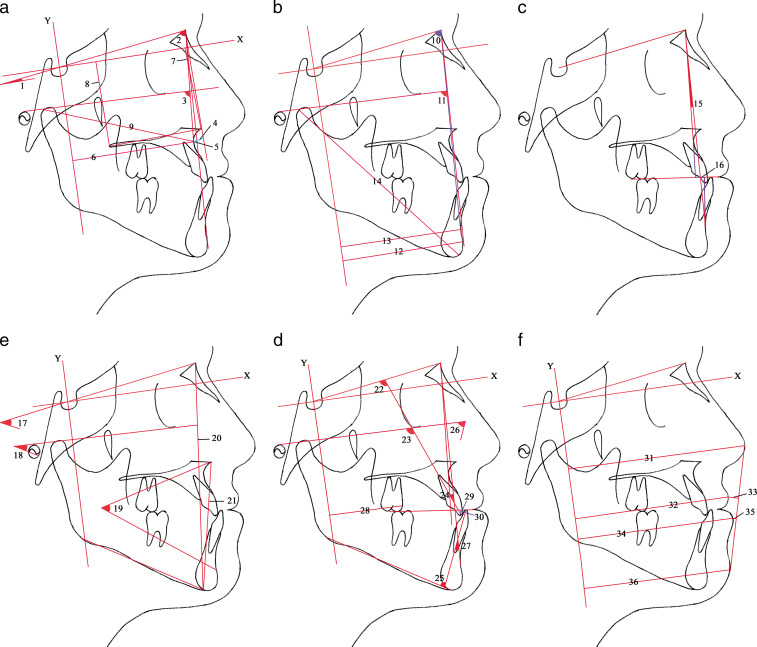
Lateral cephalometric radiographs were taken before treatment and after maxillary protraction using a standardized protocol. Cephalometric analysis was made based on a reference system in addition to conventional cephalometric analytical methods. A horizontal reference line (X) through the sella was constructed down anteriorly 7° to the SN line, and a perpendicular line was constructed through the sella as the vertical reference line (Y). Twenty-one linear and 15 angular measurements were evaluated (Figure 3a–f).
Figure 3.
Cephalometric measurements used in the study: (a) X, horizontal reference plane; Y, vertical reference plane; 1, palatal plane angle (ANSPNS-SN) (°); 2, SNA (°); 3, maxillary depth (FH-NA) (°); 4, McNamara (A-Nperp) (mm); 5, convexity (A-NPog) (mm); 6, A-Y (mm); 7, ANS-X (mm); 8, PNS-X (mm); and 9, Maxillary length (Co-A) (mm). (b) 10, SNB (°); 11, Facial depth (FH-NPog) (°); 12, Pog-Y (mm); 13, B-Y (mm); and 14, Mandibular length (Co-Gn) (mm). (c) 15, ANB (°); 16, Witts appraisal (mm). (d) 17, GoGn-SN (°); 18, FMA (°); 19, Lower facial height (ANS-Xi-Pm) (°); 20, N-Me (mm); and 21, ANS-Me (mm). (e) 22, U1-SN (°); 23, U1-FH (°); 24, U1-NA (°); 25, IMPA (°); 26, FMIA (°); 27, L1-NB (°); 28, U6m-Y (mm); 29, overjet (mm); and 30, overbite (mm). (f) 31, Pr-Y (mm); 32, Ls-Y (mm); 33, Ls-E (mm); 34, Li-Y (mm); 35, Li-E (mm); and 36, sPog-Y (mm).
Normality of the data was tested with the Shapiro-Wilks test. Statistical evaluation was conducted using a dependent t-test when the data displayed a normal curve, and a Wilcoxon signed rank test was used when the data did not display a normal curve.
RESULTS
With the exception of one patient, the patients' miniplates were stable during treatment on the right side a month after starting the treatment. When the miniplates were removed, bone apposition around them was observed (Figure 4).
Figure 4.
Bone apposition around the miniplate.
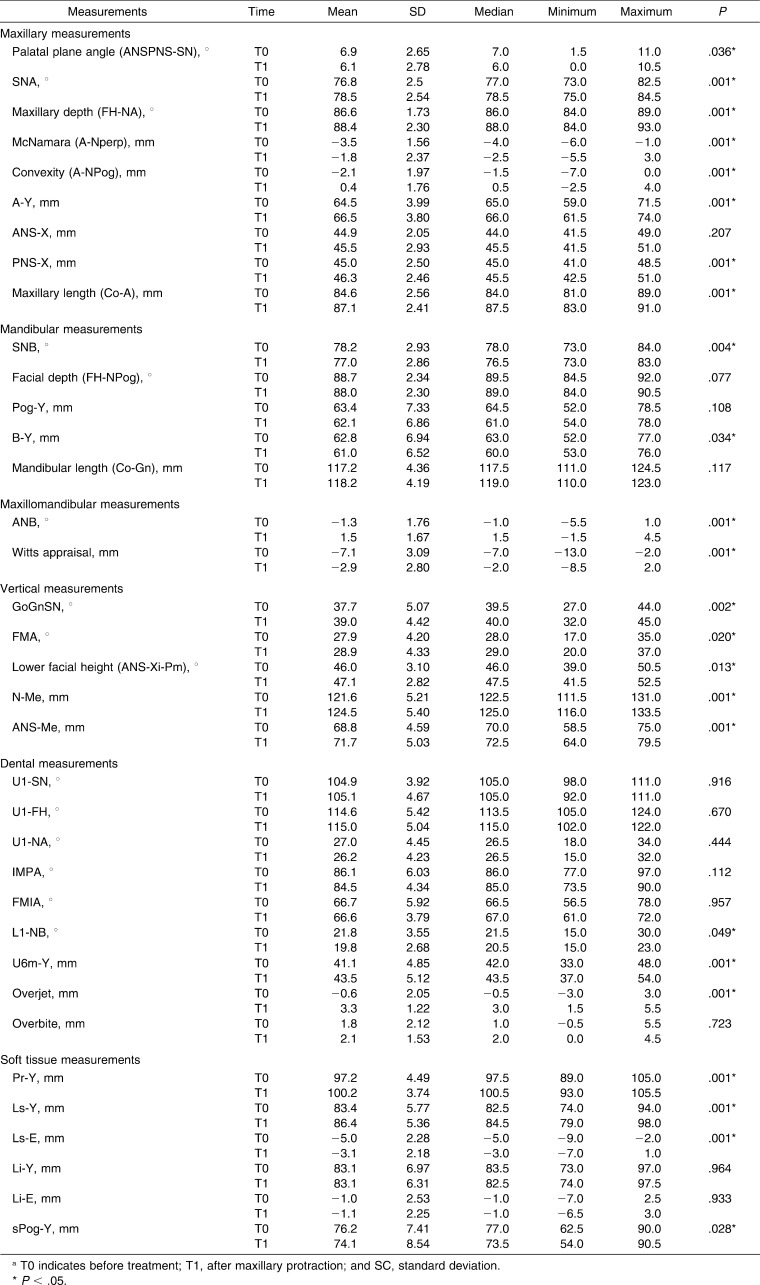
The cephalometric effects of the treatment are summarized in Table 1. The results revealed that the maxilla was displaced forward, with statistically significant increases in SNA, maxillary depth, McNamara, convexity, A-Y distance, and maxillary length. A statistically significant increase in PNS-X distance and no change in ANS-X distance resulted in a statistically significant counterclockwise rotation of the palatal plane. Skeletal effects on the mandible included statistically significant decreases in SNB and B-Y distance. Facial depth, mandibular length, and Pog-Y distance showed no significant changes with treatment. Increases in ANB and the Witts appraisal were found to be statistically significant. In addition, significant increases were observed for all vertical measurements (1°–1.3° and 2.9 mm).
Table 1.
Cephalometric Changes After Delaire-Type Facemask Anchored With Miniplatea
There were no statistically significant changes in any measured variable along the mean maxillary and mandibular incisor angulations, except for L1-NB. The L1-NB angle decreased significantly. The maxillary first molar (U6-Y) moved forward 2.4 mm. Overjet showed a statistically significant increase, whereas the overbite did not change.
Treatment effects on the facial profile were emphasized by statistically significant increases in Ls-Y and Ls-E distances and a statistically significant decrease in sPog-Y distance. No change was found in Li-Y and Li-E distances. Pr-Y distance showed a statistically significant increase with age.
DISCUSSION
It has been reported that facemask treatment should be started at early ages24–26 because sutures become highly interdigitated27 and dental changes rather than skeletal changes are achieved in older ages.5,25,26,28 To disarticulate circummaxillary sutures, at least 12–15 mm of expansion is required.29,30 However, the maxilla may be wider than the mandible after such an expansion. The Alt-RAMEC protocol was developed for disarticulating circummaxillary sutures without overexpansion.8–11 The treatment of our patients with a conventional facemask application would result in dental compensation of the skeletal problem. Therefore, we used a facemask with rigid anchorage in combination with an Alt-RAMEC protocol to achieve more positive reactions to the protraction forces. A control group (to distinguish the effects from those associated with growth) was not included in the study because of ethical concerns.
To provide rigid anchorage, ankylosed primary canine,31 osseointegrated implant,20 onplant,17 miniscrew,16 and miniplate18–21 have been reported in the literature. We preferred the miniplate because it provided a reliable source of anchorage for orthopedic forces.18,19,21 In addition, miniplates can be bent easily, and force can be applied immediately, without waiting for osseointegration.
The lateral nasal wall of the maxilla is a critical region because the force vector is closer to the center of resistance of the nasomaxillary complex when the force is applied from this region.18 In addition, it is easier to place and remove the miniplates in this region, and this region provides good bone quality.
In all but one patient, the miniplates were stable during treatment. In this patient, mobility was observed for one miniplate. The mobility could be explained, since the miniplate was placed distal to the right maxillary canine, where the bone was thin because of the root of this tooth. The miniplate provided a stable anchorage in the later stages because titanium materials can undergo osseointegration with time.
Burstone and Marcotte32 concluded that forward movement of the maxilla was small and rarely more than 1–2 mm. Baik33 and Gautam et al.34 reported that greater forward movement of maxilla was achieved when the facemask was applied in conjunction with maxillary expansion. In Class III cases treated with rigid anchorage, the amounts of maxillary protraction varied between 3.0 and 5.6 mm.18,20,21 In our cases, a significant amount of maxillary protraction (2 mm) was achieved. The reasons for the differing amounts of maxillary protraction can include age, patient cooperation level, presence of cleft lip and palate, the magnitude of force used, the selected reference plane, and treatment duration.
Even if the direction of orthopedic force was 30° downward and forward from the occlusal plane, as recommended previously,35,36 a counterclockwise rotation of the palatal plane (0.8°) was observed. The amount of palatal plane rotation was smaller than observed in the other studies using rigid anchorage17–19 and was clinically negligible. In the study of Baek et al.,21 0.2°, 0.4°, and 0.8° of counterclockwise rotation of the palatal plane were reported. However, the patients in the study of Baek et al.21 had clefts, meaning that these patients did not have some/complete parts of the midpalatal suture and that the maxilla was not as rigid as in patients with a normal midpalatal suture. This rotation effect is greater (1.27°–1.44°) in the studies12,14,37 that used a conventional facemask system. Direct miniplate anchorage for facemask treatment after Alt-RAMEC protocol is likely to minimize the rotational effect.
Facemask therapy that delivers the force to the chin has a clockwise rotation effect on the mandible.12,14,18,33,37,38 In our study, a 1.2° decrease in SNB and a 1.8-mm decrease in B-Y distance were found. This rotation effect contributes to the correction of the Class III malocclusion.12 The lack of significance in the mean increase in mandibular length indicates a lack of limited effect of facemask on mandibular growth, which agrees with the study of Ngan et al.39 Baccetti et al.38 showed smaller increases for mandibular length in the treatment group compared with the untreated group.
Vertical dimension increases are a common effect of all variations of facemask treatment.12,14–16,18,37 Yuksel et al.40 reported greater increments in vertical dimension for a late treatment group (12 years, 6 months) than for an early treatment group (9 years, 8 months). In another study,41 2.17° of increase was observed for patients with a mean age of 11 years, 8 months. The mean skeletal age of our patients was 11.6 ± 1.59 years, and the increase in vertical dimension was minimal (+1°–1.3°).
Facemask treatment in conjunction with toothborne appliances results in proclination of maxillary incisors.12,23,38,39 In our study, direct bone anchorage with miniplate eliminated undesirable proclination of the maxillary incisors. The mandibular incisors uprighted slightly as a result of the force delivered by the facemask on the chin, as reported previously.42 Overjet was improved with the combination of dental and skeletal changes.12,38,39 The increase in overjet resulted from maxillary protraction, slight mandibular rotation, and mandibular incisor uprighting in this study. Clockwise rotation of the mandible and counterclockwise rotation of the palatal plane makes one think of the possibility of a decrease in overbite. The lack of change in ANS-X distance and the slight rotation of the mandible in conjunction with uprighting of the mandibular incisors counteracted the change for overbite in our study, in contrast to the results of the studies showing a decrease in overbite.39,40
Class III patients have an unfavorable facial appearance, which may affect their psychological status. Therefore, the improvement of facial esthetics is an important factor in patients' psychosocial development. In our study, forward movement of the maxilla, associated with slight mandibular rotation, resulted in a reduction of profile concavity, in accordance with the results of studies15–21 conducted using rigid anchorage. The soft tissue effects were more marked for the upper lip and soft tissue pogonion than for the lower lip. Forward movement of the upper lip resulted from maxillary protraction without maxillary incisor proclination. Lower lip position did not change after treatment, as in the study of Cozza et al.43 However, Ngan et al.44 observed changes in soft tissue profile accompanied by forward movement of the upper lip and backward movement of the lower lip.
Clinicians should be aware that problems, such as infection due to poor oral hygiene, loosening of miniplates as a result of applying torsional forces, and soft tissue irritation due to unfavorable bending of the distal extension of the miniplate, may arise after the insertion of miniplates. Facemask treatment anchored with miniplates after use of the Alt-RAMEC protocol can offer an advantage for correcting mild/moderate maxillary retrusion; its treatment effect on the maxilla is orthopedic. However, further studies with larger study groups are required to evaluate the long-term effects of such treatment.
CONCLUSIONS
Facemask treatment anchored with miniplates after use of the Alt-RAMEC protocol resulted in the following:
Significant forward movement of the maxilla, with a slight counterclockwise rotation and without maxillary incisor proclination;
Significant clockwise rotation of the mandible, with slight uprighting of the mandibular incisors;
Statistically significant increase in vertical dimension;
Significant improvement in soft tissue profile, with significant forward movement of the upper lip and backward movement of the soft tissue pogonion.
REFERENCES
- 1.Delaire J. Maxillary growth: therapeutic conclusions. Trans Eur Orthod Soc. 1971:81–102. [PubMed] [Google Scholar]
- 2.Petit H. Adaptation following accelerated facial mask therapy. In: McNamara J. A Jr, Ribbens K. A, Howe R. P, editors. Clinical Alteration of the Growing Face Monograph No 14 Craniofacial Growth Series. Ann Arbor, Mich: University of Michigan; 1983. Center for Human Growth and Development. [Google Scholar]
- 3.Mermigos J, Full C. A, Andreasen G. Protraction of the maxillofacial complex. Am J Orthod Dentofacial Orthop. 1990;98:47–55. doi: 10.1016/0889-5406(90)70031-7. [DOI] [PubMed] [Google Scholar]
- 4.Kambara T. Dentofacial changes produced by extraoral forward force in the Macaca irus. Am J Orthod. 1977;71:249–277. doi: 10.1016/0002-9416(77)90187-7. [DOI] [PubMed] [Google Scholar]
- 5.Tanne K, Sakuda M. Biomechanical and clinical changes of the craniofacial complex from orthopedic maxillary protraction. Angle Orthod. 1991;61:145–152. doi: 10.1043/0003-3219(1991)061<0145:BACCOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Haas A. J. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Haas A. J. Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod. 1970;57:219–255. doi: 10.1016/0002-9416(70)90241-1. [DOI] [PubMed] [Google Scholar]
- 8.Liou E. J. Effective maxillary orthopedic protraction for growing Class III patients: a clinical application simulates distraction osteogenesis. Prog Orthod. 2005;6:154–171. [PubMed] [Google Scholar]
- 9.Liou E. J. Toothborne orthopedic maxillary protraction in Class III patients. J Clin Orthod. 2005;39:68–75. [PubMed] [Google Scholar]
- 10.Liou E. J, Tsai W. C. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005;42:121–127. doi: 10.1597/03-107.1. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y. C, Chang P. M. S, Liou E. J. W. Opening of circummaxillary sutures by alternate rapid maxillary expansions and constrictions. Angle Orthod. 2009;79:230–234. doi: 10.2319/031208-141.1. [DOI] [PubMed] [Google Scholar]
- 12.Nartallo-Turley P. E, Turley P. K. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998;68:217–224. doi: 10.1043/0003-3219(1998)068<0217:CEOCPE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.da Silva Filho O. G, Magro A. C, Capelozza Filho L. Early treatment of the Class III malocclusion with rapid maxillary expansion and maxillary protraction. Am J Orthod Dentofacial Orthop. 1998;113:196–203. doi: 10.1016/s0889-5406(98)70292-6. [DOI] [PubMed] [Google Scholar]
- 14.Vaughn G. A, Mason B, Moon H. B, Turley P. K. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005;128:299–309. doi: 10.1016/j.ajodo.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 15.Singer S. L, Henry P. J, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003;123:571–577. doi: 10.1067/mod.2003.S0889540603000520. [DOI] [PubMed] [Google Scholar]
- 17.Hong H, Ngan P, Han G, Qi L. G, Wei S. H. Use of onplants as stable anchorage for facemask treatment: a case report. Angle Orthod. 2005;75:453–460. doi: 10.1043/0003-3219(2005)75[453:UOOASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Kircelli B. H, Pektas Z. O. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Kircelli B. H, Pektas Z. O, Uckan S. Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Angle Orthod. 2006;76:156–163. doi: 10.1043/0003-3219(2006)076[0156:OPWSAI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.De Clerk H. J, Cornelis M. A, Cevidanes L. H, Heymann G. C, Tulloch C. J. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67:2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baek S. H, Kim K. W, Choi J. Y. New treatment modality for maxillary hypoplasia in cleft patients. Angle Orthod. 2010;80:783–791. doi: 10.2319/073009-435.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greulich W. W, Pyle S. I. Radiographic Atlas of Skeletal Development of the Hand and Wrist 2nd ed. Palo Alto, Calif: Stanford University Press; 1959. [Google Scholar]
- 23.Erverdi N, Usumez S, Solak A. New generation open-bite treatment with zygomatic anchorage. Angle Orthod. 2006;76:519–526. doi: 10.1043/0003-3219(2006)076[0519:NGOTWZ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Delaire J. Maxillary development revisited: relevance to the orthopaedic treatment of Class III malocclusions. Eur J Orthod. 1997;19:289–311. doi: 10.1093/ejo/19.3.289. [DOI] [PubMed] [Google Scholar]
- 25.Hickham J. H. Maxillary protraction therapy: diagnosis and treatment. J Clin Orthod. 1991;25:102–113. [PubMed] [Google Scholar]
- 26.Franchi L, Baccetti T, McNamara J. A., Jr Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 27.Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod. 1982;82:329–342. doi: 10.1016/0002-9416(82)90467-5. [DOI] [PubMed] [Google Scholar]
- 28.Jackson G. W, Kokich V. G, Shapiro P. A. Experimental and postexperimental response to anteriorly directed extraoral force in young Macaca nemestrina. Am J Orthod. 1979;75:318–333. doi: 10.1016/0002-9416(79)90278-1. [DOI] [PubMed] [Google Scholar]
- 29.Haas A. J. Long-term posttreatment evaluation of rapid palatal expansion. Angle Orthod. 1980;50:189–217. doi: 10.1043/0003-3219(1980)050<0189:LPEORP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Haas A. J. The non-surgical treatment of the skeletal Class III. Book of Abstract American Association of Orthodontists. In. 100th Annual Session; Chicago, Ill, April 29–May 3, 2000:85. [Google Scholar]
- 31.Kokich V. G, Shapiro P. A, Oswald R, Koskinen-Moffett L, Clarren S. K. Ankylosed teeth as abutments for maxillary protraction: a case report. Am J Orthod. 1985;88:303–307. doi: 10.1016/0002-9416(85)90129-0. [DOI] [PubMed] [Google Scholar]
- 32.Burstone C. J, Marcotte M. R. Skeletal changes. In: Burstone C. J, Marcotte M. R, editors. Problem Solving in Orthodontics GoalOriented Treatment Strategies. Chicago, IL: Quintessence; 2006:26. [Google Scholar]
- 33.Baik H. S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 34.Gautam P, Valiathan A, Adhikari R. Skeletal response to maxillary protraction with and without maxillary expansion: a finite element study. Am J Orthod Dentofacial Orthop. 2009;135:723–728. doi: 10.1016/j.ajodo.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 35.Tanne K, Hiraga J, Kakiuchi K, Yamagata Y, Sakuda M. Biomechanical effect of anteriorly directed extraoral forces on the craniofacial complex: a study using the finite element method. Am J Orthod Dentofacial Orthop. 1989;95:200–207. doi: 10.1016/0889-5406(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 36.Tanne K, Hiraga J, Sakuda M. Effects of directions of maxillary protraction forces on biomechanical changes in craniofacial complex. Eur J Orthod. 1989;11:382–391. doi: 10.1093/oxfordjournals.ejo.a036010. [DOI] [PubMed] [Google Scholar]
- 37.MacDonald K. E, Kapust A. J, Turley P. K. Cephalometric changes after the correction of Class III malocclusion with maxillary expansion/facemask therapy. Am J Orthod Dentofacial Orthop. 1999;116:13–24. doi: 10.1016/S0889-5406(99)70298-2. [DOI] [PubMed] [Google Scholar]
- 38.Baccetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 39.Ngan P, Yiu C, Hu A, Hägg U, Wei S. H, Gunel E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur J Orthod. 1998;20:237–254. doi: 10.1093/ejo/20.3.237. [DOI] [PubMed] [Google Scholar]
- 40.Yuksel S, Ucem T. T, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23:559–568. doi: 10.1093/ejo/23.5.559. [DOI] [PubMed] [Google Scholar]
- 41.Kama J. D, Ozer T, Baran S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur J Orthod. 2006;28:496–502. doi: 10.1093/ejo/cjl011. [DOI] [PubMed] [Google Scholar]
- 42.Westwood P. V, McNamara J. A, Jr, Baccetti T, Franchi L, Sarver D. M. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306–320. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 43.Cozza P, Marino A, Mucedero M. An orthopaedic approach to the treatment of Class III malocclusions in the early mixed dentition. Eur J Orthod. 2004;26:191–199. doi: 10.1093/ejo/26.2.191. [DOI] [PubMed] [Google Scholar]
- 44.Ngan P, Hägg U, Yiu C, Merwin D, Wei S. H. Soft tissue and dentoskeletal profile changes associated with maxillary expansion and protraction headgear treatment. Am J Orthod Dentofacial Orthop. 1996;109:38–49. doi: 10.1016/s0889-5406(96)70161-0. [DOI] [PubMed] [Google Scholar]