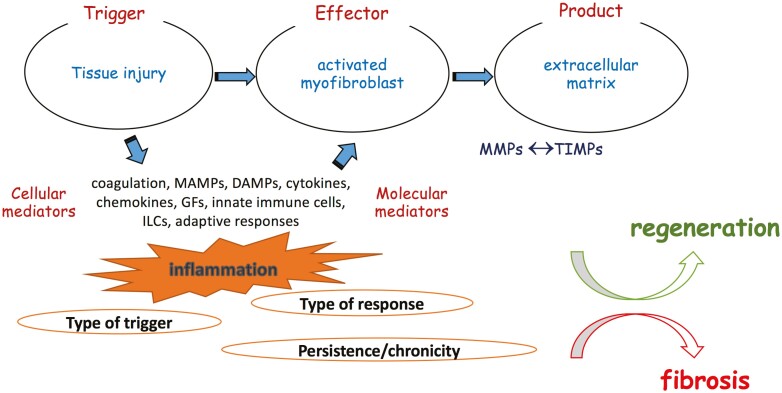
Figure 1.
Immunopathogenesis of intestinal response to injury. The intestinal mucosa is continuously exposed to a variety of potential harmful factors both of external (eg, infections, drugs, environmental toxins) and internal (eg, genetic, inflammatory, autoimmune) origin. The initial injury inflicted by such triggers create a breach in mucosal integrity, which allows entry of bacterial elements in deeper intestinal layers, releases various products of damaged host cells, and activates the coagulation pathway. The end product is a strong local and systemic inflammatory response that is executed via a rich network of cellular and molecular mediators, including cytokines, chemokines, and various constituents of the innate and adaptive arms of immunity. This original inflammatory response induces the enrichment of the local environment with the central cellular effector of fibrogenesis, the activated myofibroblast. Although the origin of myofibroblasts in intestinal fibrosis is still unrevealed, there are several potential sources, such as local fibroblasts and pericytes, circulating fibrocytes, as well as input by epithelial-to-mesenchymal and endothelial-to mesenchymal transition. Once activated, myofibroblasts become potent producers of ECM, which consists of collagens, fibronectin, and several other substances that occupy the intercellular space. This is a tightly regulated dynamic process encompassing a delicate balance between ECM degrading matrix metalloproteinases and their inhibitors. The final outcome is dictated by the type of the initial trigger and the ensuing response and, most importantly, by the transient or persistent nature of myofibroblast-activating stimuli. During homeostatic conditions, repair mechanisms lead to complete tissue regeneration and reestablish the structural integrity of the intestinal wall. In contrast, the chronic persistent inflammation that takes place in IBD constantly fuels profibrotic mechanisms, leading to tissue scarring and resulting in anatomical and functional compromise of the affected areas of the GI tract. Abbreviations: DAMP, damage-associated molecular patterns; ECM, extracellular matrix; IBD, inflammatory bowel disease; MMPs, matrix metalloproteinases; PAMP, pathogen-associated molecular pattern; TIMPs, tissue inhibitors of metalloproteinases.