Abstract
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a highly transmissible pathogenic coronavirus emerged in late 2019 causing a pandemic of acute respiratory disease, named ‘coronavirus disease 2019’ (COVID-19). It has spread fast all over the world posing an extraordinary threat to global public health. Along with SARS-CoV-2, there are seven human coronaviruses. Those causing mild diseases are the 229E, OC43, NL63 and HKU1, and the pathogenic ones are SARSCoV, MERS-CoV and SARS-CoV-2.
Objective
This review has highlighted the basic virology of SARS CoV-2 including its origin, structure, genomic characteristics, pathogenesis, immunological response and clinical manifestation along with the key difference of SARS CoV2 from the previous Coronaviruses.
Content
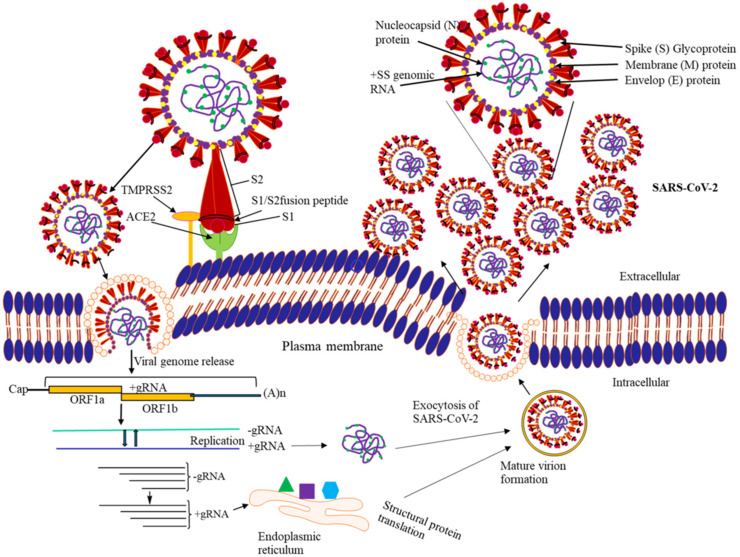
Coronaviruses are spherical and enveloped with club-shaped spikes on the surface. It has a large positive sense, single stranded RNA genome within the nucleocapsid with a helical symmetry. It has been known to cause infection to innumerable mammalian hosts, like humans, cats, bats, civets, dogs, and camels. The viral genome contains four major structural proteins: the spike (S), membrane (M), envelope (E) and the nucleocapsid (N) protein encoded within the 3’ end of the genome. Virus binds to the host cell by the S protein with specific receptor. Following receptor binding, the virus enters host cell cytosol and there is fusion of the viral and cellular membranes followed by the translation of the viral genomic RNA. Following the viral replication and sub-genomic RNA synthesis, there is formation of the mature virus. The virions are then transported to the cell surface in vesicles and are released by exocytosis.
Keywords: SARS CoV-2, COVID 19, Virology
1. Introduction
An outbreak of unusual viral pneumonia emerged in Wuhan, China, at the end of 2019, caused by a novel coronavirus designated as severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2). Being highly transmissible, coronavirus disease 2019 (COVID-19) has spread fast all over the world posing an extraordinary threat to global public health [1].
Coronaviruses, ubiquitous recognized pathogens of humans and animals were isolated as a causative agent of bronchitis in birds in 1937 [2]. During extensive research, six coronaviruses were identified causing respiratory diseases. HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1 reported to be less pathogenic compared to SARS-CoV and MERS-CoV, considered to be highly pathogenic to humans causing severe pneumonia with fatal outcome [3].
2. Spill over events leading to emergence of coronavirus events
Corona viruses are considered to be zoonotic pathogens. Those causing epidemics were believed to be originated from bats and transmitted to humans through an intermediate animal host with a likelihood of the spill over from animals to humans [4]. Chinese researchers proposed a hypothesis of pangolins a long-snouted, ant-eating mammals (used in traditional Chinese medicine) as animal source of the COVID-19 outbreak [5]. SARS-CoV-2 having higher reproductive number (R0) and more efficient spreading capacity, is considered to be more infectious than SARS CoV1. Both interact differently with the angiotensin-converting enzyme 2 (ACE 2) receptor. Different surface protein in SARS CoV2 allows its stronger binding to the ACE 2 receptor of host cell and greater efficiency at invading host cells [6]. It has a stronger bonding with upper respiratory tract (URT) and conjunctiva infecting more efficiently the URT and airways [7]. SARS-CoV-2 has highest viral load in URT at the time of onset of symptoms and during first week of illness compared to second week in SARS CoV1, indicating its highest infectiousness potential just before or within the first five days of symptom onset [8].
3. Classification of human corona viruses
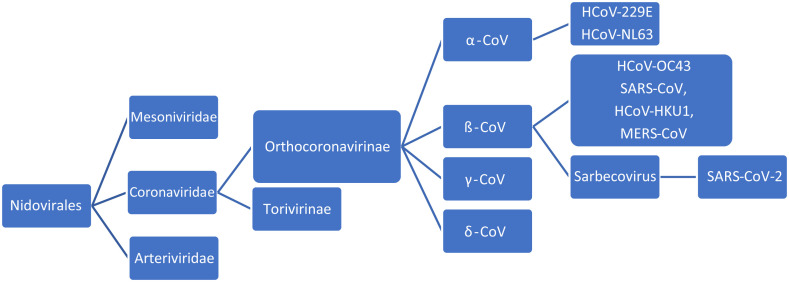
Coronaviruses are spherical viruses with club-shape spikes projecting from the surface, giving a solar corona appearance. The helically symmetrical nucleocapsids, with a positive-sense RNA genome lying within the envelope makes them having the largest genome for RNA viruses. The SARS-CoV-2 belongs to order Nidovirales, family Coronaviridae, subfamily Orthocoronavirinae, genus Betacoronavirinae and subgenus Sarbecovirus (Fig. 1 ). Genetic recombination within members of same or different genera leads to increased genetic diversity, causing spill over to other species and result in the emergence of novel viruses [9].
Fig: 1.
Classification of human coronaviruses.
4. Virology of Coronaviruses
Coronaviruses have a spike glycoprotein layer, constituting two subunits S1 and S2. S1 mediates adhesion of virus with host cell and the S2 helps its fusion to host cell membrane. Genetic modification of glycoprotein layer could potentially affect the virulence of the virus [10] as explored in pangolin coronaviruses where the furin-like cleavage sites S1/S2 in the S protein was deficient making it different and suggesting increased transmission rate among humans [11]. It also consists of structural proteins, integral membrane proteins, small membrane protein, (M and E proteins) and the Nucleocapsid Protein (N). The genes coding for this protein (S, E and N) can be identified by Nucleic Acid Amplification based diagnostic test. SARS-CoV2 has a phylogenetically different RNA-dependent RNA polymerase (RdRp) gene and proteins like 3- chymotrypsin-like protease, papain-like protease, and others exerting its virulent impact [12].
5. Genomic organization of SARS CoV2
The RNA genome (27–32 kbp) has six open reading frames (ORFs). The first open reading frame ORF1a/b (about two-thirds of the whole genome) at the 5’ end encodes the non-structural proteins (nsp) polyprotein1a, b (pp1a, pp1b) [13]. The pp1a corresponds to NSP1 to NSP11 and pp1ab comprises of NSP12 to NSP16.
The ORFs located on 3’ end encodes four structural proteins: envelop glycoprotein spike S (recognizes host cell receptors) [14], Membrane (M) proteins (shapes the virions and envelope), E proteins (virions assembly and release) and nucleocapsid protein(N) for packaging of the RNA genome and pathogenicity of the virus as an interferon (IFN) inhibitor. In addition, species-specific ORF3a, ORF3d, ORF6, ORF7a, ORF7b, ORF8, ORF9b, ORF14, and ORF10 genes encode nine accessory proteins [15].
Two distinct domains, leader sequence and untranslated region (UTR) near the 5'end form multitude of stem loop structures required for replication and transcription of viral genome. Each structural and accessory gene is preceded by transcriptional regulatory sequences (TRSs), a prerequisite for their functional expression. Structural component of 3′UTR is required for viral RNA replication [14].
On viral entry to target cell cytoplasm, the RNA genome translates into pp1a and pp1b further processing into 16 non-structural proteins (NSPs), forms a replication-transcription complex (RTC) for genomic transcription and replication, resulting in a nested set of sub-genomic RNAs (sgRNAs) synthesized by RTC as discontinuous transcription (Fig. 2 ) [16].
Fig. 2.
Genomic arrangement of SARS-CoV-2 showing sequential arrangement of various non-structural, structural and accessory genes [14].
6. Major proteins and its Functions
S protein (∼150 kDa) mediates attachment, fusion and subsequent entry of virus to host cell, facilitates infected and uninfected cell-cell fusion forming multinucleated giant cells, a strategy allowing direct spread of virus between cells to avoid virus neutralising antibodies. A host cell furin-like protease cleaves the S protein into S1 and S2. S1 makes up the large receptor-binding domain and S2 forms the stalk of the spike [17].
M protein (∼25–30 kDa), the most abundant one has three transmembrane domains defining shape of the viral envelope [14]. S and M protein interaction is essential for retention of S in the ER-Golgi intermediate compartment (ERGIC)/Golgi complex and its incorporation into new virions. M protein and N protein binding stabilises the nucleocapsid (N protein-RNA complex) and internal core of virions, completing the viral assembly. M and E proteins making the viral envelope helps in production and release of virus-like particles (VLPs) [14,15].
E protein (∼8–12 kDa), the smallest of all is abundantly expressed inside the infected cell. It is incorporated into the virus envelope and participates in viral assembly and budding. Recombinant CoVs without E protein result in significantly reduced viral titres, crippled viral maturation, or yield incompetent progeny, indicating importance of E protein in virus production and maturation. The N protein is involved in viral assembly, budding and complete virion formation [15].
7. Physical and Chemical Properties of SARS COV2
Physical agents including pH, temperature, and relative humidity can significantly affect endemic human corona viruses. Extreme pH inactivates them rapidly; however, they are stable at pH 6–6.5. SARS-CoV can be inactivated at a temperature of 56 °C exposed for 30 min, but presence of protein needs higher temperature. Viruses dried on smooth surfaces at temperatures of 22°C–25 °C and a relative humidity of 40–50% remains infectious for over 5 days, but infectivity is lost at higher temperatures of 38 °C and relative humidity of >95%. Chan et al. suggested that at air-conditioned room temperatures and low humidity the stability of SARS-CoV is maintained, facilitating cross contamination and virus transmission at home, workplaces and public institutions. Viruses may be inactivated in tropical areas with high ambient temperatures and relative humidity reducing their transmission and spread [18]. In a study in the New England Journal of Medicine, SARS-CoV-2 was found to be more stable on plastic and stainless steel than on copper. It was found to survive for 72, 8–24 and 4–8 h on plastic/stainless steel, cardboard and copper surfaces, respectively [19].
Coronaviruses are susceptible to chemical agents and disinfectants like ether, chloroform, ethanol, propanol, glutaraldehyde, formaldehyde etc. Kampf et al. found that SARS-CoV, MERS-CoV and endemic human coronaviruses can survive on metal, glass, or plastic for up to 9 days and inactivated easily by 62–71% ethanol, 0.5% hydrogen peroxide, or 0.1% hypochlorite within 60 s [20]. Sattar et al. found that hexamidine, chlorhexidine and cetrimide were ineffective against HCoV 229E, and chlorhexidine and cetrimide acquired virucidal properties with addition of alcohol. [21]. According to Kraztel et al. ethanol, isopropanol and WHO recommended hand rub formulations could effectively inactivate SARS-CoV 1&2 [22].
8. Biology of SARS CoV 2 virus multiplication
Replication of coronaviruses is considered to be very complex and begins with binding of the virus to a host cell through its target receptor. The receptor binding domain of the S1 sub-unit binds to the peptidase domain of angiotensin-converting enzyme ACE 2 [23]. Viral entry is followed by the uncoating of the viral genomic RNA. The RNA genomic template is translated to generate an RNA-dependent RNA polymerase, followed by a full-length negative strand template synthesis. A nested set of 5–7 sub genomic mRNAs having common 5′ leader and 3′ terminal sequences and a full-length genomic RNA is generated by a discontinuous transcription mechanism using negative strand template. Unique sequences at the 5’ end of mRNAs is translated to non-structural proteins and structural proteins. The helical nucleocapsids formed by assembly of newly synthesized genomic RNA molecules, the nucleoproteins within the cytoplasm bud through the membranes of the endoplasmic reticulum containing viral glycoproteins, followed by the transport of matured virions in vesicles and their release through fusion with plasma membrane [14] (Fig. 3 ).
Fig. 3.
Viral Multiplication.
9. Pathogenesis, clinical features and immune response
Distribution of ACE 2 receptors in different tissues explains the sites of infection and patient symptoms. Non-specific symptoms like fever, myalgia, headache, and respiratory symptoms occurs due to active multiplication of the virus in the lung cells [6]. It causes transient damage to the olfactory epithelium causing olfactory dysfunction and temporary loss of taste and smell sensations [23]. ACE 2 receptors found on intestine and kidney epithelium and endothelium, explains the gastrointestinal and cardiovascular complications. Lymphocytic endothelitis, hepatic necrosis and myocardial infarction observed in post-mortem examination of lung, heart, kidney, and liver of patients died of covid-19 indicates direct effect on many organs [24]. Pathological changes in the respiratory tract or endothelial dysfunction might be due to direct viral infection, cytokine dysregulation, coagulopathy, or they are multifactorial, and or the viral invasion or coagulopathy might directly contribute to some of the ischaemic complications [25].
A marked decrease in B-lymphocytes, T-lymphocytes, natural killer (NK) cells and a decrease in CD4+ T-cells with relative increase in CD8+ T-cells, is seen due to direct viral invasion. A stormy response of the immune system evoked by the destruction of these lymphocytes is represented by a spurt of cytokines, interleukin-6 (IL-6), inflammatory markers such as C-reactive protein (CRP) with increase production of fibrinogen and hypercoagulable state [26].
Multiple thrombi formation induced by hypercoagulable state in lungs and coronaries leads to increase morbidity. Lower immunological state along with cytokine storms may cause severe pneumonia and extensive inflammatory responses with destruction of type II pneumocytes causing acute respiratory distress syndrome (ARDS) [27]. Multiple factors including the trigger due to pulmonary and peripheral endothelial cell injury contribute to the coagulation disorder. Dysfunctional coagulation potentiating aggressive immune reaction and persistent inflammatory process triggers the coagulation cascade. An increased in IL-6 could activate the coagulation process and suppress the fibrinolytic system, Hypercoagulable state (evidenced by an elevated levels of fibrinogen and D-dimer, prolonged prothrombin time, and near normal activated partial thromboplastin time) could lead to multiple blood thrombi and disseminated intravascular coagulation (DIC) worsening ARDS, and might lead to sudden cardiac death [28].
SARS-CoV-2 provokes an unusual host immune response evidenced by post-mortem histology of lung tissues with features of bilateral diffuse alveolar damage, hyaline-membrane formation, interstitial mononuclear inflammatory infiltrates, and desquamation consistent with ARDS [29,30]. Overproduction and accumulation of pro-inflammatory cytokines, eventually damaging the lung parenchyma is a distinguishing feature of covid-19 with presence of mucus plugs and fibrinous exudate in the respiratory tract explaining its severity even in young adults [29]. The ACE2-carrying cells of vascular endothelium, respiratory epithelium, alveolar monocytes, renal tubular cells and macrophages might also be invaded causing multi-organ failure and septic shock in SARS CoV 2 infection [31]. Involvement of cardiovascular system is reflected by release of highly sensitive troponin and natriuretic peptides [32]. Cytokines normally regulating immunity, inflammation and haematopoiesis; but their accumulation in different organs may cause extensive tissue damage, or a cytokine release syndrome (cytokine storm), subsequently leading to capillary leak, thrombus formation, and organ dysfunction [30]. Studies suggests a correlation between viral dynamics, the severity of illness, and disease outcome and between severity of illness, viral load, and IFN- α, IFN-γ, and TNF-α response has also been established [33].
10. SARS-CoV-2 variants
In later parts of 2020 various variants of SARS- CoV2 have emerged posing high risk to global public health. These variants are Variants of Interest (VOIs) and Variants of Concern (VOCs) so as to prioritise global monitoring and research [34].
11. Variants of Interest (VOIs)
They have specific genetic markers that affect the viral transmissibility, virulence, reduction in neutralization by antibodies obtained through natural infection or vaccination, the ability to evade detection, or a decrease in the effectiveness of therapeutics or vaccination. Various VOIs are Epsilon (B.1.427 and B.1.429); Zeta (P.2); Eta (B.1.525); Theta (P.3); Iota (B.1.526); Kappa (B.1.617.1), Lambda (C.37) and mu (B.1.621).
12. Variants of Concern (VOCs)
They have similar properties like VOI with a potential of enhanced transmissibility. Various VOCs are.
Alpha (B.1.1.7 lineage): Reported in the UK, has17 mutations (8 mutations in Spike protein-Δ69-70 deletion, Δ144 deletion, N501Y, A570D, P681H, T716I, S982A, D1118H) in the viral genome. N501Y mutation in the spike protein shows an increased affinity of the protein to ACE 2 receptors [35,36].
Beta (B.1.351 lineage or GH501Y·V2): First detected in South Africa in October 2020 and was responsible for the second wave of COVID-19 infections. Nine mutations (L18F, D80A, D215G, R246I, K417 N, E484K, N501Y, D614G, andA701V) in the spike protein, three mutations (K417 N, E484K, and N501Y) located in the receptor binding domain (RBD) increase the binding affinity for the ACE receptors [37].
Gamma (P.1 lineage or GR/501Y·V3): identified in December 2020 in Brazil and has ten spike mutations (L18F, T20 N, P26S, D138Y, R190S, H655Y, T1027IV1176, K417T, E484K, and N501Y) with three mutations (L18F, K417 N, E484K) in the RBD.
Delta (B.1.617.2 lineage): Initially identified in December 2020 in India was responsible for the deadly second wave of COVID-19. It harbours ten mutations (T19R, (G142D∗), 156del, 157del, R158G, L452R, T478K, D614G, P681R, D950N) in the spike protein [34,38]. Its sub lineage assigned as AY.1 (Delta Plus) detected in India has an additional mutation(K417N) in RBD. [39].
Omicron (B.1.1.529): First reported from South Africa in November 2021 and spread worldwide becoming the most dominant variant including that in India. It possesses at least 50 mutations, with 30 in the S gene. It has high transmissibility with S gene escape in RTPCR diagnostic kits [34,38].
13. Conclusion
Many aspects of virus biology, SARS-CoV-2, a novel virus have been unravelled within a short time by the researchers. Due to great attribute to technology and the competence of virologist, cell biologists, immunologists, epidemiologists and pharmacologists lead to much known facts about the virus as compared to the disease. It provided a great opportunity for collaboration inter-sector, interdisciplinary in medicine, biology, and in chemistry. Technological and methodological advances in the field of virology, molecular biology, and pharmacology have helped in understanding the structural and genomic organization, lifecycle, and pathophysiological characteristics of SARS-CoV-2. There is still a need of cellular and animal models for SARS-CoV-2 to better understand the mechanisms underlying viral replication, pathogenesis, and transmission dynamics and therapeutics.
Declaration of competing interest
There is no conflict of interest.
References
- 1.Hu B., Guo H., Zhou P., Shi Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19(3):141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang W., Lin X.D., Guo W.P., et al. Discovery, diversity and evolution of novel coronaviruses sampled from rodents in China. Virology. 2015;474:19–27. doi: 10.1016/j.virol.2014.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samudrala P.K., Kumar P., Choudhary K., Thakur N., Wadekar G.S., Dayaramani R., et al. Virology, pathogenesis, diagnosis and in-line treatment of COVID-19. Eur J Pharmacol. 2020;883:173375. doi: 10.1016/j.ejphar.2020.173375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ge X.-Y., Li J., Yang X., Chmura A., Zhu G., Epstein J.H., Mazet J.K., Hu B., Zhang W., Peng C., et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 2013;503:535–538. doi: 10.1038/nature12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang T., Wu Q., Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr Biol. 2020;30:1346–1351.e2. doi: 10.1016/j.cub.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cevik M., Bamford C.G.G., Ho A. COVID-19 pandemic-a focused review for clinicians. Clin Microbiol Infect. 2020;26:842–847. doi: 10.1016/j.cmi.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wölfel R., Corman V.M., Guggemos W., et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 8.Cevik M., Tate M., Lloyd O., et al. SARS-CoV-2, SARS-CoV-1 and MERS-CoV viral load dynamics, duration of viral shedding and infectiousness: a living systematic review and meta-analysis. Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loomba P., Wattal C., Chakravarti A., Dutta S., Chabbra M., Kale P., et al. Can the march of COVID-19 be halted. Indian J Med Microbiol. 2020;38(1):128–133. doi: 10.4103/ijmm.IJMM_20_178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91-8. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lam T.T., Jia N., Zhang Y.W., Shum M.H., Jiang J.F., Zhu H.C., et al. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature. 2020;583:282–285. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee I., Mohabeer P., Shukla A., Kashyap A., Robinson J. COVID-19: recent advances in epidemiology, virology, etiopathogenesis, clinical trials and vaccine development. J Biomed Sci. 2020;7(1):18–27. [Google Scholar]
- 13.Masters P.S. ume 66. Elsevier; Amsterdam, The Netherlands: 2006. pp. 193–292. (The molecular biology of coronaviruses). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yadav R., Chaudhary J.K., Jain N., Chaudhary P.K., Khanra S., Dhamija P., Sharma A., Kumar A., Handu S. Role of structural and non-structural proteins and therapeutic targets of SARS-CoV-2 for COVID-19. Cells. 2021;10:821. doi: 10.3390/cells10040821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fehr A.R., Perlman S. Coronaviruses. ume 1282. Springer; Berlin/Heidelberg, Germany: 2015. An overview of their replication and pathogenesis; pp. 1–23. (Therapeutic Antibodies). [Google Scholar]
- 16.Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418–424. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glowacka I., Bertram S., Müller M.A., et al. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J Virol. 2011;85(9):4122–4134. doi: 10.1128/JVI.02232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan K.H., Malik Peiris J.S., Lam S.Y., et al. The effects of temperature and relative humidity on the viability of SARS coronavirus. Adv Virol. 2011;20:734690–734697. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Doremalen N., Bushmaker T., Morris D.H., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sattar S.A., Springthorpe V.S., Karim Y., Loro P. Chemical disinfection of non-porous inanimate surfaces experimentally contaminated with four human pathogenic viruses. Epidemiol Infect. 1989;198(102):493–505. doi: 10.1017/s0950268800030211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kratzel A., Todt D., Vkovski D., et al. 2020. Efficient inactivation of SARS-CoV-2 by the World Health Organization (WHO) recommended handrub formulations and alcohols. [DOI] [Google Scholar]
- 23.Cevik M., Kuppalli K., Kindrachuk J., Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020;371:m3862. doi: 10.1136/bmj.m3862. [DOI] [PubMed] [Google Scholar]
- 24.Monteil V., Kwon H., Prado P., et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181:905–913. doi: 10.1016/j.cell.2020.04.004. e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varga Z., Flammer A.J., Steiger P., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5pmid:32325026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., et al. Clinical Infectious Diseases; 2020. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gibson P.G., Qin L., Puah S. COVID-19 ARDS: clinical features and differences to “usual” pre-COVID ARDS. Med J Aust. 2020;213(2):54–56.e1. doi: 10.5694/mja2.50674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao W., Li T. COVID-19: towards understanding of pathogenesis. Cell Res. 2020;28:1–3. doi: 10.1038/s41422-020-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mangalmurti N., Hunter C.A. Cytokine storms: understanding COVID-19. Immunity. 2020;53:19–25. doi: 10.1016/j.immuni.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blanco-Melo D., Nilsson-Payant B.E., Liu W.-C., et al. Imbalanced host response to SARS-CoV-2 drives development of covid-19. Cell. 2020;181:1036–1045.e9. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li S.R., Tang Z.J., Li Z.H., Liu X. Searching therapeutic strategy of new coronavirus pneumonia from angiotensin-converting enzyme 2: the target of COVID-19 and SARS-CoV. Eur J Clin Microbiol Infect Dis. 2020;39(6):1021–1026. doi: 10.1007/s10096-020-03883-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu P.P., Blet A., Smyth D., Li H. The science underlying covid-19: implications for the cardiovascular system. Circulation. 2020;142:68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 33.Cevik M., Tate M., Lloyd O., et al. SARS-CoV-2, SARS-CoV-1 and MERS-CoV viral load dynamics, duration of viral shedding and infectiousness: a living systematic review and meta-analysis. Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30172-5. [forthcoming)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO COVID-19 weekly epidemiological update . vol. 74. World Health organization; January 2022. [Google Scholar]
- 35.Galloway S.E., Paul P., MacCannell D.R., Johansson M.A., Brooks J.T., MacNeil A., et al. Emergence of SARS-CoV-2 B.1.1.7 lineage - United States, december 29, 2020-january 12,2021. MMWR Morb Mortal Wkly Rep. 2021 Jan 22;70(3):95–99. doi: 10.15585/mmwr.mm7003e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Volz E., Mishra S., Chand M., Barrett J.C., Johnson R., Geidelberg L., et al. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature. 2021;593(7858):266–269. doi: 10.1038/s41586-021-03470-x. [DOI] [PubMed] [Google Scholar]
- 37.Tegally H., Wilkinson E., Giovanetti M., Iranzadeh A., Fonseca V., Giandhari J., et al. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. 2021;592(7854):438–443. doi: 10.1038/s41586-021-03402-9. [DOI] [PubMed] [Google Scholar]
- 38.Cdcmmwr Sars-CoV-2 B.1.1.529 (omicron) variant — United States, december 1–8, 2021. MMWR Morb Mortal Wkly Rep. 2021:70. doi: 10.15585/mmwr.mm7050e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacob J.J., Fletcher G.J., Priya M., Balaji B., Mutreja A. Relevance of immune response and vaccination strategies of SARS-CoV-2 in the phase of viral red queen dynamics. Indian J Med Microbiol. 2021;39(4):417–422. doi: 10.1016/j.ijmmb.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]



![FigQ5: Two versions of caption have been provided for Fig. [2,3]. Please confirm that we have used the correct one.. 2](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/17e7/8919811/19954b3b7672/gr2_lrg.jpg)