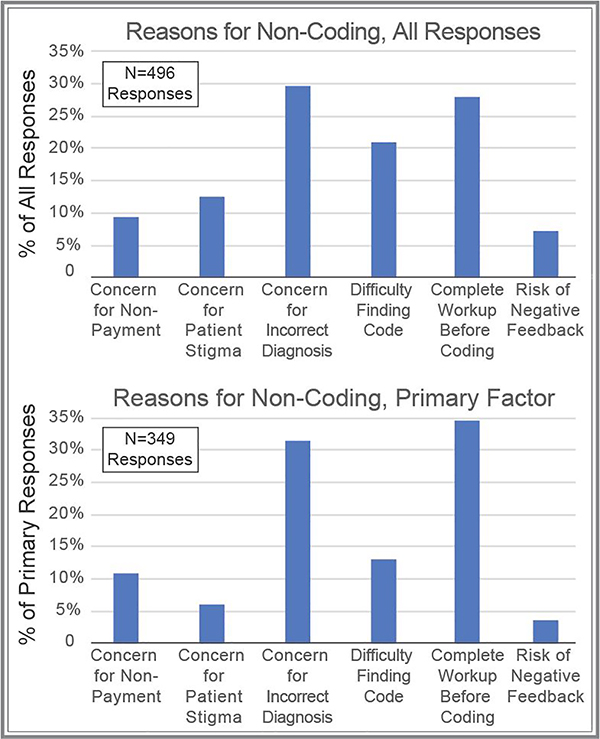
Figure 2 – Self-identified reasons for not utilizing FND-related diagnosis codes.
Neurologists were asked to recall a patient with suspected FND for which they did not utilize FND-related diagnosis codes. Respondents were asked to select all applicable reasons for not coding (could select none or multiple reasons, upper panel), and to also select the primary (most-important, lower panel) reason for not utilizing FND-related diagnostic codes. Potential responses included: concern for non-payment (insurance denial); concern that patient would be stigmatized by other healthcare providers; concern for the FND diagnosis being incorrect; difficulty finding the correct FND-related billing code; the practice style of only coding for symptoms, not underlying causes, until diagnostic testing is complete; concern about negative feedback from patient (including retaliation, bad reviews, or litigation).