Highlights
-
•
Poorer health outcomes are correlated with depression/anxiety in a rural population.
-
•
Electronic modes of recruitment engage those reporting depression/anxiety into CDSME.
-
•
CDSME increases patient activation regardless of history of depression/anxiety.
Keywords: Self-management, Mental health, Rural, Patient engagement, Evidence-based program
Abstract
Chronic disease self-management education (CDSME) programs benefit individuals with chronic diseases, including mental health conditions, by improving health-related outcomes and increasing engagement with the health care system. Recruiting individuals with a history of mental health conditions to participate in CDSME is challenging, particularly in rural, underserved areas. Hence, it is important to understand factors associated with the presence of mental health conditions, and impacts of CDSME on patient engagement. This project identifies individual and program-level characteristics, as well as recruitment characteristics, associated with reporting a history of depression and/or anxiety. It also assesses factors related to program engagement and the relationship between completing CDSME and patient activation. Data were collected during CDSME workshops offered in 2019 in a rural region of New York. Of the 421 enrollees who completed survey instruments, 162 reported a history of depression and/or anxiety. Univariate analyses indicated that those reporting a history of depression and/or anxiety were younger, female, in poorer health, had more comorbidities, were Medicaid beneficiaries, and had lower patient activation scores. They also heard about and signed up for the workshop through the internet at higher rates than those not reporting a history of depression and/or anxiety. Multivariable logistic regression modeling indicated age, self-rated health, and number of comorbidities were independent predictors of reporting a history of depression and/or anxiety. Among CDSME completers, patient activation significantly improved regardless of history of depression and/or anxiety. Engaging individuals with mental health conditions in CDSME requires a multimodal recruitment strategy incorporating electronic marketing and registration.
1. Introduction
The incidence and prevalence of chronic disease are well-recognized health concerns in the United States, with rural populations facing higher rates of chronic disease compared to their urban counterparts. (Matthews et al., 2017, Lee et al., 2021) Adults in rural and urban settings experience the same chronic conditions, but rural-residing adults have higher rates of conditions such as cardiovascular disease, arthritis, and chronic obstructive pulmonary disease. (Croft et al., 2018, Boring et al., 2017, Towne et al., 2019).
While prevalence of mental health conditions is not necessarily greater in rural areas, (Myers, Mar 2019, Crittenden and Kaye, 2021) the rate of death due to suicide and drug overdoses is higher in rural areas. (Case and Deaton, 2015, Diez Roux, Oct 2017) Rural counties have fewer mental health professionals, (Kirby et al., 2019, Summers-Gabr, Aug 2020) but even when resources are available, service utilization is lower in rural areas than in urban areas, (Crittenden and Kaye, 2021) particularly among older adults. While these lower utilization rates may be related to barriers such as lack of transportation and cost, (University of Minnesota Rural Health Research Center and NORC Walsh, 2019) they could also be attributed, in part, to a strong sense of self-reliance as well as a general lack of anonymity, both of which are prevalent within rural populations. (Lee et al., 2018).
It has become widely recognized that effective treatment of chronic disease, including mental health conditions such as depression and anxiety, involves consistent self-management. (Grady and Gough, Aug 2014) The paradox is that those with multiple chronic conditions are less likely to be able or willing to engage in self-management activities. (Jowsey et al., 2009) The Self-Management Resource Center’s suite of evidence-based programs, originally developed at Stanford University, has been extensively implemented in the US and internationally to support self-management efforts for those living with chronic disease, as well as for their care partners. The small group workshops, facilitated by trained peer leaders, are framed by social learning theory and focus on improving one’s self-efficacy in managing chronic illness. (Bandura, 1977, Lorig et al., 1999) These Chronic Disease Self-Management Education (CDMSE) programs have demonstrated effectiveness with a variety of health-related outcomes including depression and anxiety, (Lee et al., 2019, Lorig et al., Jan 2014, Lorig et al., 2016, Mehlsen et al., May 2015, Ory et al., 2013, Ritter et al., Dec 2014) but recruitment and retention remains challenging, particularly for some at-risk populations, such as those with multiple co-morbidities or a history of mental health conditions. (Lorig et al., Jan 2014, Fredericks et al., Nov 2012).
National efforts have examined the dissemination of chronic disease self-management education (CDSME) in rural areas. Generally, these studies report that rural areas, compared to urban areas, offer fewer types of self-management programs, deliver fewer workshops, and reach fewer participants. (Smith et al., 2017, Towne et al., 2015, Towne et al., 2015) However, rural residents tend to have higher program completion rates than their urban counterparts. (Ahn et al., 2014, Bobitt et al., 2019).
Implementing CDSME programs in rural areas is compounded by unique challenges that include cultural differences among residents, program scarcity, lack of awareness about program offerings, and transportation challenges. (Towne et al., 2015, Smith et al.,, Dattalo et al., Apr 2017, Horrell and Kneipp, 2017) Further, although these challenges to program implementation may be similar across rural communities, each rural community is unique in terms of its population characteristics and health service infrastructure. Despite being a goal of many programmatic initiatives, the low population density of rural communities makes serving these areas less financially viable and of lower priority compared to urban areas, which discourages investment in any sort of preventive health infrastructure. (Ariel-Donges et al., 2019, Smith et al., 2017) In addition to the barriers associated with recruiting, engaging, and retaining participants in CDSME workshops in rural communities, less is known about the added complexities and barriers to engage participants with conditions such as depression or anxiety, which are accompanied by unique needs and self-regulating behavior.
Therefore, the purposes of this exploratory study were to: (1) describe the individual, workshop, and recruitment characteristics of CDSME programs delivered in a rural region, compared by whether or not participants reported a history of depression and/or anxiety; (2) identify the factors associated with engagement in CDSME programs for individuals reporting a history of depression and/or anxiety; and (3) determine if CDSME programs effectively increased patient activation for this at-risk population.
2. Methods
2.1. Setting and participants
We collected data for these analyses as part of a 3-year implementation phase of a regional self-management program in six counties of rural central New York. The region covers over 6000 square miles with limited access to urban centers or the Interstate system. Similar to many other rural areas in the northeast, the general population is largely non-Hispanic white and skews older (30% of the population is 60 or over).
This study utilizes data from the 39 in-person CDSME workshops offered in 2019. Participants enrolled in one of three workshops: chronic disease self-management program (CDSMP), diabetes self-management program (DSMP), or chronic pain self-management program (CPSMP). All of these evidence-based interventions are 6-week peer-led workshops that meet 2 ½ hours per week targeting adults with chronic conditions. Based on social learning theory, they were developed by the Stanford Patient Education Center and are now licensed through the Self-Management Resource Center. Activities such as dealing with difficult emotions, improving communication, relaxation techniques, problem solving and goal setting are common across all workshop types. Details on workshop content and processes have been described in more detail elsewhere and collectively have been demonstrated to increase self-efficacy in improving self-management practices. (LeFort et al., 1998, Lorig et al., 1999, Lorig et al., 2016) Caregivers were also welcome to attend, and our analyses included caregivers. There was no cost for individuals to attend the intervention, but they had to be able to physically travel to the community location where the program was offered. Participants were recruited from partnering organizations including rural health networks, primary care clinics and area offices for the aging. Multiple methods of recruitment were used including traditional print media (e.g. flyers, brochures), social media, provider referrals, targeted mailings, and electronic messaging through the patient electronic health portal.
Participants were asked to complete a baseline survey at the beginning of the first CDSME workshop session and a follow-up survey at the end of the sixth CDSME workshop session. Participants who completed the workshop (i.e., attended four out of six sessions) and both the baseline and follow-up surveys received a $30 gift card. This project was declared exempt from continuing review by the Mary Imogene Bassett Institutional Review Board.
2.2. Measures
Self-reported participant sociodemographic data such as sex, age, and education were collected at enrollment, which typically occurred when the participant showed up for the first class session. In addition, participants were asked to provide information about their self-rated general health, and types of chronic conditions. These questions aligned with the measures collected for the national study of CDSME. (Kulinski et al., 2014).
Specifically, participants were asked, “has a health care provider ever told you that you have any of the following conditions? Please mark all that apply” from a checklist of 16 conditions: Alzheimer’s or related dementia, arthritis/rheumatic disease, breathing/lung disease (e.g. asthma, COPD, emphysema, chronic bronchitis), cancer or cancer survivor, chronic pain, depression or anxiety disorders, diabetes, heart disease, high cholesterol, hypertension (high blood pressure), multiple sclerosis, osteoporosis (low bone density), pre-diabetes, stroke. If the person checked “depression or anxiety disorders,” that person was considered to have a history of depression and/or anxiety.
The Patient Activation Measure (PAM-10), licensed through Insignia Health, is a 10-item, 4-point scale (from “strongly agree” to “strongly disagree,” plus an option for N/A) that measures how activated a patient is to engage in their own care, a predictor of improved health outcomes. (Hibbard, 2017) A numerical score was generated via a proprietary algorithm (https://www.insigniahealth.com/products/pam-survey) with a possible range from 0 to 100, with higher scores indicating higher patient activation, a concept we are equating with patient engagement. All participants enrolled in 2019 workshops were invited to complete this instrument at baseline and post workshop.
We also collected various process measures including how participants heard about the program, how they signed up for the program, number of workshop sessions attended, travel distance between class and home, and reasons for not attending workshop sessions.
2.3. Statistical analyses
SAS version 9.4 (Cary, NC) was used for all analyses. Chi-squared (categorical) and independent t-tests (continuous) were used to compare characteristics of those reporting depression/anxiety with those who did not. Individual level variables included sex, age, education, number of chronic conditions, general health, insurance type, and baseline patient activation score. Workshop characteristics included workshop type, distance traveled to the workshop, and workshop completion status. Recruitment characteristics included how individuals heard about the workshop, and how they registered for the workshop. Cases were omitted from analyses if they had missing values for variables of interest. Data imputation for missing values was not conducted.
Variables associated with self-reported history of depression and/or anxiety at the univariate level (p < 0.05) were entered into a multivariable logistic regression model to identify independent predictors of depression and/or anxiety. The model included sex, age, number of chronic conditions, insurance status, self-reported health, PAM score, how individuals heard about the workshop, and how they registered for the workshop.
A sub-analysis was conducted among participants that completed the 6-week program to determine how patient activation (PAM) changed over time (pre- and post-workshop PAM scores were only available for participants completing the program). The paired t-test was used to compare pre-program versus post-program PAM scores. Two-way analysis of variance (ANOVA) was used to compare pre-post differences in PAM between those with and without self-reported history of anxiety/depression.
3. Results
3.1. Sample characteristics
In 2019, 421 individuals (72.2% female, mean age 63.6 years) enrolled in at least one CDSME workshop, of which 298 (70.8%) completed at least four out of the six sessions. Of enrolled participants, 38.5% reported being told they have depression and/or anxiety by a health care provider. Demographic characteristics for the full sample, as well characteristics based on a self-reported history of depression and/or anxiety can be found in Table 1.
Table 1.
Characteristics of Self-Management Program Enrollees by reported anxiety/depression (n = 421).
| Full Sample | No Anxiety/Depression n=259 | Yes Anxiety/Depression n=162 | p-value (yes vs no anxiety/depression) | |
|---|---|---|---|---|
| Individual Level Characteristics | ||||
| Sex | 0.014 | |||
| Female | 304 (72.2) | 176 (68.0) | 128 (79.0) | |
| Male | 117 (27.8) | 83 (32.0) | 34 (21.0) | |
| Age, mean (SD) | 63.6 (12.3) | 66.6 (11.6) | 59.0 (11.9) | <0.001 |
| Education | 0.128 | |||
| Less than HS | 23 (5.5) | 13 (5.1) | 10 (6.2) | |
| HS graduate/GED | 99 (23.7) | 65 (25.4) | 34 (21.1) | |
| Some college/technical school | 185 (44.4) | 103 (40.2) | 82 (50.9) | |
| College 4 or more years | 110 (26.4) | 75 (29.3) | 35 (21.7) | |
| Chronic conditions (SD) | 3.44 (1.96) | 3.14 (1.79) | 3.94 (2.10) | <0.001 |
| Self-reported health | <0.001 | |||
| Good/Very Good/Excllent | 255 (62.8) | 183 (73.2) | 72 (46.2) | |
| Fair/Poor | 151 (37.2) | 67 (26.8) | 84 (53.9) | |
| Insurance | <0.001 | |||
| Medicaid/Dual | 102 (24.2) | 45 (17.4) | 57 (35.2) | |
| Medicare | 200 (47.5) | 139 (53.7) | 61 (37.7) | |
| Other | 89 (21.1) | 55 (21.2) | 34 (21.0) | |
| Unknown | 30 (7.1) | 20 (7.7) | 10 (6.2) | |
| Baseline Patient Activation Measure (SD) | 64.2 (16.7) | 65.8 (18.0) | 61.7 (14.2) | 0.012 |
| Workshop Characteristics | ||||
| Workshop type | <0.001* | |||
| CDSMP | 80 (19.0) | 33 (12.7) | 47 (29.0) | |
| DSMP | 192 (45.6) | 143 (55.2) | 49 (30.3) | |
| CPSMP | 149 (35.4) | 83 (32.1) | 66 (40.7) | |
| Distance to workshop (miles) | 13.2 (10.0) | 13.6 (10.2) | 12.6 (9.8) | 0.344 |
| Completed workshop | 297 (70.6) | 184 (71.0) | 113 (69.8) | 0.778 |
| Recruitment Characteristics | ||||
| How heard about | ||||
| Healthcare Provider | 103 (24.5) | 60 (23.2) | 43 (26.5) | 0.433 |
| Friend/Family | 63 (15.0) | 47 (18.2) | 16 (9.9) | 0.021 |
| Healthcare network staff | 96 (22.8) | 66 (25.5) | 30 (18.5) | 0.098 |
| Previous workshop | 27 (6.4) | 16 (6.2) | 11 (6.8) | 0.803 |
| General print media | 114 (27.1) | 78 (30.1) | 36 (22.2) | 0.076 |
| General electronic media | 41 (9.7) | 16 (6.2) | 25 (15.4) | 0.002 |
| Other | 56 (13.7) | 32 (12.9) | 24 (15.0) | 0.537 |
| How signed up | 0.001 | |||
| Internet registration | 96 (23.1) | 44 (17.2) | 52 (32.5) | |
| Contacted Living Well | 141 (33.9) | 95 (37.1) | 46 (28.8) | |
| Living Well contacted | 94 (22.6) | 56 (21.9) | 38 (23.7) | |
| Other | 85 (20.4) | 61 (23.8) | 24 (15.0) | |
| Provider referral | 64 (15.2) | 35 (13.5) | 29 (17.9) | 0.223 |
*not included in modeling due to external funding factors determining which workshop type could be offered.
3.1.1. Individual level factors
In terms of individual characteristics, females were more likely to report a history of depression and/or anxiety (χ2 = 6.07, p =.014), as well as those who were younger (t = 6.40, p <.0001), and those who were Medicaid beneficiaries (χ2 = 18.77, p <.001). Those who reported depression and/or anxiety were also more likely to rate their health as fair or poor (χ2 = 30.08, p <.001) and have more chronic conditions (t = -4.02, p <.0001). Finally, those who reported a history of depression and/or anxiety also had significantly lower baseline patient activation (PAM) scores (t = 2.57, p =.011).
3.1.2. Workshop and recruitment level factors
Workshop type was the only workshop characteristic that differed between those reporting a history of depression and/or anxiety and those who did not. In addition, there were only two variables for recruitment strategies that were significantly different between the two groups. Compared to those not reporting a history of depression and/or anxiety, those with depression and/or anxiety were significantly more likely to hear about the program via social media (e.g., Facebook posts, Google ads) (χ2 = 9.71, p =.002) and register for the program on the website (χ2 = 15.94, p =.001). The association between hearing about the program via electronic means and history of self-reported depression and/or anxiety was similar for enrollees who were under age 65 (OR = 2.4, p = 0.07) versus age 65 and older (OR = 3.4, p = 0.02).
3.2. Independent predictors to self-reporting a history of depression and/or anxiety
The multivariable logistic regression (Table 2) included 362 individuals after 59 were omitted due to missing values for variables of interest (insurance coverage (n = 27), self-reported health (n = 12), age (n = 10), PAM (n = 5) and mechanism for signing up for the program (n = 5)).
Table 2.
Results of multivariable logistic regression for reporting a history of depression and/or anxiety (n = 362).
| Characteristics | Coefficient | Odds Ratio | 95% CI Lower Limit | 95% CI Upper Limit | p |
|---|---|---|---|---|---|
| Individual Level Characteristics | |||||
| Male | −0.5079 | 0.60 | 0.34 | 1.07 | 0.083 |
| Age | −0.0482 | 0.95 | 0.93 | 0.98 | <0.001 |
| Chronic Conditions | 0.3110 | 1.37 | 1.18 | 1.58 | <0.001 |
| Good/Very Good/Excellent self-reported health | 0.6402 | 0.53 | 0.31 | 0.89 | 0.017 |
| Medicaid/Dual | 0.6434 | 1.90 | 1.05 | 3.46 | 0.035 |
| Baseline Patient Activation | −0.0124 | 0.99 | 0.97 | 1.00 | 0.111 |
| Recruitment Level Characteristics | |||||
| Heard about | |||||
| Through general electronic media | 0.8855 | 2.42 | 0.99 | 6.01 | 0.056 |
| Signed up by | |||||
| Internet registration | 0.5463 | 1.73 | 0.88 | 3.40 | 0.113 |
| Living Well contacted | 0.0810 | 1.08 | 0.56 | 2.09 | 0.809 |
| Other | −0.1541 | 0.86 | 0.41 | 1.81 | 0.687 |
Age was significantly inversely associated with self-reported history of depression and/or anxiety. Those who self-rated their health as “good, very good, or excellent” also had significantly lower odds of reporting a history of depression and/or anxiety. Each additional chronic condition reported (beyond anxiety/depression) was associated with greater odds of reporting a history of depression and/or anxiety, as was insurance through Medicaid/dual versus other insurance carriers. Those who heard about the program via electronic means had 2.42 times higher odds of history of self-reported depression compared with those who heard about the program by all other means, but this association did not reach the threshold for statistical significance in the multivariable model (p = 0.056).
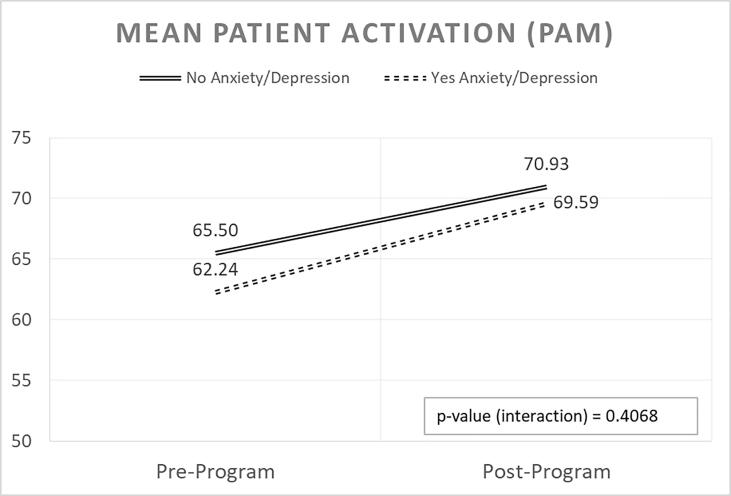
3.3. Change in patient activation
For the sub-analysis of those who completed the 6-week program, all completers taken together showed an increase in PAM by 6.2 points on average (p < 0.0001 by the paired t-test) from baseline to follow-up (Fig. 1). While both groups showed notable increases in patient activation (mean delta = 5.4 for those not reporting a history of depression and/or anxiety; mean delta = 7.4 for those who did report a history of depression and/or anxiety), these increases did not differ significantly between the two groups (p = 0.407 for the interaction of anxiety/depression by time via two-way ANOVA).
Fig. 1.
Mean patient activation (PAM) compared pre- and post-program among program completers reporting no history of anxiety and/or depression (n = 182) and those reporting history of anxiety and/or depression (n = 116).
4. Discussion
The objectives of these analyses were to describe the individual, workshop and recruitment characteristics of rural CDSME participants by self-reported history of depression and/or anxiety and to evaluate if CDSME effectively increases patient activation for this population. Similar to others’ studies, participants who were younger, Medicaid beneficiaries, reported poorer general health, and had more comorbidities were more likely to report a history of depression and/or anxiety. (Maneze et al., 2016, Braveman and Gottlieb, 2014, Faravelli et al., 2013)
Very few studies have evaluated the impact of CDSME on patient engagement using the Patient Activation Measure (PAM) since Hibbard et al.’s seminal work. (Hibbard et al., 2007) While those reporting a history of depression and anxiety had lower PAM scores at baseline, once self-rated health and Medicaid status were controlled for, the association disappeared, which indicates the complex relationship between poverty, poor health, and engagement. (Hardman et al., 2020) Our findings suggest those with a history of depression and/or anxiety could especially benefit from CDSME workshops not only to improve their ability to self-manage their chronic conditions, including behavioral health conditions (Ritter et al., 2014) but also to improve their patient activation, which has been shown to positively affect depression and anxiety. (Lin et al., 2020, Musekamp et al., 2017) Importantly, while the overall PAM scores improved significantly among those who completed the program, there was no difference between the two groups post program, indicating the intervention increased patient activation similarly. This suggests that if participants are able to get to and participate fully in the CDSME sessions, patient activation (and all its associated benefits) can increase over the 6-week workshop.
However, the same factors that contribute to poorer self-reported health for those reporting a history of depression and/or anxiety are likely to contribute to less engagement in any health-related intervention and thus recruitment could remain a challenge. Therefore, it is critical that organizations delivering the program ensure that appropriate participant recruitment/engagement, dissemination, and registration processes are used.
Our evaluation suggests that a multimodal recruitment method is effective in engaging various segments of a rural population. While hearing about and signing up for programs electronically were significantly higher for those reporting a history of depression/anxiety in the bivariate analysis, the association disappeared after adjustment for all other factors. Age could be a confounding factor as younger and middle-aged individuals are more likely to be responsive to online recruitment and enrollment strategies than those who are older. (Anguera et al., Jan 2016, Arnobit et al., 2021, Salvy et al., 2020) Meanwhile, previous studies have shown that older rural adults are more likely to engage in a program if they hear about it from their provider or another trusted community source (Dibartolo and McCrone, 2003) and are then contacted by a study team member. (Myers et al., 2019) However, our sub-analysis revealed that, while not significant, older adults who reported a history of depression/anxiety were also more likely to hear about the program through electronic means than those who did not report a history of depression/anxiety.
Thus in order to have the most expansive reach, a multimodal recruitment strategy is warranted. If recruitment efforts had relied solely on participants actively contacting organizations to register for workshops after reading about the program from a flyer or other print media, it is unlikely we would have as effectively reached many of those younger individuals who are reporting a history of depression and/or anxiety.
5. Future directions
The findings from this analysis raise additional questions. According to the National Center for Health Statistics, young adults (18–29) have the highest prevalence of any form of depression, while those who are 30–44 have the lowest prevalence. The prevalence of depression among older middle age (45–64) and older adults (65+) depends on the severity of the reported depression but was generally in the middle. (Villarroel and Terlizzi, 2019) Similarly, younger adults report higher rates of anxiety than do older adults. (Goodwin et al., 2020) Since younger and middle-aged adults are more likely to respond to technology-based methods of recruitment, they may also be more responsive to technology-based versions of CDSME. (Jaglal et al., 2013) Future research could compare mental health-related outcomes for in person versus online delivery modalities in rural areas. Assuming that broadband access is available, online delivery may be more appealing because a sense of anonymity can be maintained, an issue that is important to rural residents in regards to mental health concerns. (Cheesmond et al., 2019).
6. Limitations
This study is not without limitations. First, asking participants to self-report their history of depression or anxiety disorders may have introduced bias. Previous research has shown discordance between self-report versus claims data or medical chart diagnosis for depressive disorders (Jiang et al., 2015, Singh, 2009) Related to this concern, the self-report chronic conditions checklist that participants completed combined depression and anxiety instead of separating them into two distinct diagnoses. The collapsing of these conditions into one response category may have impacted our study results and interpretation of our study findings. Our decision to use this checklist was based on its use in other program evaluations at the state and national levels. (Kulinski et al., 2014) In the future, we recommend separating these two conditions for better accuracy when examining mental health conditions. We also recommend future studies include more objective measures to identify the presence and severity of current depression and/or anxiety among participants. Second, this study engaged participants from a 6-county region in upstate New York; therefore, findings may not be widely generalizable to other rural communities or states. Third, missing data for variables of interest limited the number of participants that could be included in the multivariable regression analysis. Fourth, our sample had relatively high baseline patient activation scores, with over half of participants scoring above a 64 (beginning to take action, but lacking confidence to support new behaviors). (Hibbard et al., 2007) While this is not surprising, since enrolling in a self-management program indicates some level of engagement with the healthcare system, it highlights that these CDSME program participants may not be the same as other individuals with chronic diseases. Further research is needed to understand the ability to recruit individuals with lower levels of engagement and assess how CDSME programs can benefit them.
7. Conclusion
This analysis highlights the unique profile of rural individuals who report a history of depression and/or anxiety and how they engage with self-management programs. To engage individuals experiencing mental health conditions in rural areas, it is important to use recruitment methods that they prefer and are more likely to use. Marketing the programs using multimodal recruitment strategies is recommended as an effective strategy to reach this population in a rural region.
CRediT authorship contribution statement
Kristin Pullyblank: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Wendy Brunner: Project administration, Conceptualization, Writing – review & editing. Melissa Scribani: Formal analysis, Visualization, Writing – review & editing. Nicole Krupa: Data curation, Writing – review & editing. Marcia G. Ory: Conceptualization, Writing – review & editing. Matthew Lee Smith: Conceptualization, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors would like to acknowledge Dr. David Strogatz, Lynae Wyckoff, Jennifer Flynn, Carleen Henderson and all of the Living Well peer leaders, participants, and partnering organizations for their assistance with program implementation and data collection.
Funding
This work was supported in part by the Health Resources and Services Administration [Grant Number D04RH31785]. The funder had no role in data collection, analysis, and presentation of results.
References
- Matthews K.A., Croft J.B., Liu Y., Lu H., Kanny D., Wheaton A.G., Cunningham T.J., Khan L.K., Caraballo R.S., Holt J.B., Eke P.I., Giles W.H. Health-related behaviors by urban-rural county classification–United States, 2013. MMWR Surveill. Summ. 2017;66(5):1–8. doi: 10.15585/mmwr.ss6605a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Smith M.L. In: Handbook of Rural Aging. Kaye L.W., editor. Routledge, Taylor, and Francis; 2021. Chronic disease; pp. 68–76. [Google Scholar]
- Croft J.B., Wheaton A.G., Liu Y., Xu F., Lu H., Matthews K.A., Cunningham T.J., Wang Y., Holt J.B. Urban-Rural County and State Differences in Chronic Obstructive Pulmonary Disease — United States, 2015. MMWR Morb. Mortal. Wkly Rep. 2018;67(7):205–211. doi: 10.15585/mmwr.mm6707a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobitt J., Aguayo L., Payne L., Jansen T., Schwingel A. Geographic and social factors associated with Chronic Disease Self-Management Program participation: Going the “extra-mile” for disease prevention. Prev. Chronic Dis. 2019;16:E25. doi: 10.5888/pcd16.180385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boring M.A., Hootman J.M., Liu Y., Theis K.A., Murphy L.B., Barbour K.E., Helmick C.G., Brady T.J., Croft J.B. Prevalence of arthritis and arthritis-attributable activity limitation by urban-rural county classification–United States, 2015. MMWR Morb. Mortal. Wkly Rep. 2017;66(20):527–532. doi: 10.15585/mmwr.mm6620a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towne S.D., Callaghan T.H., Ferdinand A.O., Akinlotan M., Primm K., Bolin J. Prevalence and mortality of heart disease and related conditions: Disparities affecting the south, rural areas, and American Indian and Alaska Natives [Policy brief] 2019. https://srhrc.tamhsc.edu/docs/srhrc-pb5-towne-heartdisease.pdf
- Myers C.R. Using telehealth to remediate rural mental health and healthcare disparities. Issues Ment. Health Nurs. 2019;40(3):233–239. doi: 10.1080/01612840.2018.1499157. [DOI] [PubMed] [Google Scholar]
- Crittenden J.A. In: Handbook of Rural Aging. Kaye L.W., editor. Taylor & Francis Group; Routledge: 2021. Mental and Behavioral Health; pp. 284–288. [Google Scholar]
- Diez Roux A.V. Despair as a cause of death: more complex than it first appears. Am. J. Public Health. 2017;107(10):1566–1567. doi: 10.2105/AJPH.2017.304041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.L., Towne S.D., Herrera-Venson A., et al. Dissemination of Chronic Disease Self-Management Education (CDSME) Programs in the United States: Intervention delivery by rurality. Int. J. Environ. Res. Public Health. 2017;14(6) doi: 10.3390/ijerph14060638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers-Gabr N.M. Rural-urban mental health disparities in the United States during COVID-19. Psychol Trauma. 2020;12(S1):S222–S224. doi: 10.1037/tra0000871. [DOI] [PubMed] [Google Scholar]
- Lee H.J., McDonagh M.K. Springer Publishing Company; New York, NY: 2018. Rural Nursing: Concepts, Theory, and Practice. [Google Scholar]
- Grady P.A., Gough L.L. Self-management: a comprehensive approach to management of chronic conditions. Am. J. Public Health. 2014;104(8):e25–e31. doi: 10.2105/AJPH.2014.302041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jowsey T., Jeon Y.-H., Dugdale P., Glasgow N.J., Kljakovic M., Usherwood T. Challenges for co-morbid chronic illness care and policy in Australia: a qualitative study. Aust. N Z Health Policy. 2009;6(1) doi: 10.1186/1743-8462-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariel-Donges A.H., Gordon E.L., Dixon B.N., et al. Rural/urban disparities in access to the National Diabetes Prevention Program. Transl Behav Med. 2019 doi: 10.1093/tbm/ibz098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnobit C.I., Loo K., Pagano I., et al. Recruiting cancer survivors to a mobile mindfulness intervention in the United States: Exploring online and face-to-face recruitment strategies. Int. J. Environ. Res. Public Health. 2021;18(19) doi: 10.3390/ijerph181910136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Lorig K., Ritter P.L., Turner R.M., English K., Laurent D.D., Greenberg J. A diabetes self-management program: 12-month outcome sustainability from a nonreinforced pragmatic trial. J. Med. Internet Res. 2016;18(12):e322. doi: 10.2196/jmir.6484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K.R., Sobel D.S., Stewart A.L., Brown B.W., Bandura A., Ritter P., Gonzalez V.M., Laurent D.D., Holman H.R. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Med. Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Lee S., Jiang L., Dowdy D., Hong Y.A., Ory M.G. Effects of the Chronic Disease Self-Management Program on medication adherence among older adults. Translational Behavioral Medicine. 2019;9(2):380–388. doi: 10.1093/tbm/iby057. [DOI] [PubMed] [Google Scholar]
- University of Minnesota Rural Health Research Center and NORC Walsh Center for Rural Health Analysis, 2019. Mental Health in Rural Communities Toolkit [online]. Assessed January 26, 2022, https://www.ruralhealthinfo.org/toolkits/mental-health/1/barriers.
- Ory M.G., Ahn S., Jiang L., Smith M.L., Ritter P.L., Whitelaw N., Lorig K. Successes of a national study of the chronic disease self-management program: Meeting the triple aim of health care reform. Med. Care. 2013;51(11):992–998. doi: 10.1097/MLR.0b013e3182a95dd1. [DOI] [PubMed] [Google Scholar]
- Mehlsen M., Heegaard L., Frostholm L. A prospective evaluation of the Chronic Pain Self-Management Programme in a Danish population of chronic pain patients. Patient Educ. Couns. 2015;98(5):677–680. doi: 10.1016/j.pec.2015.01.008. [DOI] [PubMed] [Google Scholar]
- Lorig K., Ritter P.L., Pifer C., Werner P. Effectiveness of the chronic disease self-management program for persons with a serious mental illness: a translation study. Community Ment. Health J. 2014;50(1):96–103. doi: 10.1007/s10597-013-9615-5. [DOI] [PubMed] [Google Scholar]
- Ritter P.L., Ory M.G., Laurent D.D., Lorig K. Effects of chronic disease self-management programs for participants with higher depression scores: secondary analyses of an on-line and a small-group program. Transl. Behav. Med. 2014;4(4):398–406. doi: 10.1007/s13142-014-0277-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericks S., Lapum J., Lo J. Anxiety, depression, and self-management: a systematic review. Clin Nurs Res. 2012;21(4):411–430. doi: 10.1177/1054773812436681. [DOI] [PubMed] [Google Scholar]
- Towne S.D., Jr., Smith M.L., Ahn S., Ory M.G. The reach of chronic-disease self-management education programs to rural populations. Front. Public Health. 2015;2:172. doi: 10.3389/fpubh.2014.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towne S.D., Smith M.L., Ahn S., Altpeter M., Belza B., Kulinski K.P., Ory M.G. National dissemination of multiple evidence-based disease prevention programs: reach to vulnerable older adults. Front. Public Health. 2015;2 doi: 10.3389/fpubh.2014.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn S., Smith M.L., Cho J., Jiang L., Post L., Ory M.G. Factors associated with successful completion of the chronic disease self-management program among middle-aged and older asian-american participants: a national study. Front. Public Health. 2014;2:257. doi: 10.3389/fpubh.2014.00257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, M.L., Towne, S.D., Jr., Bergeron, C.D., et al. Geographic disparities associated with travel to medical care and attendance in programs to prevent/manage chronic illness among middle-aged and older adults in Texas. Rural Remote Health. Nov 2019;19(4):5147. 10.22605/RRH5147. [DOI] [PubMed]
- Dattalo M., Wise M., Ford Ii J.H., Abramson B., Mahoney J. Essential resources for implementation and sustainability of evidence-based health promotion programs: a mixed methods multi-site case study. J. Community Health. 2017;42(2):358–368. doi: 10.1007/s10900-016-0263-x. [DOI] [PubMed] [Google Scholar]
- Horrell L.N., Kneipp S.M. Strategies for recruiting populations to participate in the chronic disease self-management program (CDSMP): A systematic review. Health Mark. Q. 2017;34(4):268–283. doi: 10.1080/07359683.2017.1375240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeFort S.M., Gray-Donald K., Rowat K.M., Jeans M. Randomized controlled trial of a community-based psychoeducation program for the self-management of chronic pain. Pain. 1998;74:297–306. doi: 10.1016/s0304-3959(97)00190-5. [DOI] [PubMed] [Google Scholar]
- Kirby J.B., Zuvekas S.H., Borsky A.E., Ngo-Metzger Q. Rural residents with mental health needs have fewer care visits than urban counterparts. Health Aff. (Millwood). 2019;38(12):2057–2060. doi: 10.1377/hlthaff.2019.00369. [DOI] [PubMed] [Google Scholar]
- Kulinski K.P., Boutaugh M., Smith M.L., Ory M.G., Lorig K. Setting the stage: measure selection, coordination, and data collection for a national self-management initiative. Front. Public Health. 2014;2:206. doi: 10.3389/fpubh.2014.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard J. University of Oregon; 2017. Assessing measurement properties of the PAM 10 and 13. [Google Scholar]
- Patient Activation Measure (PAM). Insignia Health. https://www.insigniahealth.com/products/pam-survey.
- Villarroel, M.A., Terlizzi, E.P. Symptoms of depression among adults: United States, 2019. 2020. NCHS Data Brief. [PubMed]
- Maneze D., Everett B., Astorga C., Yogendran D., Salamonson Y. The influence of health literacy and depression on diabetes self-management: a cross-sectional study. J. Diabetes Res. 2016;2016:3458969. doi: 10.1155/2016/3458969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129(1_suppl2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faravelli C., Alessandra Scarpato M., Castellini G., Lo S.C. Gender differences in depression and anxiety: the role of age. Psychiatry Res. 2013;210(3):1301–1303. doi: 10.1016/j.psychres.2013.09.027. [DOI] [PubMed] [Google Scholar]
- Hibbard J.H., Mahoney E.R., Stock R., Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv. Res. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardman R., Begg S., Spelten E. What impact do chronic disease self-management support interventions have on health inequity gaps related to socioeconomic status: a systematic review. BMC Health Serv. Res. 2020;20(1) doi: 10.1186/s12913-020-5010-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M.-Y., Weng W.-S., Apriliyasari R.W., Van truong P., Tsai P.-S. Effects of patient activation intervention on chronic diseases: A meta-analysis. J. Nurs. Res. 2020;28(5):e116. doi: 10.1097/jnr.0000000000000387. [DOI] [PubMed] [Google Scholar]
- Musekamp G., Schuler M., Seekatz B., Bengel J., Faller H., Meng K. Does improvement in self-management skills predict improvement in quality of life and depressive symptoms? A prospective study in patients with heart failure up to one year after self-management education. BMC Cardiovasc. Disord. 2017;17(1) doi: 10.1186/s12872-017-0486-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anguera J.A., Jordan J.T., Castaneda D., Gazzaley A., Arean P.A. Conducting a fully mobile and randomised clinical trial for depression: access, engagement and expense. BMJ Innov. 2016;2(1):14–21. doi: 10.1136/bmjinnov-2015-000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvy S.-J., Carandang K., Vigen C.LP., Concha-Chavez A., Sequeira P.A., Blanchard J., Diaz J., Raymond J., Pyatak E.A. Effectiveness of social media (Facebook), targeted mailing, and in-person solicitation for the recruitment of young adult in a diabetes self-management clinical trial. Clin Trials. 2020;17(6):664–674. doi: 10.1177/1740774520933362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dibartolo M.C., McCrone S. Recruitment of rural community-dwelling older adults: barriers, challenges, and strategies. Aging Ment Health. 2003;7(2):75–82. doi: 10.1080/1360786031000072295. [DOI] [PubMed] [Google Scholar]
- Myers B.A., Pillay Y., Guyton Hornsby W., Shubrook J., Saha C., Mather K.J., Fitzpatrick K., de Groot M. Recruitment effort and costs from a multi-center randomized controlled trial for treating depression in type 2 diabetes. Trials. 2019;20(1) doi: 10.1186/s13063-019-3712-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin R.D., Weinberger A.H., Kim J.H., Wu M., Galea S. Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. J. Psychiatr. Res. 2020;130:441–446. doi: 10.1016/j.jpsychires.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaglal S.B., Haroun V.A., Salbach N.M., Hawker G., Voth J., Lou W., Kontos P., Cameron J.E., Cockerill R., Bereket T. Increasing access to chronic disease self-management programs in rural and remote communities using telehealth. Telemed. J. E Health. 2013;19(6):467–473. doi: 10.1089/tmj.2012.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U. S. A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheesmond N.E., Davies K., Inder K.J. Exploring the role of rurality and rural identity in mental health help-seeking behavior: A systematic qualitative review. J. Rural Mental Health. 2019;43(1):45–59. doi: 10.1037/rmh0000109. [DOI] [Google Scholar]
- Jiang L., Zhang B., Smith M.L., Lorden A.L., Radcliff T.A., Lorig K., Howell B.L., Whitelaw N., Ory M.G. Concordance between self-reports and medicare claims among participants in a national study of chronic disease self-management program. Front. Public Health. 2015;3 doi: 10.3389/fpubh.2015.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh J.A. Accuracy of Veterans Affairs databases for diagnoses of chronic diseases. Preventing Chronic Disease. 2009;6(4) [PMC free article] [PubMed] [Google Scholar]