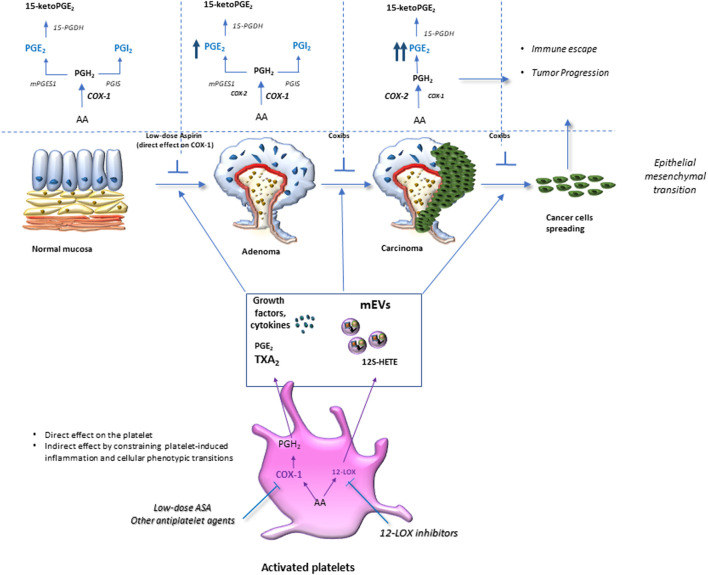
FIGURE 3.
Platelet activation in response to intestinal damage is crucial in chronic inflammation/fibrosis. Platelet activation in response to intestinal epithelial damage contributes to acute inflammation by promoting leukocyte recruitment to restore normal tissue function. However, exaggerated platelet activation is associated with an elevated release of thromboxane (TX) A2 and prostaglandin (PG)E2, growth factors, angiogenic factors, cytokines, and chemokines, as well as medium-sized extracellular vesicles (mEVs) rich in genetic material (mRNAs and microRNAs). These factors activate stromal cells (such as myofibroblasts and immune cells), thus increasing the production and release of growth factors and inflammatory mediators, including PGE2, due to cyclooxygenase (COX)-2 induction. Platelet-derived TXA2 induces phenotypic and functional changes in myofibroblasts, such as the reduction of α-Alpha Smooth Muscle Actin (SMA) and the increase of vimentin fibronectin RhoA expression; these events lead to an enhanced capacity to proliferate and migrate, thus, contributing to chronic intestinal inflammation and fibrosis. The inhibition of platelet COX-1 activity (by low-dose Aspirin) or blocking the TXA2 receptor (TP) can mitigate chronic intestinal inflammation and fibrosis.