Abstract
Objective
This longitudinal study examined changes in psychological outcomes of perioperative frontline healthcare workers at one of Australia’s most COVID-19 affected hospitals, following the surge and decline of a pandemic wave.
Method
A single-centred longitudinal online survey was conducted between 26 May and 17 November 2020. Recruitment was via poster advertisement and email invitation. The survey was sent out every 4 weeks, resulting in seven time-points.
Results
In total, 385 survey results were analysed from 193 staff (about 64% response rate), 72 (37%) of whom completed the survey more than once. The prevalence of moderate-to-severe anxiety and depressive symptoms peaked at 27% and 25%, respectively, during the pandemic surge. Up to 35% displayed post-traumatic stress disorder (PTSD) symptoms. Although not statistically significant, the trend of depressive and PTSD symptoms worsened over time, especially among females and anaesthetic/surgical trainees, despite subsidence of the pandemic curve. Technicians and anaesthetic/scrub nurses were the at-risk groups with worst psychological outcomes.
Conclusion
We found persistent mental health impacts on frontline perioperative HCWs despite subsidence of the pandemic wave. Further research is needed to determine the extent and trajectory of such impacts with larger sample sizes to determine generalisability to frontline HCWs in general.
Keywords: Longitudinal survey, psychological impact, perioperative frontline healthcare workers, COVID-19 pandemic
A compelling body of evidence illustrates a high degree of mental health vulnerability among healthcare workers (HCWs) during the COVID-19 pandemic. Notably, several studies demonstrated an increased incidence of depression, anxiety, insomnia and distress among HCWs.1–6 Simply being a HCW was identified as an independent predictor of psychological distress;1–4 being a frontline HCW was associated with worst outcomes.7,8
At 18 October 2021, Victoria was the most affected Australian state,9 and experienced the longest lockdown globally.10 The Royal Melbourne Hospital (RMH) remains the epicentre of COVID cases in Victoria.11 Perioperative staff at RMH face many workplace stressors. There are constant concerns about aerosol transmission of COVID-19, because aerosol-generating procedures are regularly performed in operating theatres,12 and frequently on patients with unknown COVID-19 status (e.g. trauma or unconscious patients requiring urgent surgery and/or intubation). They also experience frequent changes of personal protective equipment (PPE) requirements, theatre workflow and workload.
While much evidence illuminates psychological concerns among HCWs, most research was cross-sectional. Given the dynamic nature of mental health in relation to environmental changes, understanding longitudinal trajectories is critical. Our longitudinal study evaluated the psychological impact of the COVID-19 pandemic on RMH perioperative staff, examining changes over time. We investigated whether baseline characteristics influenced changes and associations between key characteristics and psychological outcomes.
Methods
This single-centre longitudinal online survey was conducted between 26 May and 17 November 2020; coinciding with the ‘second wave’ of COVID-19 in Victoria, Australia. Hosted by REDCap10.5.2 (Vanderbilt University, Nashville, Tennessee, USA), outcome assessment was undertaken 4-weekly, providing seven time-points in total. Melbourne Health Human Research Ethics Committee approved this study (HREC/63609/MH-2020).
Recruitment was via poster advertisement and emails sent to all RMH perioperative staff every 4 weeks. The survey was open for 1 week at each time-point. The study population consisted of approximately 300 members, including anaesthetic or surgical consultants and trainees, anaesthetic or scrub nurses and theatre technicians. Participation was voluntary, participants could join at any time-point, and consent was implied upon survey completion.
Demographic and COVID-19 exposure details were recorded (Supplemental Appendix 1). To maintain confidentiality, two additional items (favourite drink and first pet name) were included to facilitate participant matching across time-points, in conjunction with other characteristics (e.g. age group, gender, professional group and years worked).
Primary outcomes were anxiety, depression and post-traumatic stress disorder (PTSD) symptomatology measured using the Generalised Anxiety Disorder scale (GAD-7; range 0–21), Patient Health Questionnaire (PHQ-9; range 0–27) and Primary Care-Post-Traumatic Stress Disorder (PC-PTSD-5) questionnaire, respectively. On the seventh survey, the PC-PTSD-5 questionnaire was replaced by the Impact Event Scale–revised (IES-R-22; range 0–88) and Abbreviated Maslach Burnout Inventory (A-MBI-9; range 0–18).
Linear mixed models with random intercepts were fitted to examine differences in psychological health (GAD-7, PHQ-9 and PC-PTSD-5 scores) over time with and without adjustment for age group, gender, profession, years worked, pre-existing mental illness and number of COVID-19 patients and related-deaths encountered.
Interactions between time and (1) gender, (2) profession and (3) pre-existing mental illness were considered in linear mixed models, as were associations between number of (1) COVID-patients and (2) COVID-deaths encountered and (3) professional group, for each psychological outcome. Analyses were conducted using Stata 13.0 (Statacorp, College Station, Texas, USA).
Results
In total, 406 surveys were completed across seven time-points. Twenty-one entries containing repeat (within same time-point) or no data were excluded. This left 385 entries from 193 participants (about 64% response rate) for analysis; 72 (37%) completed the survey more than once, 10% had five or more time-points.
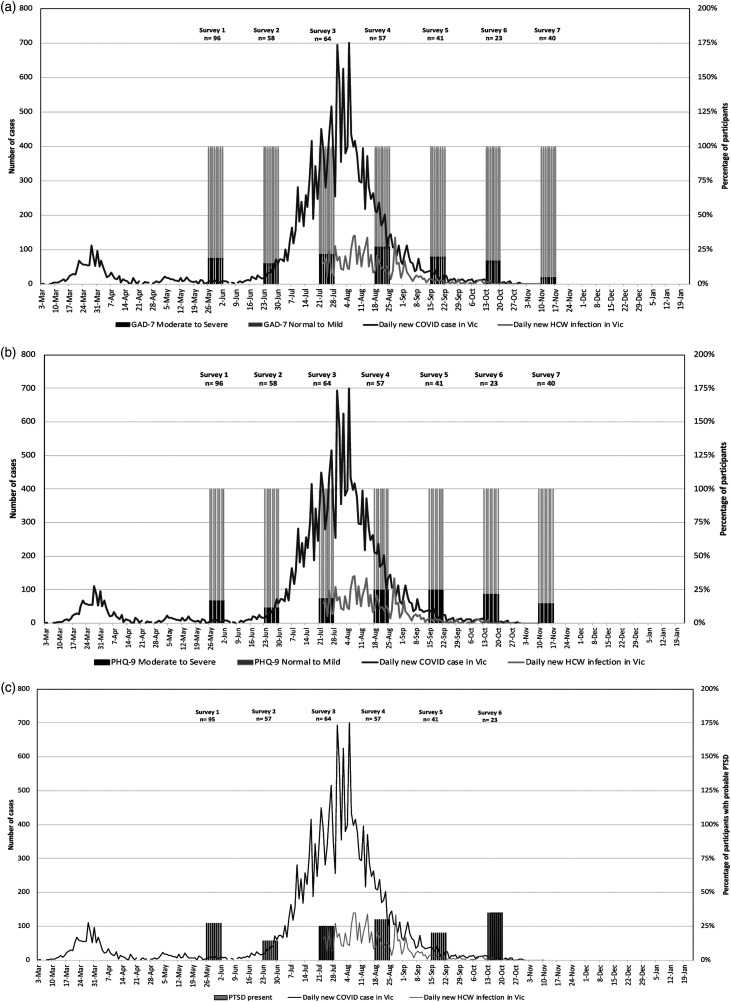
Demographic and COVID-exposure data are shown in Table 1. Immediately after the second pandemic wave peaked, 27% and 25% of the participants experienced moderate-to-severe anxiety and depressive symptoms, respectively (Figure 1 and Table 2). Further, 35% of the participants experienced PTSD symptoms towards the end of the pandemic wave.
Table 1.
Participating perioperative staff demographic characteristics at entry to the studya and overall COVID-exposure details
| N = 193 | |
|---|---|
| Age group (years), n (%) | |
| >20–30 | 28 (15) |
| >30–40 | 66 (34) |
| >40–50 | 53 (28) |
| >50–60 | 34 (17) |
| >60–70 | 10 (5) |
| >70 | 2 (1) |
| Sex, n (%) | |
| Female | 116 (60) |
| Male | 74 (38) |
| Other | 3 (2) |
| Living with a child <16 years old, n (%) | 61 (32) |
| Living with an adult >65 years old, n (%) | 15 (8) |
| Profession, n (%) | |
| Anaesthetic consultant | 41 (21) |
| Anaesthetic nurse | 36 (19) |
| Anaesthetic trainee | 18 (9) |
| Scrub nurse | 21 (11) |
| Surgical consultant | 29 (15) |
| Surgical trainee | 8 (4) |
| Technician | 13 (7) |
| Other | 27 (14) |
| Average hours worked per week, mean (SD), min–max | 37.5 (10.9), 1–70 |
| Number of years worked at current role, mean (SD), min–max | 10.8 (9.8), 0–43 |
| Working locationb, n (%) | |
| Operating theatre | 149 (77) |
| Intensive care unit | 2 (1) |
| Recovery area | 29 (15) |
| Emergency department | 10 (5) |
| Dedicated COVID ward | 1 (1) |
| Non-COVID ward | 13 (7) |
| Other | 35 (18) |
| Pre-existing baseline mental health issues, including anxiety, depression or post-traumatic stress disorder, n (%) | 36 (19) |
| Number of COVID-19 patients encountered every 4 weeks, mean (SD), min–max | 4 (15), 0–240 |
| Total number of participants who encountered COVID-related deaths, n(%) | 6 (3) |
| Total number of participants tested positive, n (%) | 17 (9) |
| Total number of participants who had been quarantined, n (%) | 17 (9) |
| Total number of participants with close friends or relatives tested positive with COVID-19, n (%) | 23 (12) |
| Total number of participants with close friends or relatives died from COVID-19, n (%) | 3 (2) |
aStaff could enter the study at any point during the seven survey rounds.
bStaff could indicate multiple working locations.
Figure 1.
Daily new COVID-19 case and healthcare worker infection in Victoria (Vic), Australia in 2020; overlaid with categorised psychological health outcomes. Note. A = anxiety outcomes; B = depression outcomes; C = PTSD outcomes; GAD = generalised anxiety score; PHQ = patient health questionnaire; PTSD = post-traumatic stress score.
Table 2.
Severity categories of anxiety and depression; and presence of post-traumatic stress disorder in each round of the survey
| Survey round 1 (26/5/20–2/6/20) | Survey round 2 (23/6/20–30/6/20) | Survey round 3 (21/7/20–28/7/20) | Survey round 4 (18/8/20–25/8/20) | Survey round 5 (15/9/20–22/9/20) | Survey round 6 (13/10/20–20/10/20) | Survey round 7 (10/11/20–17/11/20) | |
|---|---|---|---|---|---|---|---|
| GAD-7, anxiety symptoms (score) | N = 96 | N = 58 | N = 64 | N = 57 | N = 41 | N = 23 | N = 40 |
| Normal (0–4) | 51 (53%) | 38 (66%) | 27 (42%) | 27 (47%) | 22 (53%) | 14 (61%) | 28 (70%) |
| Mild (5-9) | 27 (28%) | 11 (19%) | 23 (36%) | 15 (26%) | 11 (27%) | 5 (22%) | 10 (25%) |
| Moderate (10-14) | 13 (14%) | 6 (10%) | 9 (14%) | 9 (16%) | 6 (15%) | 1 (4%) | 1 (2.5%) |
| Severe (15–21) | 5 (5%) | 3 (5%) | 5 (8%) | 6 (11%) | 2 (5%) | 3 (13%) | 1 (2.5%) |
| PHQ-9, depressive symptoms (score) | N = 96 | N = 58 | N = 64 | N = 57 | N = 41 | N = 23 | N = 40 |
| Normal (0–4) | 57 (60%) | 35 (60%) | 34 (53%) | 28 (49%) | 21 (51%) | 10 (43%) | 24 (60%) |
| Mild (5–9) | 22 (23%) | 16 (28%) | 18 (28%) | 15 (26%) | 10 (24%) | 8 (35%) | 10 (25%) |
| Moderate (10–14) | 13 (14%) | 3 (5%) | 7 (11%) | 8 (14%) | 5 (12%) | 2 (9%) | 5 (12.5%) |
| Moderate severe (15–19) | 3 (3%) | 1 (2%) | 5 (8%) | 5 (9%) | 4 (10%) | 1 (4%) | 1 (2.5%) |
| Severe (20–27) | 1 (1%) | 3 (5%) | 0 (0%) | 1 (2%) | 1 (3%) | 2 (9%) | 0 (0%) |
| PTSD, post-traumatic stress disorder (score) | N = 95 | N = 57 | N = 64 | N = 57 | N = 41 | N = 23 | |
| Present (≥3) | 26 (27%) | 8 (14%) | 16 (25%) | 17 (30%) | 8 (20%) | 8 (35%) | N/A |
| IES-R, distress symptoms (score) | N = 38 | ||||||
| Normal (0–23) | N/A | N/A | N/A | N/A | N/A | N/A | 18 (47%) |
| Mild (24–32) | 18 (47%) | ||||||
| Moderate (33–36) | 1 (3%) | ||||||
| Severe (≥37) | 1 (3%) | ||||||
| AMBI, burnout symptoms (scale 0-18) | N = 38 | ||||||
| Emotional exhaustion | N/A | N/A | N/A | N/A | N/A | N/A | 10 (5–12[1–17]) |
| Depersonalisation | 2 (1–6[0–16]) | ||||||
| Personal accomplishment | 13.5 (12–16[6–18]) | ||||||
Note. GAD-7 = Generalised Anxiety Disorder inventory; PHQ-9 = Patient Health Questionnaire; PC-PTSD-5 = Primary Care - Post-Traumatic Stress Disorder questionnaire.
Values are presented as number (percentage) or median(IQR[range]).
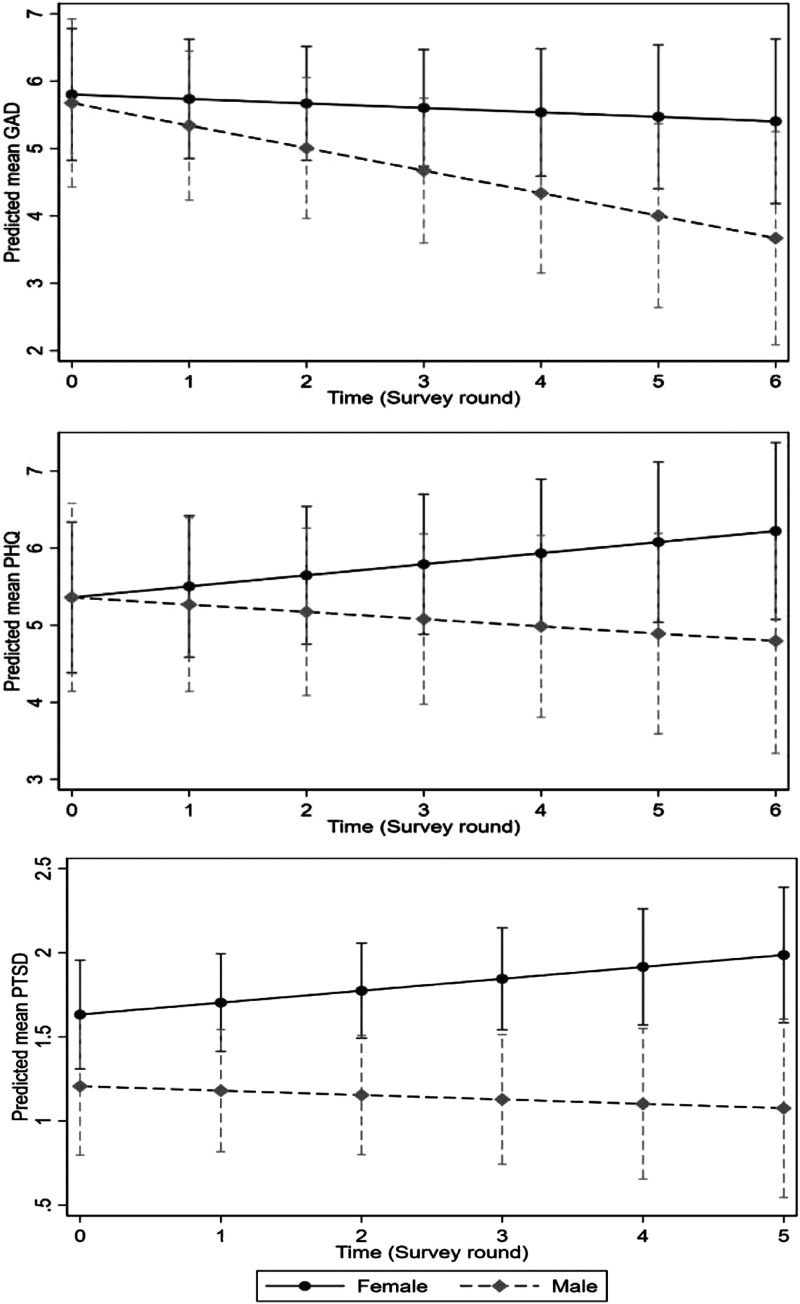
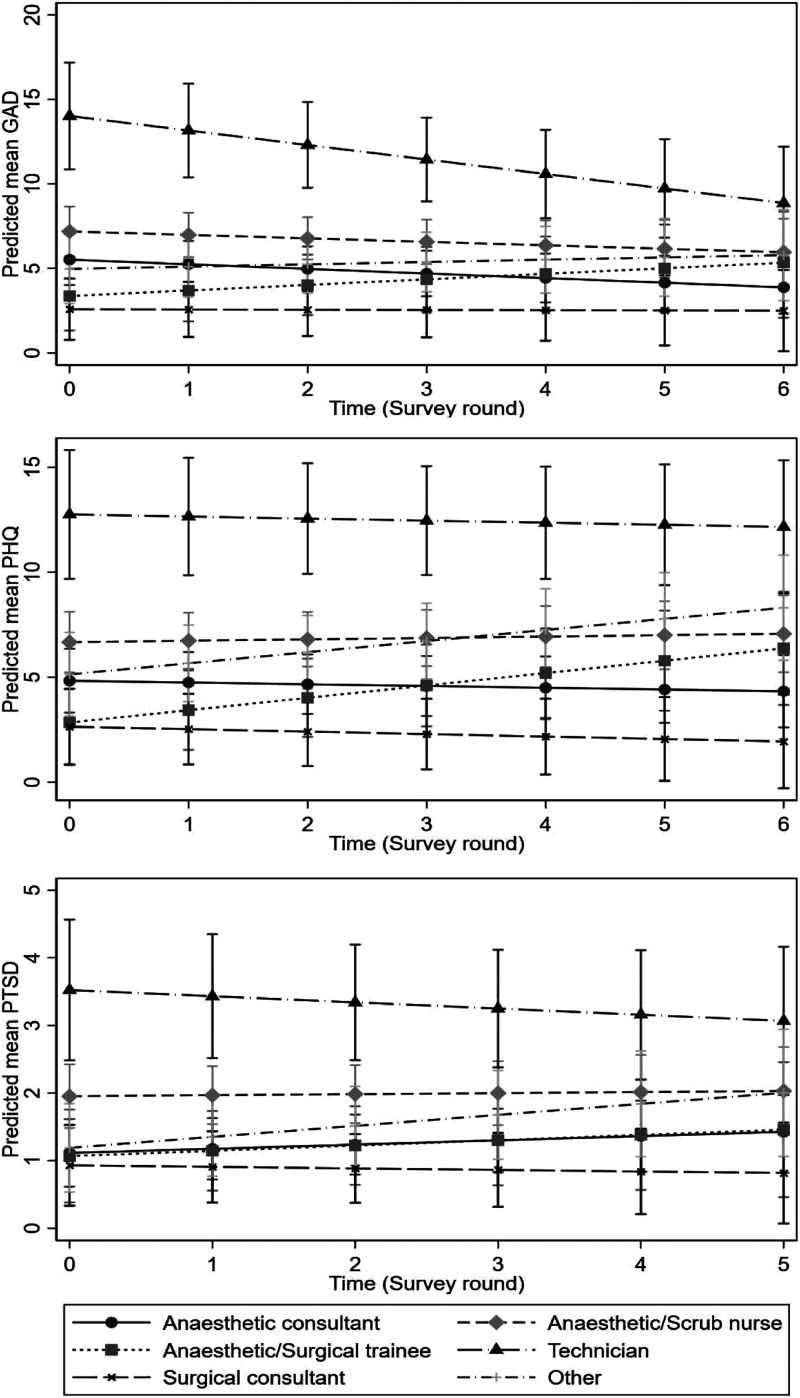
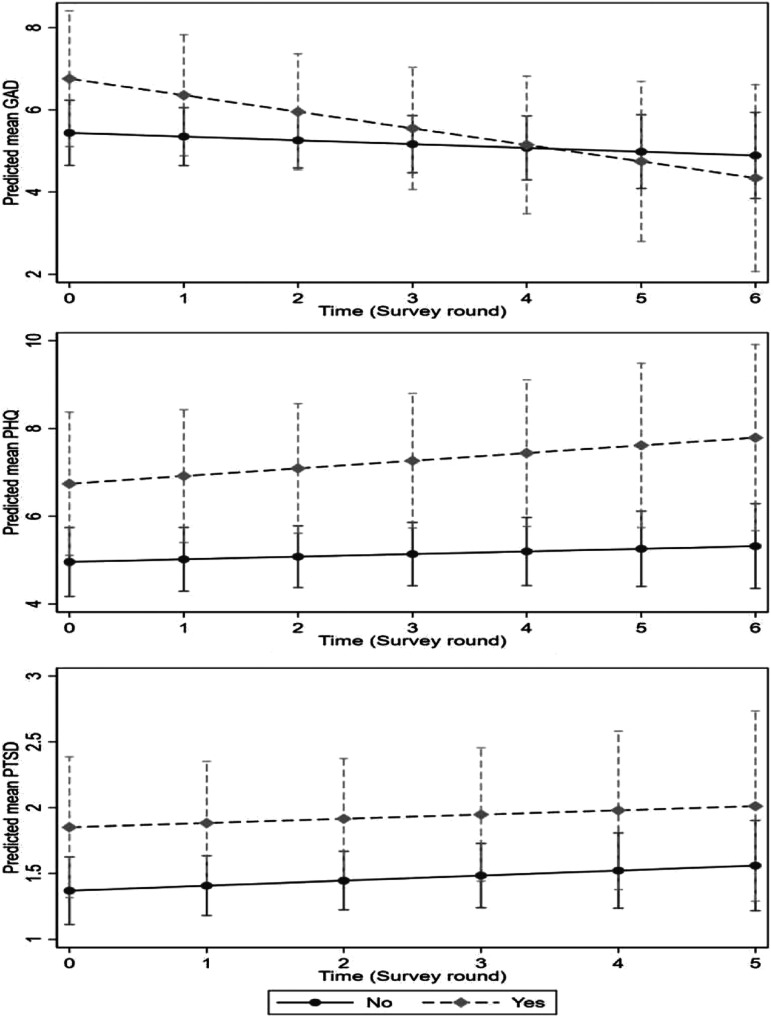
Results indicated GAD-7 decreased on average by 0.15 per 4-week period (95% CI: −0.33, 0.04), whereas PHQ-9 (0.08, 95% CI: −0.07, 0.23) and PC-PTSD-5 (0.04, 95% CI: −0.03, 0.11) increased (Table 3). All psychological outcomes were worse for females than males (Figure 2); and worst among technicians and best among surgical consultants across all time-points (Figure 3). They were worse initially for those with pre-existing mental illness (Figure 4). PHQ and PTSD scores were increasing (i.e. worsening) over time for females and anaesthetic/surgical trainees.
Table 3.
Unadjusted and adjusted estimates of the change in primary outcome summary scores over time from linear mixed models
| Unadjusted | Adjusteda | ||||||
|---|---|---|---|---|---|---|---|
| Coef | 95% CI | p-value | Coef | 95% CI | p-value | ||
| GAD-7 (n = 182b) | |||||||
| Timec | −0.04 | (−0.24, 0.15) | .661 | −0.15 | (−0.33, 0.04) | .121 | |
| PHQ-9 (n = 182b) | |||||||
| Timec | 0.12 | (−0.04, 0.28) | .137 | 0.08 | (−0.07, 0.23) | .308 | |
| PC-PTSD-5 (n = 171b) | |||||||
| Timec | 0.05 | (−0.02, 0.12) | .183 | 0.04 | (−0.03, 0.11) | .309 | |
Note. GAD-7 = Generalised Anxiety Disorder inventory; PHQ-9 = Patient Health Questionnaire; PC-PTSD-5 = Primary Care - Post-Traumatic Stress Disorder questionnaire; CI = confidence interval; Coef = coefficient.
aLinear mixed models with random intercepts adjusted for participant age, gender, professional group, years worked, pre-existing mental health issues, number of COVID related deaths encountered and number of COVID patients encountered.
bThe number of unique participants included in the model with the outcome measured on at least one survey wave. There were 359 unique observations for GAD-7 and PHQ-9 for these 182 participants with the number of observations per participant ranging from 1 to 7. There were 321 unique observations for PC-PTSD-5 PTSD with the number of observations per participant ranging from 1 to 6. The residual intraclass correlation from adjusted models was estimated to be 0.55 (95% CI 0.44–0.66), 0.73 (95% CI 0.65–0.80) for PHQ-9, 0.63 (95% CI 0.52–0.72) for PC-PTSD-5 PTSD.
cTime represents the mean difference in outcome per survey round (i.e. per 4-week period).
Figure 2.
Estimated average mean scores and 95% confidence intervals over time (survey round) by gender identity from linear mixed models with an interaction between gender and time. Note. GAD = generalised anxiety score; PHQ = patient health questionnaire; PTSD = post-traumatic stress score.
Figure 3.
Estimated average mean scores and 95% confidence intervals by time (survey round) by profession. Note. GAD = generalised anxiety score; PHQ = patient health questionnaire; PTSD = post-traumatic stress score.
Figure 4.
Estimated average mean scores and 95% confidence intervals over time (survey round) by whether participants have pre-existing baseline mental health issues including anxiety, depression and post-traumatic stress symptoms. Note. GAD = generalised anxiety score; PHQ = patient health questionnaire; PTSD = post-traumatic stress score.
Both technicians and anaesthetic/scrub nurses had significantly worse psychological outcomes, whereas surgeons had significantly less anxiety and depression relative to anaesthetic consultants (Table 4).
Table 4.
Unadjusted estimates from linear mixed models of associations between each of profession, number of COVID patients encountered and number of COVID related deaths encountered and each psychological health outcomes
| GAD | PHQ | PTSD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef | 95% CI | p-value | Coef | 95% CI | p-value | Coef | 95% CI | p-value | |
| COVID patients (n = 186) | 0.02 | (−0.01, 0.05) | .107 | 0.03 | (0.00, 0.06) | .039a | 0.00 | (−0.01, 0.02) | .675 |
| COVID deaths (n = 187) | 0.12 | (−0.78, 1.03) | .787 | 0.05 | (−0.75, 0.84) | .911 | −0.05 | (−0.31, 0.22) | .716 |
| Profession (n = 187) | |||||||||
| Anaesthetic consultant | Ref | Ref | Ref | ||||||
| Anaesthetic/Scrub nurse | 2.80 | (1.14, 4.46) | .001a | 3.25 | (1.55, 4.95) | <.001a | 1.20 | (0.65, 1.76) | <.001a |
| Anaesthetic/Surgical trainee | 0.24 | (−1.79, 2.27) | .814 | 0.69 | (−1.39, 2.77) | .515 | 0.34 | (−0.32, 1.01) | .316 |
| Technician | 7.54 | (5.00, 10.09) | <.001a | 8.92 | (6.31, 11.52) | <.001a | 2.13 | (1.28, 2.98) | <.001a |
| Surgical consultant | −2.27 | (−4.21, −0.34) | 0.021a | −2.40 | (−4.39, −0.42) | .018a | −0.41 | (−1.04, 0.23) | .209 |
| Other | 1.47 | (−0.56, 3.51) | .157 | 3.09 | (1.01, 5.17) | .004a | 0.56 | (−0.13, 1.26) | .114 |
Note. GAD = generalised anxiety score; PHQ = patient health questionnaire; PTSD = post-traumatic stress score; CI = confidence interval; Coef. = coefficient.
aStatistically significant.
Discussion
This study demonstrated a significant psychological impact of COVID-19 on frontline perioperative HCWs at one of Australia’s most affected hospitals over a 6-month period. The prevalence of moderate-to-severe anxiety, depressive and PTSD symptoms reached 27%, 25% and 35%, respectively, during the second pandemic wave. While the findings are comparable to global systematic reviews,1,3,5,7 divergence is evident at a local level. Notably, our findings reflect worse outcomes than Dobson and colleague’s cross-sectional study.13 The different survey time may account for differing results.14 This highlights the dynamic nature of HCWs’ emotional responses, hence importance of a longitudinal study.
Longitudinally, although not statistically significant, anxiety appeared to decrease over time. Previous research showed that being clinically unprepared was associated with worse anxiety,15 whereas systemic support and adequate knowledge protected HCWs against adverse psychological outcomes.16 During the early stage of this study, there was minimal knowledge about the virus and PPE requirement. As the pandemic evolved, organisational support was strengthened, with provision of procedural guidelines,17 team communications and training.11
In contrast, depressive and PTSD symptoms worsened over time, although not statistically significant, during the study period, particularly among females and anaesthetic or surgical trainees. Our findings align with emerging literature highlighting poor psychological outcomes for women5,6,16 and junior doctors18,19 during the pandemic. Elevated levels of psychological distress found in this cohort during non-pandemic times,20 may confer increased risk during a crisis.
Technicians and anaesthetic or scrub nurses exhibited poor psychological outcomes. Both groups lacked control in their workflow and were frequently deployed to high-risk duties. Moreover, technicians as a group tend to be overlooked, because of their small workforce. They mostly worked solo, which might reduce support and communication to and within the group. Contrarily, surgeons demonstrated favourable psychological outcomes, possibly because of their autonomy in decision making, and the reduction in direct patient contact, due to cutback in elective cases and options of telehealth consultation.
This study is not without limitation. Although our sample size was modest, we had a reasonable response rate of 64% and representation across a range of HCW roles. However, there was high attrition across time, only 37% of 193 participants had longitudinal data, limiting the ability to assess within-individual change. Although efforts were made to verify repeated observations using multiple questionnaire items, the possibility of misclassification remained. Furthermore, the small sample size and covariate adjustment required reduced power to detect significant differences.
In conclusion, this study gives a partial longitudinal view of the psychological health of frontline perioperative HCWs, working at one of Australia’s most COVID-19 affected hospitals during a pandemic wave. It highlighted the persistent psychological impact despite subsidence of the pandemic wave. Further research is needed to determine the extent and trajectory of such impacts with larger sample sizes to determine generalisability to frontline HCWs.
Supplemental Material
Supplemental Material, sj-pdf-1-apy-10.1177_10398562221077887 for A longitudinal study of the psychological impact of the COVID-19 pandemic on frontline perioperative healthcare staff in an Australian tertiary public hospital by Irene Ng, Elizabeth Barson, Caroline Fisher, Reny Segal, Daryl L Williams, Roni B Krieser, Paul M Mezzavi, Keat Lee, Yinwei Chen, Teresa Sindoni, Jessica Xu, Karen Lambt and Toni Withiel in Hand Therapy
Acknowledgements
We thank the perioperative staff at the Royal Melbourne Hospital for the participation in this longitudinal study.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Irene Ng https://orcid.org/0000-0002-6632-5604
Caroline Fisher https://orcid.org/0000-0002-4570-8526
Daryl L Williams https://orcid.org/0000-0002-6987-5804
Jessica Xu https://orcid.org/0000-0002-4697-1625
References
- 1.Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2020; 295: 113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020; 288: 112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krishnamoorthy Y, Nagarajan R, Saya GK, et al. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2020; 293: 113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3: e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020; 88: 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paybast S, Baghalha F, Emami A, et al. The anxiety disorder among the healthcare providers during the COVID-19 infection pandemic: a systematic review. Int Clin Neurosci J 2020; 7(3): 115–121. [Google Scholar]
- 7.Thakur B, Pathak M. Burden of predominant psychological reactions among the healthcare workers and general during COVID-19 pandemic phase: a systematic review and meta-analysis. Indian J Community Med 2021; 46(4): 600–605. 10.1101/2021.01.02.21249126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanghera J, Pattani N, Hashmi Y, et al. The impact of SARS‐CoV‐2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health 2020; 62(1): e12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Australian Government Department of Health . Coronavirus (COVID-19) case numbers and statistics. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-case-numbers-and-statistics (accessed 12 December 2021). [Google Scholar]
- 10.Sky News . Melbourne endures world’s longest lockdown. https://www.skynews.com.au/australia-news/coronavirus/melbourne-endures-worlds-longest-lockdown/video/a441003cbf6aa05d1935087f680e7123 (accessed 23 September 2021). [Google Scholar]
- 11.The Royal Melbourne Hospital . Lessons from the second wave: staff come together to reflect on healthcare worker infections. https://www.thermh.org.au/news/lessons-second-wave-staff-come-together-reflect-healthcare-worker-infections (accessed 11 September 2020). [Google Scholar]
- 12.Dhillon RS, Rowin WA, Humphries RS, et al. Aerosolisation during tracheal intubation and extubation in an operating theatre setting. Anaesthesia 2021; 76: 182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dobson H, Malpas CB, Burrell AJC, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry 2021; 29(1): 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahrens KF, Neumann RJ, Kollmann B, et al. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry 2021; 20(1): 140–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond NE, Crowe L, Abbenbroek B, et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers’ depression, anxiety, and stress levels. Aust Crit Care 2021; 34(2): 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kock JHD, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021; 21(1): 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine . Bulletin. https://www.anzca.edu.au/getattachment/2e833c76-d25b-4d98-b6cf-5a19fdb01eb9/ANZCA-Bulletin-Spring-2020 (2021, accessed December 2021). [Google Scholar]
- 18.Adams MA, Brazel M, Thomson R, et al. The mental health of Australian medical practitioners during Covid-19. Australas Psychiatry 2021; 29(5): 523–528. [DOI] [PubMed] [Google Scholar]
- 19.Grafton-Clarke C, Uraiby H, Abraham S, et al. Medical training alongside Covid-19: a qualitative analysis of the junior doctor experience 2021. Epub ahead of print. DOI: 10.21203/rs.3.rs-745131/v1. [DOI] [Google Scholar]
- 20.Beyondblue. Depression. Anxiety . National mental health survey of doctors and medical students. https://www.beyondblue.org.au/docs/default-source/research-project-files/bl1132-report---nmhdmss-full-report_web (accessed 25 January 2020). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-apy-10.1177_10398562221077887 for A longitudinal study of the psychological impact of the COVID-19 pandemic on frontline perioperative healthcare staff in an Australian tertiary public hospital by Irene Ng, Elizabeth Barson, Caroline Fisher, Reny Segal, Daryl L Williams, Roni B Krieser, Paul M Mezzavi, Keat Lee, Yinwei Chen, Teresa Sindoni, Jessica Xu, Karen Lambt and Toni Withiel in Hand Therapy