Abstract
Introduction:
From 1999–2004 to 2011–2014, untreated dental caries prevalence decreased among US children aged 2 to 5 y, regardless of family income. Policies were concurrently initiated for children to increase access to preventive dental services in dental, primary, and community settings and to restorative care in dental settings.
Objectives:
We aimed to examine 1) whether changes in prevalence and severity of untreated and treated caries between the periods varied by family income and 2) to what degree increased past-year dental visit (PYDV) contributed to the changes.
Methods:
We used data for 3,822 children in the National Health and Nutrition Examination Survey 1999 to 2004 and 2011 to 2014. Caries prevalence included prevalence of untreated caries with ≥1 decayed teeth (dt) and prevalence of treated caries with ≥1 filled teeth (ft). Caries severity included number of dt and ft among those with ≥1 dt or ft. We estimated changes in caries outcomes among low- and higher-income children with models—one controlling for sociodemographics and another controlling for sociodemographics and PYDV. Significant changes (P < 0.05) becoming insignificant after controlling for PYDV provide insight on the contribution of PYDV to changes in outcomes.
Results:
Prevalence of untreated caries decreased for low- and higher-income children, with a slightly larger decrease for low-income children; dt decreased only for low-income children; and estimated decreases did not vary by model. An increase in prevalence of treated caries was observed only among low-income children but became minimized and insignificant after controlling for PYDV. Similarly, after controlling for PYDV, the increase in ft among low-income children lost significance, whereas the increase among higher-income children remained.
Conclusion:
Untreated caries among children aged 2 to 5 y declined from 1999–2004 to 2011–2014, with larger declines among low-income children. While changes in PYDV contributed to increases in treated caries, particularly for low-income children, additional factors appear to have contributed to decreased untreated caries.
Keywords: dental utilization, poverty status, child, dental care, public health surveillance, health surveys
Introduction
Dental caries among young children remains a significant public health problem (US Department of Health and Human Services 2000). The costs to treat caries among young children can be substantial if extensive procedures and general anesthesia in a hospital operating room are required (US Department of Health and Human Services 2000; Colak et al. 2013). An analysis of National Health and Nutrition Examination Survey (NHANES) data from 1988–1994 to 1999–2004 found an increase in the prevalence of caries (24% vs. 28%) and no significant change in untreated caries (19% vs. 20%) among US children aged 2 to 5 y (Dye et al. 2007). The lack of improvement in oral health status among young children raised wide attention (Edelstein and Chinn 2009; Tinanoff and Reisine 2009; Shenkin 2011). Some studies hypothesized that the increased caries prevalence may be due to increased access, which may result in earlier receipt of restorations (fillings; Shenkin 2011; Ghazal et al. 2015). Whereas NHANES uses visual-tactile examination to identify cavitated lesions as untreated caries and the presence of restoration as treated caries (Centers for Disease Control and Prevention 2013b), more sensitive diagnostic tools used in a dental office (e.g., radiographs) would identify caries in earlier stages (Burt 1997; Shenkin 2011; Ghazal et al. 2015).
Since 2000, several initiatives have been launched to increase access to preventive and restorative dental care, especially among low-income children. Initiatives aimed at increasing the capacity and demand for care delivered in dental settings included the following. The Health Resources and Services Administration’s oral health service expansion efforts (Institute of Medicine and National Research Council 2011) steadily expanded clinical dental capacity in federally qualified health centers—the number of patients receiving dental services more than tripled, from 1.4 million in 2001 to 4.8 million in 2014 (Health Resources and Services Administration 2008, 2015). Demand for dental care among parents may have also increased due to the following: 1) the Children’s Health Insurance Program Reauthorization Act of 2009, which expanded Medicaid/Children’s Health Insurance Program (CHIP) dental care coverage and increased outreach to parents of children in low-income families (Centers for Medicare & Medicaid Services [CMS] n.d.); 2) a 2003 change in the American Academy of Pediatrics’ recommended age for a child’s first dental visit, from 3 y to 1 y (Hale and American Academy of Pediatrics Section on Pediatric 2003). The CMS Oral Health Initiative, which launched in 2010, likely increased access in dental and primary care settings by using all available dental and medical professionals (CMS 2014). Further stimuli to increasing access in primary care settings were 1) the 2004 US Preventive Services Task Force’s recommendations for primary care clinicians to prescribe oral fluoride supplementation to children aged 6 mo through 5 y who are served by fluoride-deficient water systems (Calonge and U.S. Preventive Services Task Force 2004) and 2) the 2008 American Academy of Pediatrics’ policy statement recommending that pediatricians apply fluoride varnish for patients at risk for caries and without a dental home (American Academy of Pediatrics 2008).
National data from 1999–2004 to 2011–2014 suggest that these national efforts focusing on improving access to preventive dental care provided by dental and primary care providers might have had an impact—the prevalence of dental caries decreased among low-income children aged 2 to 5 y, and prevalence of untreated caries decreased among all children, regardless of income (Dye et al. 2017). These initiatives also likely contributed to the increase in past-year dental use among children from 2000 to 2010 and beyond, particularly among low-income children (Wall et al. 2012; Steinmetz et al. 2014; Nasseh and Vujicic 2015). Our study aimed to examine the contribution of increased dental use on changes in untreated and treated caries prevalence and severity from 1999–2004 to 2011–2014 among low- and higher-income children aged 2 to 5 y. We also examine whether changes in the caries outcomes varied by family income.
Methods
Data Source
We used NHANES data for 2 periods: 1999 to 2004 and 2011 to 2014. NHANES is a cross-sectional survey representative of the noninstitutionalized US population (Centers for Disease Control and Prevention 2013a). Data on health status and risk factors are collected through interviews, health examinations, and laboratory tests. During both periods, dental caries examinations of survey participants aged ≥2 y were conducted by trained and calibrated dentists at the Mobile Examination Center. Cavitated carious lesions (untreated decayed teeth [dt]) and restorations (fillings) were recorded for each primary tooth surface. NHANES 2011 to 2014 and 1999 to 2004 used the same dental caries examination protocol. Details of the NHANES sampling design and oral health protocol are described elsewhere (Centers for Disease Control and Prevention 2013b; National Center for Health Statistics 2013).
Study Population
This study included children aged 2 to 5 y with data for caries outcomes and family poverty status.
Outcome Variables
We assessed changes in untreated and treated dental caries in primary teeth. Prevalence of untreated caries was defined as percentage of population having ≥1 dt and prevalence of treated caries as percentage of population having ≥1 filled teeth (ft). We also examined the severity of untreated and treated caries, including number of dt and ft among children with ≥1 dt or ft.
We assessed untreated and treated caries separately because changes in untreated caries could be attributable to changes in preventive care provided in multiple settings—dentist office, primary care, or community—whereas treated caries could be attributable to treatment provided in dental offices only. Assessing untreated and treated caries outcomes would provide insight on the contribution of increased dental use to changes in caries during the last decade among low- and higher-income children.
Because <25% of children aged 2 to 5 y experienced caries from 2011 to 2014 (Dye et al. 2017), we departed from the usual convention of measuring dt and ft among all children and instead estimated these measures only among children with caries, as this would more accurately reflect the severity among children with the condition.
Main Explanatory Variable
Time was the main explanatory variable and was categorized into 2 periods: 1999 to 2004 and 2011 to 2014.
Covariates
Sociodemographic variables were reported by parents or guardians at the interview. The following categorization of race and ethnicity was used to be comparable between the periods: non-Hispanic White, non-Hispanic Black, Mexican American, and all others (National Center for Health Statistics 2013). Poverty status was defined as the percentage of family income relative to the US Department of Health and Human Services’ federal poverty level (FPL) and was classified into 2 groups: low income (<200% FPL) and higher income (≥200% FPL). Parental education was approximated by the highest education level of the household reference person and his or her spouse and grouped as less than high school, high school graduate, and more than high school. Dental care utilization status was based on past-year dental visit (PYDV) status, defined as having a PYDV (yes/no). Child’s current health insurance status was categorized as Medicaid/CHIP, private insurance or other insurance, and no insurance.
Statistical Analysis
We estimated crude and adjusted (controlling for covariates) caries outcomes for each period for the 2 poverty categories. By using the average marginal prediction (Bieler et al. 2010), we obtained prevalence estimates from binomial regression models and severity estimates from negative binomial regression models. Our models included an interaction term between poverty status and time, which allowed us to assess whether changes in caries over time varied by poverty status.
We calculated changes in crude and adjusted caries outcomes over time by subtracting the value of 1999 to 2004 from the value of 2011 to 2014. T tests were used to test whether these changes were significant and whether changes varied by income.
We specified 2 models to assess the contribution of PYDV to changes in caries outcomes between surveys. The first model, sociodemographic model, adjusted for only sociodemographic variables, including age, sex, race/ethnicity, and household education level. The second model, dental utilization model, included the sociodemographic variables and PYDV. PYDV was considered to contribute to changes in caries if the changes that were significant in the sociodemographic model became insignificant in the dental utilization model. We also assessed multicollinearity of covariates to ensure that multicollinearity was not contributing to changes in outcomes becoming insignificant when we added dental utilization to the sociodemographic variables. There were no covariates with tolerance <0.4, indicating that multicollinearity was not present (Allison 1999).
We also developed 2 sensitivity models. One added health insurance status to the dental utilization model to see if changes from the dental utilization model would be affected with further control for distribution changes in health insurance status. Considering that the same child may have treated and untreated teeth, we conducted a sensitivity model to account for distributions of treated and untreated caries between the periods—specifically, for the treated caries outcome, we added untreated caries to the dental utilization model, and for the untreated caries outcome, we added treated caries to the dental utilization model.
Results were considered statistically significant if P < 0.05. To account for the complex survey design, we used SAS-Callable SUDAAN 11 (RTI International) to estimate prevalence and Stata 13 (StataCorp) to estimate severity. The Mobile Examination Center survey weights were used to account for disproportionate sampling, nonresponse, and poststratification to the US population.
Results
We included 3,822 children aged 2 to 5 y (2,184 from NHANES 1999 to 2004 and 1,638 from NHANES 2011 to 2014) who had complete data for the caries outcomes and poverty status (Table 1).
Table 1.
Population Distribution by Sociodemographic Factors among Low- and Higher-Income Children Aged 2 to 5 y: NHANES, 1999 to 2004 and 2011 to 2014.
| Low Income | Higher Income | |||
|---|---|---|---|---|
| 1999 to 2004 (n = 1,458) |
2011 to 2014 (n = 1,096) |
1999 to 2004 (n = 726) |
2011 to 2014 (n = 542) |
|
| Age, y | ||||
| 2 to 3 | 52.1 | 52.6 | 45.4 | 51.2 |
| 4 to 5 | 48.0 | 47.4 | 54.6 | 48.8 |
| Sex | ||||
| Male | 51.2 | 51.0 | 48.4 | 49.2 |
| Female | 48.8 | 49.0 | 51.6 | 50.8 |
| Race/ethnicity | ||||
| Non-Hispanic White | 46.3 | 39.2 | 72.8 | 68.2 |
| Non-Hispanic Black | 19.6 | 19.5 | 7.5 | 6.8 |
| Mexican American | 18.9 | 21.6 | 7.5 | 8.0 |
| Other | 15.3 | 19.8 | 12.2 | 17.0 |
| Household education level | ||||
| Less than high school | 33.8 | 25.7a | 4.8 | 2.3a |
| High school graduate | 27.5 | 24.9 | 12.2 | 8.1 |
| More than high school | 37.7 | 48.1 | 82.0 | 88.4 |
| Past-year dental visit | ||||
| Yes | 42.2 | 67.2a | 50.7 | 64.4a |
| No | 57.5 | 32.5 | 49.2 | 35.3 |
| Health insurance | ||||
| Medicaid/CHIP | 47.7 | 57.7a | 4.2 | 6.2 |
| Private or other | 38.8 | 35.6 | 92.1 | 88.0 |
| No insurance | 13.4 | 6.6 | 3.8 | 5.4 |
Values are presented as percentages. Poverty status was defined as the percentage of family income relative to the federal poverty level (FPL) and was classified into 2 groups (low income, <200% FPL; higher income, ≥200% FPL).
CHIP, Children’s Health Insurance Program; NHANES, National Health and Nutrition Examination Survey.
Significant at P < 0.05 based on chi-square test to assess if the distribution among categories for each factor changed from 1999–2004 to 2011–2014.
Population distribution changes from 1999–2004 to 2011–2014 were observed for certain covariates (Table 1). The proportions of children with higher household education level and a PYDV significantly increased in the low- and higher-income groups. The PYDV increase was larger for the low-income group (42.2% vs. 67.2%) than the higher-income group (50.7% vs. 64.4%). The proportion of low-income children enrolled in Medicaid/CHIP increased (47.7% vs. 57.7%), and the proportion of uninsured decreased (13.4% vs. 6.6%).
From 2011 to 2014, treated caries prevalence (22.3% vs. 1.9%) and mean ft (3.7 vs. 0.6) were significantly higher among those with PYDV than those without PYDV (results not shown). No significant difference was observed for untreated caries prevalence (11.3% vs. 10.0%), although a significantly lower dt was demonstrated for those with PYDV (1.0 vs. 2.5). A similar pattern was observed for 1999 to 2004.
Decreases in untreated caries prevalence occurred across both income groups with a slightly larger decrease in the low-income group. After controlling for sociodemographic factors and PYDV, the decreases in prevalence of untreated caries remained (low income: 10.0 percentage points, from 22.8% to 12.8%; higher income: 7.7 percentage points, from 15.5% to 7.9%) with essentially no changes as compared with those without control for PYDV (Figure, Table 2). Similarly, the decrease in dt was not affected by PYDV; dt decreased significantly only among low-income children, with a significantly larger decline among low-income children (2.8 vs. 1.3) than among higher-income children (1.8 vs. 1.3).
Figure.
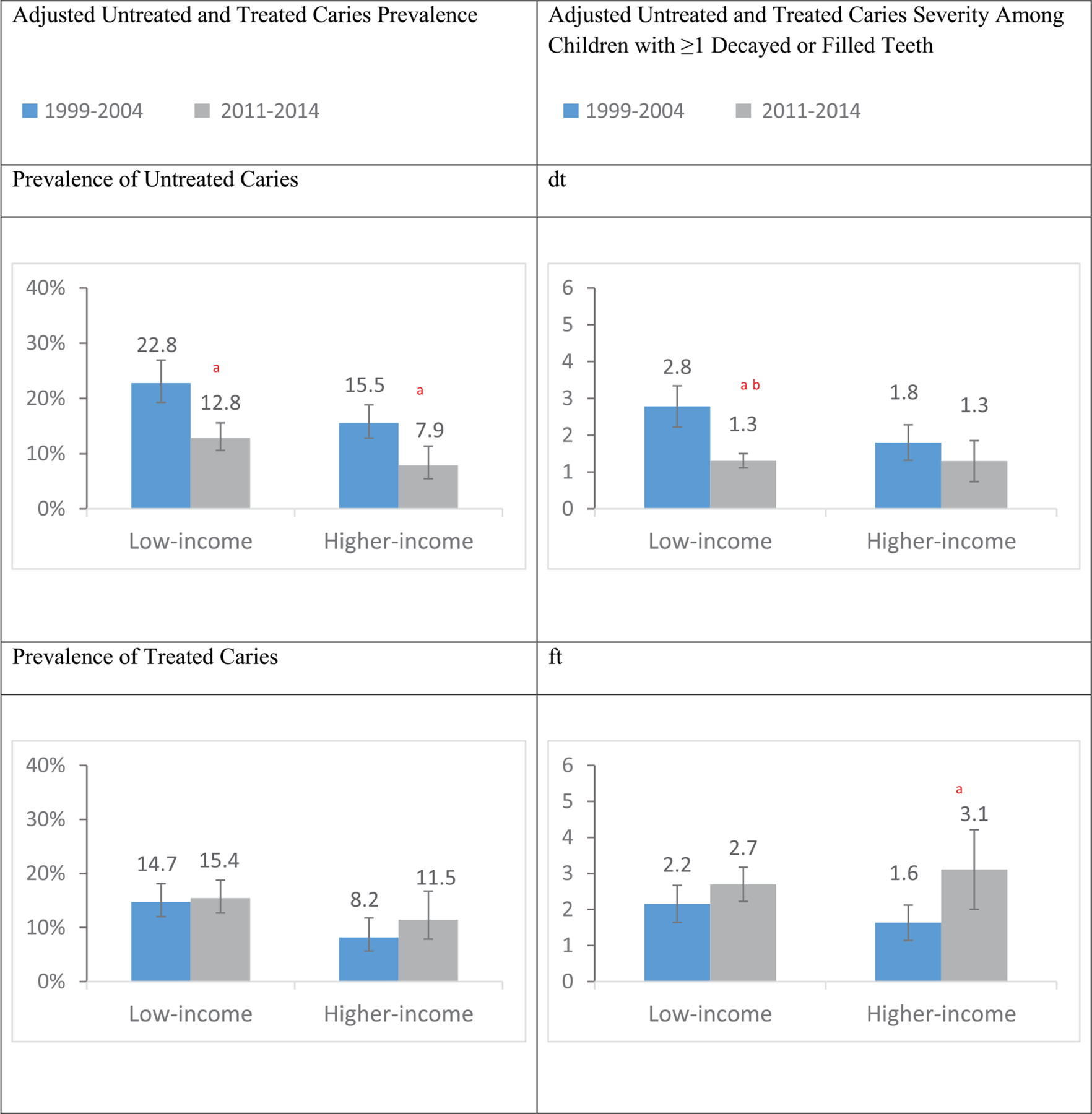
Adjusted untreated and treated dental caries prevalence and severity among children aged 2 to 5 y by poverty status: NHANES 1999 to 2004 and 2011 to 2014.
Adjusted untreated and treated dental caries prevalence and severity: from the dental utilization model with control for sex, age, race/ethnicity, household education level, and past-year dental visit status; error bars represent 95% CIs; severity measures among children with ≥1 decayed or filled primary teeth.
Poverty status was defined as the percentage of family income relative to the federal poverty level (FPL) and was classified into 2 groups (low income, <200% FPL; higher income, ≥200% FPL).
aSignificant change in adjusted untreated and treated caries from 1999–2004 to 2011–2014 at P < 0.05 based on t test.
bChange in adjusted untreated and treated caries from 1999–2004 to 2011–2014 in low-income group significantly differed from that in higher-income group at P < 0.05 based on t test.
dt, number of decayed primary teeth among children with ≥1 decayed or filled teeth; ft, number of filled primary teeth among children with ≥1 decayed or filled teeth; NHANES, National Health and Nutrition Examination Survey.
Table 2.
Crude and Adjusted Changes and 95% CIs in Untreated and Treated Dental Caries Prevalence and Severity by Poverty Status among Children Aged 2 to 5 y: NHANES, 1999 to 2004 and 2011 to 2014.
| Adjusted Changes (95% CI) | |||
|---|---|---|---|
| Variable: Poverty Statusa | Crude Change (95% CI) | Sociodemographic Modelb | Dental Utilization Modelc |
| Prevalence, % | |||
| Untreated caries | |||
| Low income | −12.6 (−17.6, −7.6)d,e | −10.2 (−14.6, −5.7)d | −10.0 (−14.2, −5.7)d |
| Higher income | −6.9 (−10.0, −3.8)d | −7.8 (−11.7, −3.9)d | −7.7 (−11.6, −3.7)d |
| Treated caries | |||
| Low income | 5.6 (1.6, 9.7)d | 5.6 (1.8, 9.3)d | 0.7 (−3.1, 4.5) |
| Higher income | 3.8 (−1.1, 8.8) | 5.4 (−0.5, 11.4) | 3.3 (−2.1, 8.7) |
| Severity among children with ≥1 decayed or filled teeth | |||
| Decayed teeth | |||
| Low income | −1.7 (−2.3 to −1.2)d,e | −1.7 (−2.2 to −1.1)d,e | −1.5 (−2.1 to −0.9)d,e |
| Higher income | −0.6 (−1.2 to 0.1) | −0.7 (−1.4 to 0.1) | −0.5 (−1.3 to 0.2) |
| Filled teeth | |||
| Low income | 1.2 (0.6 to 1.9)d | 1.3 (0.6 to 1.9)d | 0.5 (−0.1 to 1.2) |
| Higher income | 2.0 (0.7 to 3.3)d | 2.1 (0.8 to 3.4)d | 1.5 (0.3 to 2.7)d |
NHANES, National Health and Nutrition Examination Survey.
Poverty status was defined as the percentage of family income relative to the federal poverty level (FPL) and was classified into 2 groups (low income, <200% FPL; higher income, ≥200% FPL).
Adjusted changes in untreated and treated dental caries from 1999–2004 to 2011–2014 from the sociodemographic model, with control for age, sex, race/ethnicity, and household education level.
Adjusted changes in untreated and treated dental caries from 1999–2004 to 2011–2014 from the dental utilization model, controlling for past-year dental visit status in addition to the covariates included in the sociodemographic model.
Crude or adjusted change in untreated and treated caries from 1999–2004 to 2011–2014 was significant at P < 0.05 based on t test.
Crude or adjusted change in untreated and treated caries from 1999–2004 to 2011–2014 in low-income group significantly differed from that in higher-income group at P < 0.05 based on t test.
The pattern for treated caries is the opposite of that for untreated caries. Among low-income children, prevalence of treated caries from crude and sociodemographic models increased by 5.6 percentage points; however, the increase was largely reduced and no longer significant after controlling for PYDV (Table 2). Similar changes were observed in ft among low-income children. For higher-income children, an increase in ft remained after control for past-year dental care use. The addition of health insurance status to the dental utilization model did not affect the changes (results not shown).
Although the same child can have treated and untreated teeth, the percentage of the study population with both treated and untreated caries was low (2.9%), accounting for about one-fifth of those with either treated or untreated caries. The correlation between untreated and treated prevalence measures was also low (r = 0.08). Thus, through the addition of treated caries to the dental utilization model for untreated caries outcomes and the addition of untreated caries to the dental utilization model for treated caries outcomes, the pattern of changes in the caries outcomes from the dental utilization model remained (results not shown).
Discussion
Over this study period, from 1999–2004 to 2011–2014, decreases in untreated caries were larger among low-income children than among higher-income children. The decreases in untreated caries outcomes were not explained by changes in sociodemographics or PYDV. However, the increases in treated caries were largely explained by increased PYDV, especially among low-income children.
Our findings of crude estimates were consistent with the recent publication based on the same NHANES cycles (Dye et al. 2017). Although this study reported age-standardized untreated caries prevalence and its changes over time by poverty status, the analysis did not test whether the change varied by poverty status. Another question remaining is whether changes in multiple sociodemographic factors and dental care use over time accounted for changes in untreated versus treated caries and their variation by poverty status. We took a closer look at changes in untreated and treated caries outcomes individually and used the unique multivariate marginal prediction models that allow assessment of the remaining questions.
Another study including NHANES data from 1999 to 2004 and 2011 to 2014 found no significant difference in income disparity of decayed or filled primary teeth surfaces over time among children aged 2 to 5 y (Slade and Sanders 2017). That study assessed decayed or filled primary teeth surfaces only among total population. Our findings of opposite directions of changes in dt and ft and differed impact of increased PYDV on changes in untreated versus treated caries suggested the need to assess untreated and treated caries outcomes separately. A decrease in dt was among low-income children only, and changes in dt varied by income, indicating changed income disparity over time. Although surface- and tooth-level caries outcomes are not completely comparable, our assessment of dt and ft that was limited to children with caries rather than among all children may provide more comprehensive and sensitive assessment of caries outcomes and their disparities. In addition, in Slade and Sanders’s study (2017), no changes in income disparity for caries over time were based on overlapped confidence intervals. We went beyond this assessment and performed tests that may detect differences or disparities in a more sensitive way.
Our finding that increases in treated caries were largely minimized after controlling for PYDV, particularly among low-income children, may be partially explained by a larger increase in past-year dental care use among low-income children, as found in our study and as reported previously (Wall et al. 2012; Nasseh and Vujicic 2015).
Another consideration for controlling for the increased PYDV should be noted. The criteria used to identify caries in a population-based survey setting and in a dental office setting may differ, although the criteria used in each setting remain the same over time. NHANES serves the purpose of the national public health surveillance system, which requires that data collection be accurate and reliable, as well as timely and highly efficient (Smith et al. 2013). NHANES uses tactile-visual assessment to determine the presence of cavitation as untreated caries and the presence of restorations (fillings) as treated caries (Centers for Disease Control and Prevention 2013b). However, at a dental office visit, additional diagnostic tools, such as radiographs and laser fluorescence, may be used to detect early-stage caries, which then may be filled before tactile-visual assessment could even detect them (Shenkin 2011; Ghazal et al. 2015). Therefore, not like untreated caries based on cavitated lesions detected in a population-based survey, a filled tooth may have noncavitated lesions before the filling, especially when given the increased access to dental care and the potential variation in dentists’ treatment decisions (Burt 1997; Shenkin 2011; Ghazal et al. 2015). Controlling for PYDV may partially adjust for observed increases in treated caries and, eventually, overall caries due to increased dental utilization and different diagnostic criteria used in a population-based survey versus a dental office setting.
Our finding that decreases in untreated caries were not explained by the increase in PYDV is surprising. Several factors should be considered for interpretation of this finding. First, it is possible that the measure of past-year dental care is not sufficiently sensitive to measure receipt and frequency of dental services with evidence of effectiveness in preventing caries. An analysis of 2009 data from the Medical Expenditure Panel Survey found that past-year dental use was 7.6% and 43.7% among children aged 0 to 2 and 3 to 5 y, respectively. The percentage of children receiving a preventive dental service with evidence of effectiveness (i.e., sealants or topical fluoride) was notably lower—1.7% among children aged 0 to 2 y and 17.5% among children aged 3 to 5 y (Griffin et al. 2014). Second, PYDV reported in NHANES is higher than that reported in the Medical Expenditure Panel Survey (Lin et al. 2017). If children who did not have a PYDV were incorrectly classified as having a dental visit, the effect of PYDV would be attenuated. Third, children can receive effective preventive dental services from primary care as well as dental providers. A CMS report highlighted faster growth in the use of preventive dental care (23.2% vs. 42.4%) than in the use of treatment dental care (15.3% vs. 22.9%) from 2000 to 2012 among Medicaid/CHIP-enrolled children (Steinmetz et al. 2014). Very young children are about twice as likely to have visited a medical office than a dental office (Agency for Healthcare Research and Quality 2016). With concerted efforts by multiple sectors at national, state, and local levels, significant progress has been made to integrate preventive dental care into primary care settings among young children, especially among low-income children (Rozier et al. 2003; CMS 2014; US Preventive Services Task Force 2014). The number of state Medicaid programs that reimburse primary care physicians for providing preventive dental services dramatically increased from 1 state in 2000 (North Carolina; Rozier et al. 2003) to 25 in 2008 (Cantrell and National Academy for State Health Policy 2008) and 49 in 2015 (Arthur and Rozier 2016). A recent analysis of CMS-416 data from 2010 to 2013 indicated that although the percentage of Medicaid-enrolled children aged 0 to 5 y receiving preventive dental services through primary care settings was low (4.3%), it had increased over time (Arthur and Rozier 2016).
Our study is subject to several limitations. First, our study was not designed to directly evaluate the impact of the concurring national initiatives to improve access to dental care. Second, past-year dental care use was reported by parents or caregivers and might be subject to recall bias. However, given that the same dental visit question was asked in both periods, we do not expect the recall bias to change significantly and thus affect the changes in caries between the periods. Third, selection bias might exist because the dental use measure did not capture the type and extent of services provided and very young children may be more likely to visit dentists for treatment purpose. Fourth, missing primary teeth were not included in the NHANES protocol, because of the difficulty in determining whether a missing primary tooth was the result of dental caries, trauma, or natural exfoliation (Centers for Disease Control and Prevention 2013b). The degree of underestimation of caries burden due to this limitation might be larger among lower-income children than high-income children if the former would be more likely to have a tooth extraction versus a (sometimes more costly) restoration.
Despite its limitations, our study has several strengths. First, NHANES is the only national data source that has been used to monitor trends in oral health status based on clinical examination in the US population. The NHANES 2011 to 2014 and 1999 to 2004 uniquely covered the period when major national initiatives were launched to improve dental care access and oral health status, particularly among low-income children. As expected, we observed declines in untreated caries among children between the study periods, with larger declines observed among low-income children. Second, our study appears to be the first to apply the model-based approach to assess the potential contribution of increased dental care use to the changes in dental caries over time and their variations by poverty status. Finally, instead of focusing on caries severity in the total population, as commonly reported, we assessed caries severity among children with caries, which provided a more specific assessment of severity.
In conclusion, untreated dental caries prevalence and severity among US children aged 2 to 5 y declined from 1999–2004 to 2011–2014, with larger declines observed among low-income children, but these decreases were not associated with the increase in PYDV. The increases in treated caries were associated with increased past-year dental care use, particularly among low-income children. While changes in PYDV contributed to increases in treated caries, especially for low-income children, additional factors appear to have contributed to decreased untreated caries.
Knowledge Transfer Statement:
For young children, the degree and direction of changes in caries over the last decade varied by outcome measure (e.g., untreated or treated) and family poverty status. Examining the effect of increased dental utilization on changes in untreated and treated caries outcomes can help identify those policies that contribute to changes in these outcomes and highlight the potential role of the different caries assessment criteria used in dental offices versus those in a population-based survey.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Agency for Healthcare Research and Quality. 2016. MEPSnet/HC trend query [accessed 2017 Jun 16]. https://meps.ahrq.gov/mepsweb/data_stats/MEPSnetHC/startup.
- Allison PD. 1999. Logistic regression using the SAS system: theory and application. Cary (NC): SAS Institute Inc. [Google Scholar]
- American Academy of Pediatrics, Section on Pediatric Dentistry and Oral Health. 2008. Preventive oral health intervention for pediatricians. Pediatrics. 122(6):1387–1394. [DOI] [PubMed] [Google Scholar]
- Arthur T, Rozier RG. 2016. Provision of preventive dental services in children enrolled in Medicaid by nondental providers. Pediatrics. 137(2):e20153436. [DOI] [PubMed] [Google Scholar]
- Bieler GS, Brown GG, Williams RL, Brogan DJ. 2010. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 171(5):618–623. [DOI] [PubMed] [Google Scholar]
- Burt BA. 1997. How useful are cross-sectional data from surveys of dental caries? Community Dent Oral Epidemiol. 25(1):36–41. [DOI] [PubMed] [Google Scholar]
- Calonge N, US Preventive Services Task Force. 2004. Prevention of dental caries in preschool children: recommendations and rationale. Am J Prev Med. 26(4):326–329. [DOI] [PubMed] [Google Scholar]
- Cantrell C, National Academy for State Health Policy. 2008. The role of physicians in children’s oral health. State Health Policy Monitor. 2(5):1–5. [Google Scholar]
- Centers for Disease Control and Prevention. 2013a. About the National Health and Nutrition Examination Survey [accessed 2017 Feb 10]. http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- Centers for Disease Control and Prevention. 2013b. National Health and Nutrition Examination Survey (NHANES)— oral health examiners manual 2013–2014 [accessed 2016 Sep 2]. https://www.cdc.gov/nchs/data/nhanes/nhanes_13_14/Oral_Health_Examiners.pdf.
- Centers for Medicare & Medicaid Services. 2014. Update on CMS Oral Health Initiative and other oral health related items [accessed 2017 Feb 10]. https://www.medicaid.gov/federal-policy-guidance/downloads/cib-07-10-2014.pdf.
- Centers for Medicare & Medicaid Services. n.d. CHIPRA [accessed 2017 Feb 10]. https://www.medicaid.gov/chip/chipra/chipra.html.
- Colak H, Dulgergil CT, Dalli M, Hamidi MM. 2013. Early childhood caries update: a review of causes, diagnoses, and treatments. J Nat Sci Biol Med. 4(1):29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. 2017. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014. J Am Dent Assoc. 148(8):550–565.e7. [DOI] [PubMed] [Google Scholar]
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, Eke PI, Beltran-Aguilar ED, Horowitz AM, Li CH. 2007. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. (248):1–92. [PubMed] [Google Scholar]
- Edelstein BL, Chinn CH. 2009. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr. 9(6):415–419. [DOI] [PubMed] [Google Scholar]
- Ghazal T, Levy SM, Childers NK, Broffitt B, Cutter GR, Wiener HW, Kempf MC, Warren J, Cavanaugh JE. 2015. Factors associated with early childhood caries incidence among high caries-risk children. Community Dent Oral Epidemiol. 43(4):366–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Barker LK, Wei L, Li CH, Albuquerque MS, Gooch BF, Centers for Disease Control and Prevention. 2014. Use of dental care and effective preventive services in preventing tooth decay among US Children and adolescents—Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010. MMWR Suppl. 63(2):54–60. [PubMed] [Google Scholar]
- Hale KJ, American Academy of Pediatrics Section on Pediatric Dentistry. 2003. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 111(5 Pt 1):1113–1116. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration. 2008. Bureau of Primary Health Care Section 330 grantees Uniform Data System (UDS)—calendar year 2007 data national rollup report [accessed 2017 Jan 5]. https://bphc.hrsa.gov/datareporting/nationaldata/2007/2007_nat_uds_summary.pdf.
- Health Resources and Services Administration. 2015. Health center data and reporting—2014 health center profile [accessed 2017 Jan 5]. https://bphc.hrsa.gov/datareporting/index.html.
- Institute of Medicine, National Research Council. 2011. Improving access to oral health care for vulnerable and underserved populations [accessed 2017 May 10]. http://www.nationalacademies.org/hmd/Reports/2011/Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations.aspx.
- Lin M, Li CH, Wei L, Naavaal S, Kolavic Gray S, Manz MC, Barker L. 2017. Prevalence of past-year dental visit among US adults, 1999–2010: comparison of trends and estimates between the Behavioral Risk Factor Surveillance System and three national surveys. J Public Health Dent. 77(2):105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasseh K, Vujicic M. 2015. Dental care utilization rate continues to increase among children, holds steady among workingage adults and the elderly. Health Policy Institute research brief. American Dental Association; [accessed 2017 May 10]. http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1015_1.ashx. [Google Scholar]
- National Center for Health Statistics. 2013. National Health and Nutrition Examination Survey: analytic guidelines, 2011–2012 [accessed 2016 Sep 2]. http://www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf.
- Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. 2003. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ. 67(8):876–885. [PubMed] [Google Scholar]
- Shenkin JD. 2011. An increase in caries rate or an increase in access to care: data show mixed results. J Public Health Dent. 71(1):1–5. [DOI] [PubMed] [Google Scholar]
- Slade GD, Sanders AE. 2017. Two decades of persisting income-disparities in dental caries among US children and adolescents. J Public Health Dent [epub ahead of print 2017 Dec 15] in press. doi: 10.1111/jphd.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PF, Hadler JL, Stanbury M, Rolfs RT, Hopkins RS, Group CSS. 2013. “Blueprint version 2.0”: updating public health surveillance for the 21st century. J Public Health Manag Pract. 19(3):231–239. [DOI] [PubMed] [Google Scholar]
- Steinmetz E, Bruen B, Ku L. 2014. Children’s use of dental care in Medicaid: federal fiscal years 2000–2012 [accessed 2018 Mar 2]. https://www.medicaid.gov/medicaid/benefits/downloads/dental-trends-2000-to-2012.pdf.
- Tinanoff N, Reisine S. 2009. Update on early childhood caries since the Surgeon General’s report. Acad Pediatr. 9(6):396–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. 2000. Oral health in America: a report of the Surgeon General. Rockville (MD): National Institutes of Health. [Google Scholar]
- US Preventive Services Task Force. 2014. Final recommendation statement: dental caries in children from birth through age 5 years. Screening [accessed 2017 Feb 13]. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/dental-caries-in-children-from-birth-through-age-5-years-screening. [DOI] [PubMed]
- Wall TP, Vujicic M, Nasseh K. 2012. Recent trends in the utilization of dental care in the United States. J Dent Educ. 76(8): 1020–1027. [PubMed] [Google Scholar]


