Abstract
Objective:
Psychiatric disorders increase risk for contracting coronavirus disease 2019 (COVID-19), but we know little about relationships between psychiatric symptoms and COVID-19 risky and protective behaviors. Posttraumatic stress disorder (PTSD) has been associated with increased propensity to engage in risky behaviors, but may also be associated with increased COVID-19 protective behaviors due to increased threat sensitivity and social isolation.
Methods:
We examined associations of PTSD symptoms with COVID-19-related protective and risky behaviors using data from a cross-sectional online US study among 845 US adults in August-September 2020. PTSD symptoms (PTSD Checklist-5), socio-demographics, COVID-19-related experiences and vulnerabilities, and past 30-day engagement in ten protective and eight risky behaviors for COVID-19 were assessed via self-report. We examined associations between PTSD symptoms and COVID-19 protective and risky behaviors with linear regressions, adjusting for covariates.
Results:
Probable PTSD and higher PTSD symptom severity were associated with greater engagement in protective behaviors, but also greater engagement in risky behaviors. Associations were only slightly attenuated by adjustment for COVID-19 exposures and perceived likelihood and severity of COVID-19. Associations varied by PTSD clusters: intrusions and arousal were associated with both more protective and more risky behaviors, whereas negative cognitions/mood was associated only with more risky, and avoidance only with more protective, behaviors.
Conclusion:
Higher PTSD symptoms were associated with engagement in more protective but also more risky behaviors for COVID-19. Mental health should be considered in the design of public health campaigns dedicated to limiting infectious disease spread.
Keywords: COVID-19, mental health, posttraumatic stress disorder, protective behaviors, risky behaviors
Individual behaviors are key to both individual and population health, and have become even more critical during the coronavirus disease 2019 (COVID-19) pandemic as behavioral strategies have been a key defense against infection spread (Centers for Disease Control and Prevention, 2020a). Since the beginning of the COVID-19 outbreak, individuals in most countries worldwide have been advised to sustain engagement in protective behaviors (e.g., mask wearing, hand sanitizing) and avoid engagement in risky behaviors (e.g., socializing indoors, taking flights). Pre-pandemic studies have linked posttraumatic stress disorder (PTSD) with engagement in more risky and fewer protective health behaviors (Feldner et al., 2007; Kronish et al., 2012). Thus, we might expect that individuals with PTSD would be at heightened risk for COVID-19 due to engagement in more risky and fewer protective behaviors against infection. However, PTSD has also been linked with increased threat sensitivity (Ehlers & Clark, 2000; Lanius et al., 2017; Olatunji et al., 2013) and greater social isolation (King et al., 2006), which may enhance adherence to COVID-19 behavioral restrictions. Multiple structural and environmental factors may also influence risk for PTSD as well as engagement in protective and risky behaviors (Golden & Earp, 2012). Understanding patterns of COVID-related protective and risky behaviors associated with PTSD symptoms is important to inform ongoing prevention efforts for COVID-19 and future prevention efforts for other diseases.
Accumulating research indicates that PTSD is associated with an increased propensity to engage in risky health behaviors, including smoking, alcohol and substance use, dangerous driving, and risky sexual behaviors for contracting HIV (Kronish et al., 2012; Reisner et al., 2009; van den Berk-Clark et al., 2018). Some evidence suggests that PTSD may also be associated with lower engagement in protective health behaviors, such as medication adherence and physical activity, although findings are not entirely consistent (Hall et al., 2015; Lee & Park, 2018). For example, individuals with PTSD have lower physical activity levels and lower medication adherence, but PTSD is not consistently associated with maintaining a healthy diet (Kronish et al., 2012; Lee & Park, 2018; van den Berk-Clark et al., 2018). Most studies focus on general health behaviors, rather than risky/protective behaviors amid infectious epidemics. However, one study during the Ebola epidemic in Sierra Leone found that individuals with PTSD were less likely to engage in protective (e.g., seeking prevention information from community leaders) and more likely to engage in risky (e.g., treating symptomatic individuals with hot salt water bath) behaviors for Ebola (Betancourt et al., 2016), suggesting a link between PTSD and epidemic-related behaviors in some contexts.
Although PTSD has been linked with decreased protective and increased risky health behaviors in general, some PTSD symptoms may facilitate protective behaviors during a pandemic. First, PTSD has been linked with heightened threat sensitivity (Ehlers & Clark, 2000; Lanius et al., 2017; Olatunji et al., 2013), conceptualized as both heightened reactivity and more avoidance of threat, which could increase engagement in protective behaviors against COVID-19. For example, in a study including men who have sex with men, hyperarousal symptoms were associated with lower rates of risky sexual behavior (Choi et al., 2017). Thus, people with PTSD may perceive COVID-19 as more threatening, which may increase their motivation to protect themselves against the disease. Second, PTSD has been linked with increased social isolation (King et al., 2006), which could increase ease of adoption of social distancing in the context of COVID-19. However, other studies have indicated lower levels of subjective but not objective social support in PTSD (Ahmadian et al., 2020). Thus, it is possible that PTSD could be associated with more or less risky behavioral patterns against COVID-19, depending on the specific behaviors assessed. Further, given the heterogeneous nature of PTSD (Galatzer-Levy & Bryant, 2013), it is possible that different symptom clusters of PTSD (i.e., intrusions, avoidance of trauma-related stimuli, negative alterations in cognition and mood, and alterations in arousal and reactivity), may be differentially associated with specific behaviors during the pandemic. However, few studies have examined the effects of PTSD symptoms, or PTSD symptoms clusters, on a range of protective and risky behaviors concurrently.
In this study, we examined cross-sectional associations between self-reported PTSD symptoms and a range of protective and risky behaviors for COVID-19 in a trauma-enriched sample of individuals from across the United States. We hypothesized that higher levels of PTSD symptoms (both probable PTSD as defined by the clinical cutoff (Bovin et al., 2016) and higher symptom severity) would be associated with both increased protective and increased risky behaviors, relative to lower levels of PTSD symptoms. In secondary analyses, we examined associations of each PTSD symptom cluster with protective and risky behaviors. Given that direct experiences with COVID-19 and perceived risk of COVID-19 have been associated with increases in protective behaviors (de Bruin & Bennett, 2020; Makhanova & Shepherd, 2020), we also examined associations of PTSD symptoms with COVID-19 exposure-related experiences (e.g., having a COVID-19 test, COVID-19 diagnosis), perceived likelihood of contracting COVID-19, and expected severity of COVID-19 if contracted and adjusted for these in follow-up models, hypothesizing that associations between PTSD symptoms and behaviors would be attenuated.
Materials and Methods
Study Sample
Study participants included community-dwelling adults (>18 years) currently residing in the US who engaged in prior research related to trauma exposure. Participants were individuals who had indicated interest in participating in remote research related to trauma and PTSD in 2017–2018 (Niles et al., 2020). Specifically, 3,631 individuals self-selected into the 2017–2018 cohort if they identified as “suffering from anxiety or stress resulting from exposure to a traumatic event”; 52.0% of respondents met criteria for probable PTSD at that time (see Supplemental Table 1). Invitations for the current study were emailed to all 3,631 individuals who were asked to provide electronic consent to participate in the current study. Consenting individuals were directed to a 30-minute online Qualtrics survey that assessed psychological experiences during the COVID-19 pandemic. Individuals received a $5 Amazon e-gift card upon completing the full survey. Of the 3,631 individuals contacted, 1,000 started the survey and among these, 1 did not consent, 78 stopped the survey prior to consenting, and 25 did not complete at least the demographic information at the beginning of the survey, resulting in an eligible sample of 896 (24.7% response rate) participants between August 4-September 19, 2020. We primarily conducted complete case analysis including 845 (94.3% of the eligible sample, N = 896) participants with full information on all relevant variables, and all data used in the current analyses came from the COVID-19 survey. This study was approved and conducted in compliance with the Institutional Review Board at the University of California, San Francisco.
Measures
Independent Variables
Trauma Exposure and PTSD Symptoms.
Lifetime trauma exposure was assessed with a modified version of the Trauma History Screen (THS) (Carlson et al., 2011), which asked participants to report if they had experienced 17 potentially traumatic events. The THS includes 14 potentially traumatic events and one other trauma not specified, and we included two additional events: experiencing a life-threatening illness; and serious injury, harm, or death you caused to someone else. Past month PTSD symptom severity in relation to one’s worst trauma was assessed with the PTSD Checklist-5 (PCL-5) (Weathers et al., 2013). The PCL-5 is a widely used self-report measure of PTSD symptoms in adults with sound psychometric properties (Bovin et al., 2016). Individuals rated the severity of 20 symptoms covering four Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) criteria clusters on a five-point scale (0 = not at all to 4 = extremely). Total symptom severity scores were derived by summing across 20 items (potential range 0–80), and the scale had excellent internal consistency reliability in our sample (α = 0.96). We used a PCL-5 total score of ≥ 33 to define the presence of probable PTSD. Previously, Bovin et al. (2016) found that a total PCL-5 score of 33 exhibited high sensitivity (0.88), specificity (0.69), efficiency (0.80), positive predictive value (0.81), and negative predictive value (0.78) when compared with the results of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) (Weathers et al., 2013). This cutoff score has been used in numerous studies with various samples, including general community samples recruited online (van Stolk-Cooke et al., 2018) and university students (Contractor et al., 2018). To examine symptom clusters, we created separate subscale sum scores for each symptom cluster: intrusions; avoidance of trauma-related stimuli; negative alterations in cognition and mood; and alterations in arousal and reactivity.
Dependent Variables
COVID-19 Protective and Risky Behaviors.
Individuals reported the frequency of engagement in 18 behaviors in the past 30 days on a 5-point scale: 0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = always. Behaviors included ten protective behaviors (e.g., washing hands, maintaining six-foot distance, mask wearing, isolating oneself) and eight risky behaviors (e.g., attending event with a large crowd, taking a flight for vacation, going to indoor restaurants or bars). To confirm our a priori groupings of protective and risky behaviors in our newly developed measure, we examined the underlying latent structure with a confirmatory factor analysis (CFA) using the cfa function in R (Rosseel, 2012). The CFA produced an adequate fit, providing statistical support that our designations of COVID-19-related protective and risky behaviors were consistent with these data (see Confirmatory Factor Analysis in Supplement for details) (Hu & Bentler, 1999).
Perceptions of COVID-19 Protection.
To capture participants’ perceived approach to protection against COVID-19, individuals reported how frequently in the past 30 days they acted more cautiously than others in their community (0 = never to 4 = always), and their overall approach to protecting themselves from contracting COVID-19 on a six-point scale (i.e., extremely relaxed, relaxed, fairly relaxed, fairly cautious, cautious, extremely cautious).
Covariates
COVID-19 Exposure-Related Experiences and Vulnerabilities.
Experiences that might have occurred since the pandemic began included having: had a COVID-19 test (yes/no); been in quarantine, defined as completely isolating oneself to avoiding spreading COVID-19 (yes/no); had COVID-19 (yes, diagnosed based on a COVID-19 test; probably yes, diagnosed by a clinician without a COVID-19 test; maybe, suspected COVID-19; no, did not have COVID-19); and conditions that make one vulnerable to COVID-19 (yes/no), including body weight (normal weight, underweight, overweight, obese; those overweight and obese were considered vulnerable). Individuals also reported whether someone in their household had COVID-19 (yes, someone was diagnosed based on a COVID-19 test; probably yes, someone was diagnosed by a clinician without a COVID-19 test; maybe, someone experienced symptoms of COVID-19; no, nobody had COVID-19), whether they know anyone who has had COVID-19 (yes/no), and whether they provide COVID-19 care in employment (direct care, supportive care, does not provide COVID-19 care). Individuals reported on the likelihood that they would contract COVID-19 in the next year (1 = very unlikely, 2 = unlikely, 3 = neutral, 4 = likely, 5 = very likely) and the severity of their symptoms if contracted (1 = absent, 2 = mild, 3 = moderate, 4 = severe, 5 = extreme).
Socio-demographic Covariates.
Covariates were all self-reported and represent potential confounders between PTSD symptoms and COVID-19-related behaviors. Demographic variables included age (continuous in years), gender, and race/ethnicity (Non-Hispanic White, Black, Asian, Latinx, other or more than one race). Socio-economic variables included educational attainment, current employment status, and household income. Family and residential variables included marital status, living situation, residential area type, and US Census Bureau region of residence. See Table 1 for levels of categorical covariates.
Table 1.
Socio-demographic Covariates and COVID-19 Experiences and Vulnerabilities by Probable PTSD Status (N = 845)
| No/Low PTSD (n = 569, 67.3%) |
Probable PTSD (n = 276, 32.7%) | T-test or χ2 Value | ||||||
|---|---|---|---|---|---|---|---|---|
| Covariate | N | % | N | % | N | % | ||
| Age (M (SD)), in years | 36.95 | 11.0 | 37.50 | 11.2 | 35.82 | 10.5 | 2.09* | |
| Gender | Man | 169 | 20.0 | 120 | 21.1 | 49 | 17.8 | 12.08** |
| Woman | 655 | 77.5 | 442 | 77.7 | 213 | 77.2 | ||
| Non-Binary, Transgender, Other | 21 | 2.5 | 7 | 1.2 | 14 | 5.1 | ||
| Race/Ethnicity | Non-Hispanic White | 495 | 58.6 | 336 | 59.1 | 159 | 57.6 | 0.91 |
| Black | 114 | 13.5 | 76 | 13.4 | 38 | 13.8 | ||
| Asian | 79 | 9.3 | 52 | 9.1 | 27 | 9.8 | ||
| Latinx | 86 | 10.2 | 60 | 10.5 | 26 | 9.4 | ||
| Other Race or More Than One Race | 71 | 8.4 | 45 | 7.9 | 26 | 9.4 | ||
| Educational Attainment | High School or Less | 79 | 9.3 | 48 | 8.4 | 31 | 11.2 | 1.99 |
| Some College/2-yr College Degree | 234 | 27.2 | 156 | 27.4 | 78 | 28.3 | ||
| 4-yr College Degree or Grad School | 532 | 63.0 | 365 | 64.1 | 167 | 60.5 | ||
| Current Employment Status | Employed Full Time | 470 | 55.6 | 328 | 57.6 | 142 | 51.4 | 17.14** |
| Employed Part Time | 129 | 15.3 | 88 | 15.5 | 41 | 14.9 | ||
| Unemployed | 177 | 20.9 | 99 | 17.4 | 78 | 28.3 | ||
| Student | 34 | 4.0 | 29 | 5.1 | 5 | 1.8 | ||
| Retired | 19 | 2.2 | 14 | 2.5 | 5 | 1.8 | ||
| Furloughed | 16 | 1.9 | 11 | 1.9 | 5 | 1.8 | ||
| Annual Household Income | ≤$50,000 per year | 352 | 41.7 | 220 | 38.7 | 132 | 47.8 | 7.73+ |
| $50,001–$100,000 per year | 334 | 39.5 | 235 | 41.3 | 99 | 35.9 | ||
| $100,001–$150,000 per year | 102 | 12.1 | 70 | 12.3 | 32 | 11.6 | ||
| >$150,000 per year | 57 | 6.7 | 44 | 7.7 | 13 | 4.7 | ||
| Marital status | Married | 283 | 33.5 | 201 | 35.3 | 82 | 29.7 | 6.91+ |
| Single, In a Relationship | 253 | 29.9 | 176 | 30.9 | 77 | 27.9 | ||
| Single, No Relationship | 243 | 28.8 | 154 | 27.1 | 89 | 32.2 | ||
| Separated/Divorced/Widowed | 66 | 7.8 | 38 | 6.7 | 28 | 10.1 | ||
| Living Situation | Living Alone | 185 | 21.9 | 121 | 21.3 | 64 | 23.2 | 0.40 |
| Living with Others | 660 | 78.1 | 448 | 78.7 | 212 | 76.8 | ||
| Residential Area Type | Urban | 431 | 51.0 | 286 | 50.3 | 145 | 52.5 | 2.85 |
| Suburban | 298 | 35.3 | 208 | 36.6 | 90 | 32.6 | ||
| Town | 65 | 7.7 | 39 | 6.9 | 26 | 9.4 | ||
| Rural | 51 | 6.0 | 36 | 6.3 | 15 | 5.4 | ||
| Region of Residence | West | 277 | 32.8 | 190 | 33.4 | 87 | 31.5 | 0.52 |
| Midwest | 139 | 16.4 | 95 | 16.7 | 44 | 15.9 | ||
| Northeast | 167 | 19.8 | 111 | 19.5 | 56 | 20.3 | ||
| South | 262 | 31.0 | 173 | 30.4 | 89 | 32.2 | ||
| Had a COVID-19 Test | Yes | 275 | 32.5 | 187 | 32.9 | 88 | 31.9 | 0.08 |
| Quarantined | Yes | 260 | 30.8 | 159 | 27.9 | 101 | 36.6 | 6.53* |
| Had COVID-19 | Yes, diagnosed with test | 12 | 1.4 | 7 | 1.2 | 5 | 1.8 | 11.65** |
| Probably, diagnosed without test | 9 | 1.1 | 3 | 0.5 | 6 | 2.2 | ||
| Maybe, suspected COVID-19 | 135 | 16.0 | 79 | 13.9 | 56 | 20.3 | ||
| No, did not have COVID-19 | 689 | 81.5 | 480 | 84.4 | 209 | 75.7 | ||
| Vulnerable Conditions | Yes | 286 | 33.8 | 173 | 30.4 | 113 | 40.9 | 9.22** |
| Body Weight | Normal Weight | 430 | 50.9 | 305 | 53.6 | 125 | 45.3 | 5.18 |
| Underweight | 37 | 4.4 | 23 | 4.0 | 14 | 5.1 | ||
| Overweight | 337 | 39.9 | 215 | 37.8 | 122 | 44.2 | ||
| Obese | 41 | 4.9 | 26 | 4.6 | 15 | 5.4 | ||
| COVID-19 in a Household Member | Yes, diagnosed with test | 28 | 3.3 | 18 | 3.2 | 10 | 3.6 | 11.50** |
| Probably, diagnosed without test | 6 | 0.7 | 1 | 0.2 | 5 | 1.8 | ||
| Maybe, suspected COVID-19 | 80 | 9.5 | 46 | 8.1 | 34 | 12.3 | ||
| No, did not have COVID-19 | 731 | 86.5 | 504 | 88.6 | 227 | 82.2 | ||
| Know Those with COVID-19 | Yes | 511 | 60.5 | 331 | 58/2 | 180 | 65.2 | 3.86+ |
| COVID-19 Care in Employment | Provides Direct COVID-19 Care | 35 | 4.1 | 25 | 4.4 | 10 | 3.6 | 2.22 |
| Provides Supportive COVID-19 Care | 53 | 6.3 | 31 | 5.4 | 22 | 8.0 | ||
| Does Not Provide COVID-19 Care | 757 | 89.6 | 513 | 90.2 | 244 | 88.4 | ||
Note. Probable PTSD = PCL-5 scores ≥ 33. Other Race is Native Hawaiian, Pacific Islander, American Indian, Alaska Native, and Middle Eastern
p < .01,
p < .05,
p < .10 for t-tests (age) and χ2 tests of independence (categorical covariates) by PTSD
Statistical Analyses
We examined overall distributions of PTSD symptoms, COVID-19 experiences and vulnerabilities, protective and risky behaviors, and covariates. We also examined the distribution of covariates and COVID-19 experiences and vulnerabilities by probable PTSD status.
Our primary analytic models examined associations between PTSD symptoms (binary cutoff and total severity score, separately) and average frequency of engagement in COVID-19 protective and risky behaviors, and all behaviors combined, adjusting for covariates. Specifically, we ran linear regression models for associations between PTSD symptoms and derived composite variables of the mean frequency across ten protective behaviors (coded 0 = never to 4 = always), mean frequency across eight risky behaviors (coded 0 = never to 4 = always), and mean frequency across all 18 behaviors (protective behaviors coded 0 = never to 4 = always and risky behaviors reverse coded as 4 = never to 0 = always; higher levels indicate more favorable/healthy behavior). For all models, we first adjusted for socio-demographic covariates (Model 1), then additionally adjusted for COVID-19 experiences and vulnerabilities and perceived likelihood and severity of COVID-19 (Model 2). PTSD symptoms were standardized (M = 0, SD = 1) to improve interpretability. Given the multiple analyses conducted, P-value were corrected by the Benjamini–Hochberg false discovery rate (FDR) procedure for associations between each primary predictor (i.e., probable PTSD, PTSD symptoms) and all outcomes (i.e., average protective, risky, and all behaviors, and 18 individual behaviors). All p-values presented for analytic models are FDR corrected.
In exploratory secondary models, we ran individual linear regressions for associations between PTSD symptoms and the frequency of each individual behavior separately as continuous variables. Linear regressions were also conducted for associations between PTSD symptoms and perceptions of behaviors (i.e., frequency of acting more cautious than their community, and overall approach to protecting themselves). Finally, we reran primary models for associations between each PTSD cluster subscale (standardized) and averaged behaviors separately to examine whether specific symptom clusters were more strongly associated with COVID-19-related behaviors.
We conducted several sensitivity analyses to: 1) address missing data using multiple imputation (Rubin, 2004; Van Buuren et al., 2006); 2) explore if our results held in a sample excluding individuals with short survey completion time, which may indicate inattention (Curran, 2016), or IP addresses outside the US, which could be due to either the use of a VPN or to actual location outside the US; 3) incorporate DSM-5 diagnostic criteria; and 4) examine associations of depression and anxiety (assessed with the 21-item Depression Anxiety Stress Scale (Antony et al., 1998), an abbreviated version of the DASS-42 (Lovibond & Lovibond, 1995)) with COVID-19 behaviors. See Measures and Analyses in Supplement for more details. All analyses were conducted in R, version 4.0.2.
Results
The analytic sample had a majority of participants identify as female (77.5% were women) with a mean age of 37.0 (SD = 11.0) and was relatively diverse with respect to race/ethnicity (58.6% identified as Non-Hispanic white, 13.5% as black/African American, 9.3% as Asian, 10.2% as Latinx, and 8.4% as other race or more than one race) (Table 1). Participants tended to be more highly educated than the general US population, with 63.0% having a 4-year college degree or more, but there was a varied distribution of income and current employment status.
Among the sample, 32.5% reported having a COVID-19 test and 30.8% reported having quarantined since the pandemic began (Table 1). In line with overall US population COVID-19 prevalence of 2.1% by September 19, 2020 (Centers for Disease Control and Prevention, 2020b), a small proportion of our participants reported having already had COVID-19, with 1.4% diagnosed with, and 1.1% diagnosed without, a test. A larger proportion (16.0%) reported a suspicion of having had COVID-19. A third of the sample (33.8%) reported having a condition making them vulnerable to COVID-19, and 39.9% identified as overweight and 4.9% as obese. Regarding likelihood of contracting COVID-19, 37.5% reported their likelihood as unlikely or very unlikely, 45.4% responded neutrally, and 17.1% reported it was likely or very likely. When asked about potential symptom severity if they contracted COVID-19, 13.0% expected that they would not have symptoms, 30.4% expected mild symptoms, 42.4% expected moderate symptoms, 11.4% expected severe symptoms, and 2.8% expected extreme symptoms.
Trauma Exposure and PTSD Symptoms
Most of the sample (n = 677, 80.3%) experienced at least one lifetime trauma, with many reporting multiple lifetime traumas: 10.4% of the sample reported two, 14.3% reported three, and 43.3% reported four or more traumatic event types. A total of 276 (32.7%) individuals met criteria for probable PTSD (≥ 33 PCL-5 severity scores). The mean PCL-5 score was 24.5 (SD = 20.0) ranging from a low of 0 to a high of 80.
Individuals with probable PTSD had a mean PCL-5 score of 48.7 (SD = 11.6) and were younger, more likely to be non-binary, transgender, or other gender, more likely to be unemployed, had marginally lower household income, and were marginally less likely to be married or in a relationship compared to those scoring below the clinical cutoff for probable PTSD. Individuals with probable PTSD were more likely to report that they had quarantined, been diagnosed with or suspected to have had COVID-19, to have conditions making them vulnerable to COVID-19, to have a diagnosed or suspected COVID-19 infection in their household, and to know others with COVID-19, compared to those scoring below the clinical cutoff (Table 1).
PTSD Symptoms and COVID-19 Protective and Risky Behaviors
Average Protective and Risky Behaviors
The average engagement frequency across ten protective behaviors was 2.73 (SD = 0.7), which reflects between “sometimes” and “often”. Risky behaviors were less frequently reported, as the average frequency across eight risky behaviors was 0.91 (SD = 0.7), or “never” to “rarely”. When all behaviors were included and coded so higher values indicate more favorable behavior, average frequency was 3.34 (SD = 0.5), reflecting high levels of protective behaviors and low levels of risky behaviors overall. Adjusting for socio-demographic covariates, probable PTSD (versus no/low PTSD) as well as greater PTSD symptom severity were associated with significantly greater average frequency of protective behaviors (Table 2; Figure 1). Associations were attenuated though higher PTSD symptom severity remained significantly associated with greater frequency of protective behaviors when adjusting for COVID-19 exposure-related experiences and perceived COVID-19 likelihood and severity (see Supplemental Table 2 for covariate effects). Interestingly, probable PTSD and greater PTSD severity were also associated with significantly greater average frequency of risky behaviors. Additionally, positive associations with risky behaviors were more robust to adjustment for COVID-19 experiences and likelihood and severity of COVID-19 compared with models with protective behaviors. Probable PTSD was not associated with overall mean frequency of behaviors due to the higher protective and increased reverse-scored risky behaviors cancelling each other out. Average protective and average risky behaviors were weakly but significantly negatively correlated in those without probable PTSD (r = −0.17, p < .001), but not in those with probable PTSD (r = −0.07, p = 0.28), highlighting greater inconsistency in behavior patterns within the group with probable PTSD.
Table 2.
Linear Regressions with PTSD Symptoms and Frequency of Engaging in COVID-19 Protective and Risky Behaviors in the Past 30 Days (N = 845)
| Independent Variable: Probable PTSD | Independent Variable: PTSD Severity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||
| Dependent Variable | M | SD | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI |
| Average Behavior Engagement: frequency of engagement from never=0 to always=4 | ||||||||||
| Protective Behaviors | 2.73 | 0.7 | 0.13 * | 0.04, 0.22 | 0.09 | −0.01, 0.18 | 0.07 ** | 0.03, 0.12 | 0.06 * | 0.01, 0.10 |
| Risky Behaviors | 0.91 | 0.7 | 0.14 * | 0.04, 0.23 | 0.15 ** | 0.05, 0.24 | 0.06 * | 0.02, 0.11 | 0.07 * | 0.03, 0.12 |
| All Behaviorsa | 3.34 | 0.5 | 0.00 | −0.07, 0.07 | −0.03 | −0.10, 0.04 | 0.01 | −0.02, 0.04 | 0.00 | −0.04, 0.03 |
| Protective Behaviors | ||||||||||
| Washed hands more frequently | 3.38 | 0.9 | 0.11 | −0.02, 0.23 | 0.08 | −0.05, 0.21 | 0.03 | −0.03, 0.09 | 0.02 | −0.04, 0.09 |
| Used hand sanitizer | 3.28 | 0.9 | 0.04 | −0.10, 0.18 | 0.01 | −0.13, 0.15 | 0.02 | −0.05, 0.09 | 0.00 | −0.07, 0.07 |
| Wore a mask/face covering in public | 3.77 | 0.6 | 0.00 | −0.08, 0.09 | −0.01 | −0.09, 0.08 | 0.01 | −0.03, 0.05 | 0.01 | −0.03, 0.05 |
| Maintained 6-foot distance | 3.18 | 0.9 | 0.11 | −0.02, 0.24 | 0.12 | −0.01, 0.25 | 0.05 | −0.01, 0.12 | 0.06 | −0.01, 0.12 |
| Isolated oneself | 2.66 | 1.2 | 0.18+ | 0.01, 0.35 | 0.09 | −0.08, 0.26 | 0.10 * | 0.02, 0.18 | 0.05 | −0.03, 0.13 |
| Stayed updated on COVID-19 news | 2.96 | 1.0 | 0.14 | −0.01, 0.28 | 0.09 | −0.06, 0.24 | 0.09 * | 0.02, 0.15 | 0.06 | −0.01, 0.13 |
| Sanitized packages | 1.63 | 1.5 | 0.21+ | 0.00, 0.42 | 0.17 | −0.04, 0.39 | 0.12 * | 0.02, 0.22 | 0.11 | 0.01, 0.21 |
| Stocked up on food or supplies | 2.29 | 1.2 | 0.18+ | 0.02, 0.34 | 0.09 | −0.08, 0.25 | 0.11 * | 0.04, 0.19 | 0.07 | −0.01, 0.15 |
| Changed clothes after being outside | 1.99 | 1.4 | 0.25+ | 0.05, 0.46 | 0.19 | −0.02, 0.40 | 0.16 ** | 0.07, 0.26 | 0.14 * | 0.04, 0.24 |
| Took immune supplements | 2.16 | 1.5 | 0.08 | −0.14, 0.30 | 0.03 | −0.19, 0.25 | 0.05 | −0.06, 0.15 | 0.03 | −0.08, 0.14 |
| Risky Behaviors | ||||||||||
| Went to the grocery store | 2.28 | 1.1 | −0.05 | −0.21, 0.11 | 0.01 | −0.16, 0.18 | −0.02 | −0.10, 0.06 | 0.01 | −0.06, 0.09 |
| Took public transportation | 0.47 | 1.0 | 0.21 * | 0.06, 0.35 | 0.21 * | 0.06, 0.35 | 0.11 ** | 0.04, 0.18 | 0.11 * | 0.04, 0.18 |
| Took a flight for vacation | 0.32 | 0.8 | 0.18 * | 0.06, 0.30 | 0.19 * | 0.06, 0.31 | 0.09 ** | 0.04, 0.15 | 0.09 * | 0.04, 0.15 |
| Socialized outdoors | 1.37 | 1.0 | 0.13 | −0.02, 0.28 | 0.14 | −0.01, 0.29 | 0.05 | −0.02, 0.12 | 0.06 | −0.02, 0.13 |
| Socialized indoors | 1.13 | 1.1 | 0.17+ | 0.02, 0.33 | 0.17 | 0.01, 0.32 | 0.08+ | 0.01, 0.15 | 0.09 * | 0.02, 0.16 |
| Attending an event with a large crowd | 0.32 | 0.8 | 0.20 * | 0.08, 0.31 | 0.20 ** | 0.09, 0.32 | 0.09 ** | 0.03, 0.14 | 0.09 * | 0.03, 0.14 |
| Went to outdoor restaurants or bars | 0.83 | 1.0 | 0.12 | −0.03, 0.26 | 0.14 | −0.01, 0.28 | 0.06 | −0.01, 0.13 | 0.07 | 0.00, 0.14 |
| Went to indoor restaurants or bars | 0.59 | 0.9 | 0.13 | −0.01, 0.26 | 0.12 | −0.02, 0.26 | 0.06 | −0.01, 0.12 | 0.06 | −0.01, 0.12 |
Note. Model 1 adjusted for age, gender, race/ethnicity, education, employment, income, marital status, living situation, residential area type, state region; Model 2 adjusted for Model 1 plus COVID-19 test, quarantine, COVID-19 diagnosis, vulnerable conditions, body weight, household COVID-19 diagnosis, knowing others with COVID-19, COVID-19-related employment, and perceived likelihood of infection and severity if infected.
Probable PTSD is PCL-5 severity scores ≥ 33, reference is no/low PTSD. PTSD symptom severity scores are standardized (M = 0, SD = 1).
All behaviors is mean frequency of protective behaviors (never = 0 to always = 4) and inversed risky behaviors (never = 4 to always = 0); higher values indicate more favorable (more protective/fewer risky) behaviors
False Discovery Rate (FDR)-corrected p-values: ** p < .01, *p < .05, +p < .10
Figure 1. Effect Estimates from Linear Regressions with Probable PTSD and Frequency of Engaging in COVID-19 Protective and Risky Behaviors in the Past 30 Days (N = 845).
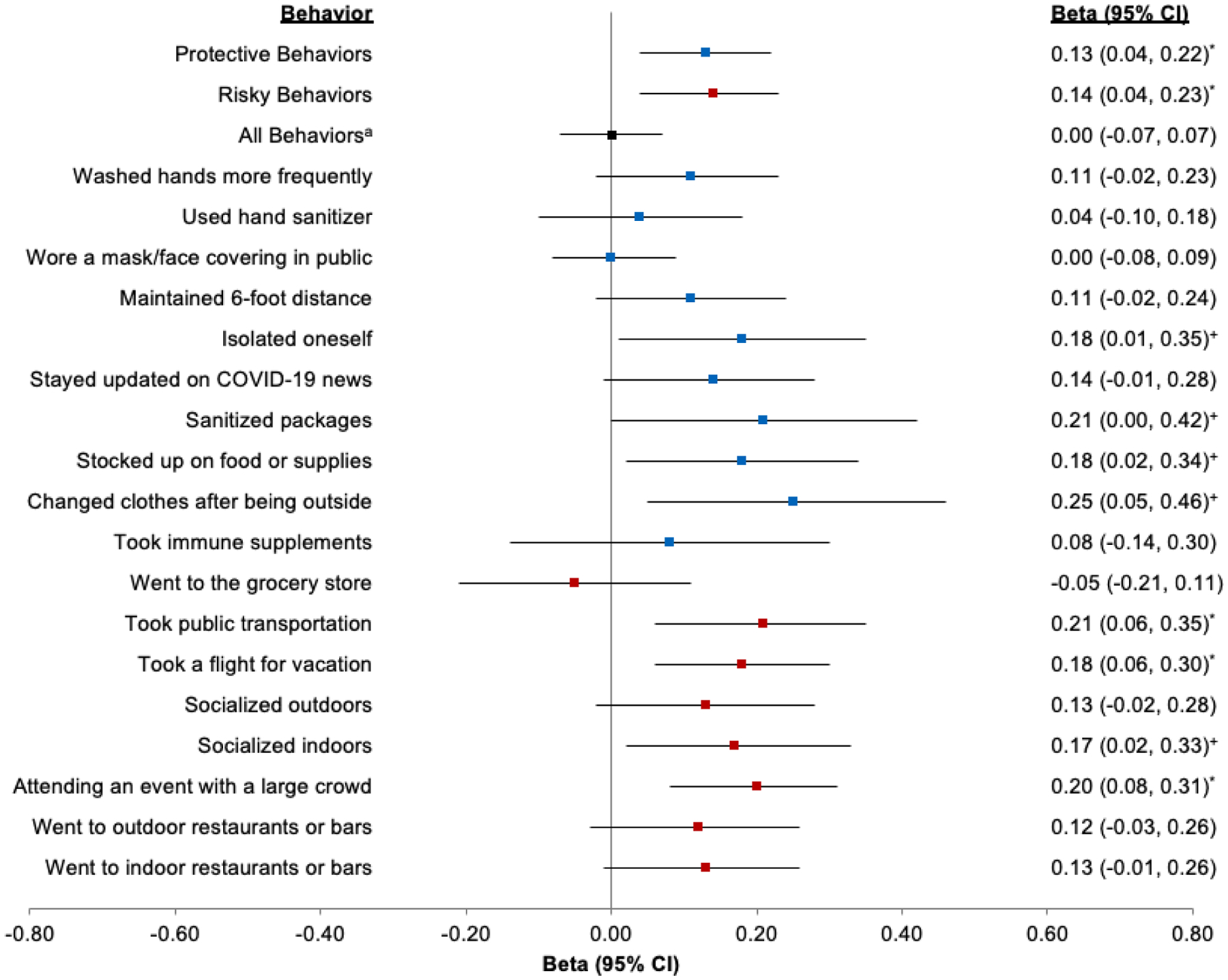
Note. Models adjusted for age, gender, race/ethnicity, education, employment, income, marital status, living situation, residential area type, state region. Probable PTSD is PCL-5 severity scores ≥ 33 (reference PCL-5 severity scores < 33).
a All behaviors is mean frequency of protective behaviors (never = 0 to always = 4) and inversed risky behaviors (never = 4 to always = 0); higher values indicate more favorable (more protective/fewer risky) behaviors
* False Discovery Rate (FDR)-corrected p-values: *p < .05, +p < .10
Individual Protective and Risky Behaviors
Most of the sample reported always engaging in individual recommended protective behaviors such as washing hands (56.9%), sanitizing hands (52.8%), wearing a mask (82.2%), and maintaining six-foot distance from others (43.0%). Other protective behaviors were less commonly reported as always, including sanitizing delivered packages (17.6%), stocking up on supplies (17.2%), and changing clothes after being outside (20.9%). There was also variability in risky behaviors. Most individuals never took public transportation (77.0%), took a flight for vacation (83.3%), attended a large event (81.8%), or went to indoor restaurants (64.0%). Going to the grocery store (6% never), socializing outdoors (23.0% never), and socializing indoors (32.2% never) were more frequently reported. Correlations between engagement in behaviors varied, from no correlation (e.g., staying up to date on COVID-19 news and using public transportation) to r = 0.68 (i.e., going to indoor and outdoor restaurants or bars) (Supplemental Figure 1). Generally, protective behaviors were positively correlated with each other and risky behaviors were positively correlated with each other. Although protective behaviors were mostly negatively correlated with risky behaviors, the relationship was not entirely monotonic (e.g., positive correlations between sanitizing packages and attending a large event, r = 0.13). In exploratory secondary analyses with specific behaviors, probable PTSD was associated with greater frequency of taking public transportation, taking a flight for vacation, and attending an event with a large crowd (and marginally associated with greater frequency of socializing indoors, as well as with isolating oneself, sanitizing packages, stocking food/supplies, and changing clothes after being outside; Table 2; Figure 1). Similar to primary models, adjusting for COVID-19 experiences and vulnerabilities attenuated associations between probable PTSD and individual protective behaviors, but did not impact associations between probable PTSD and individual risky behaviors.
PTSD Symptoms and Perceptions of Behaviors
Individuals with probable PTSD (versus no/low PTSD) reported taking a more cautious approach to protecting themselves against COVID-19 (β = 0.19, 95% CI [0.03, 0.30], p = 0.02), and generally acting more cautiously than others in their community (β = 0.22, 95% CI [0.07, 0.37], p = 0.007), adjusting for socio-demographic covariates.
PTSD Symptom Clusters and Protective and Risky Behaviors
Intrusions, and arousal and reactivity, clusters followed similar patterns to the full PTSD scale (Table 3). The intrusions and arousal and reactivity subscales were each associated with higher levels of protective and higher levels of risky behaviors. In contrast, higher levels of trauma-related avoidance were associated only with more protective behaviors, while higher levels of negative cognitions and mood were only marginally associated with more risky behaviors. Consistent with primary models, adjusting for COVID-19 experiences and vulnerabilities attenuated associations with protective behaviors, but not risky behaviors. Each PTSD symptom cluster was also associated with taking a more cautious approach to protection against COVID-19 and acting more cautiously than their community, adjusted for socio-demographic covariates (Supplemental Table 3).
Table 3.
Linear Regressions with PTSD Symptom Clusters and Frequency of Engaging in Protective and Risky Behaviors for COVID-19 in the Past 30 Days (N = 845)
| Independent Variable: Intrusions | Independent Variable: Avoidance | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||
| Dependent Variable | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI |
| Protective Behaviors | 0.09 *** | 0.04, 0.13 | 0.07 ** | 0.03, 0.12 | 0.08 ** | 0.03, 0.12 | 0.07 ** | 0.02, 0.11 |
| Risky Behaviors | 0.08 *** | 0.04, 0.12 | 0.08 ** | 0.03, 0.12 | 0.03 | −0.01, 0.08 | 0.03 | −0.01, 0.08 |
| All Behaviorsa | 0.01 | −0.03, 0.04 | 0.00 | −0.03, 0.03 | 0.03 | −0.01, 0.06 | 0.02 | −0.01, 0.05 |
| Independent Variable: Negative Cognitions and Mood | Independent Variable: Arousal and Reactivity | |||||||
| Model 1 | Model 2 | Model 1 | Model 2 | |||||
| Dependent Variable | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI |
| Protective Behaviors | 0.04+ | 0.00, 0.09 | 0.02 | −0.02, 0.07 | 0.08 ** | 0.03, 0.12 | 0.05 * | 0.01, 0.10 |
| Risky Behaviors | 0.05+ | 0.00, 0.09 | 0.05+ | 0.01, 0.10 | 0.07 ** | 0.02, 0.11 | 0.08 ** | 0.04, 0.13 |
| All Behaviorsa | 0.00 | −0.03, 0.04 | −0.01 | −0.05, 0.02 | 0.01 | −0.02, 0.04 | −0.01 | −0.04, 0.02 |
Note. Model 1 adjusted for age, gender, race/ethnicity, education, employment, income, marital status, living situation, residential area type, state region; Model 2 adjusted for Model 1 plus COVID-19 test, quarantine, COVID-19 diagnosis, vulnerable conditions, body weight, household COVID-19 diagnosis, knowing others with COVID-19, COVID-19-related employment, and perceived likelihood of infection and severity if infected.
PTSD symptom cluster subscales are standardized (mean=0, SD=1).
All behaviors is mean frequency of protective behaviors (never=0 to always=4) and inversed risky behaviors (never=4 to always=0); higher values indicate more favorable (more protective/fewer risky) behaviors
False Discovery Rate (FDR)-corrected p-values: ***p < .001, ** p < .01, *p < .05, +p < .10
Sensitivity Analyses
Primary analyses were rerun in 25 multiply imputed datasets that imputed missing values among the eligible sample (N = 896) and pooled parameter estimates across datasets. Imputed analyses resulted in similar associations between PTSD symptoms and protective and risky behaviors, with slightly stronger associations for risky behaviors (Supplemental Table 4). Among the sample excluding individuals with short survey durations (n = 80) or locations ostensibly outside the US based on IP addresses (n = 22), our patterns of results generally remained the same, though estimates with risky behaviors were attenuated slightly (Supplemental Table 5). Results for models using probable PTSD defined by the severity cutoff were largely similar to models using a more conservative definition of probable PTSD, which also required DSM-5 diagnostic criteria (Supplemental Table 6). Depression severity was associated with more risky behaviors in fully adjusted models, but was unassociated with protective behaviors (Supplemental Table 7). Associations between anxiety severity and behaviors were similar to those observed for probable PTSD with smaller effect sizes (Supplemental Table 7).
Discussion
In a large trauma-enriched sample of US adults, probable PTSD and higher PTSD symptom severity were associated with greater engagement in protective behaviors against, but also in more risky behaviors for, COVID-19. Importantly, our data indicate that PTSD symptoms are associated with greater objective exposure to COVID-19 (e.g., quarantines, infections in self and others), and higher subjective threat of COVID-19, as indexed by perceived likelihood and predicted severity of infection. However, associations between PTSD symptoms and COVID-19 protective and risky behaviors remained significant even when accounting for COVID-19 exposures, vulnerability factors for poor COVID-19 outcomes, and perceived likelihood and severity of infection. Interestingly, individuals reporting more PTSD symptoms reported more risky behaviors despite a pattern of increased actual and perceived exposure to COVID-19. Additionally, we found that higher PTSD symptoms were associated with the perception of a more cautious approach to COVID-19 overall, indicating a potential discrepancy between perceived approach and actual behavior patterns.
As PTSD is highly heterogeneous (Galatzer-Levy & Bryant, 2013), it is critical that we understand associations of specific symptom profiles with COVID-19 behavior patterns. For example, heightened threat sensitivity in PTSD (Ehlers & Clark, 2000; Lanius et al., 2017; Olatunji et al., 2013) may promote protective behaviors to mitigate feelings of threat. Heightened sensitivity to threat may cause individuals to take more precautionary (e.g., sanitizing packages) or avoidant (e.g., isolating oneself) behaviors, consistent with the concept of safety behaviors – immediate behaviors taken to downregulate unpleasant internal experiences in a specific context – which are believed to be an etiological mechanism in anxiety (Kirk et al., 2019). Increased social isolation seen in PTSD (King et al., 2006) may result in more favorable behaviors in the context of COVID-19, such as isolating and maintaining physical distance from others. We found that intrusions, reactivity, and avoidance subscales were each associated more protective behaviors, suggesting that experiences of unwanted memories, hypervigilance to stimuli, as well as attempts to avoid stimuli may promote engagement with behaviors to protect oneself against COVID-19.
Aspects of PTSD may increase risky behaviors due to inaccurate threat perception, avoidance of thoughts about risk, emotion dysregulation, or deficits in motivational systems (Ben-Zur & Zeidner, 2009). Both the negative cognitions and moods subscale of PTSD and depressive symptoms separately were found to be associated with more risky behaviors in our study; therefore, negative cognitive or emotional processes, or other negative psychological factors related to the pandemic itself such as apathy or despair, may be driving risky behaviors. It is possible that engagement in some risky behaviors represents an attempt to regulate negative emotions through social support (e.g., socializing behaviors). PTSD is also often comorbid with other psychiatric conditions such as substance use disorders, which could contribute to increases in risky behaviors. While adjusting for crude measures of smoking, alcohol, and cannabis use did not alter our pattern of results for protective or risky behaviors, future studies should specifically examine the contributing role of illicit substances. Further, we found that some aspects of PTSD, namely intrusions and reactivity, as well as anxiety symptoms were associated with higher levels of both risky and protective behaviors. Overall, our findings highlight the need to consider protective and risky behaviors and their underlying determinants separately, embedded within a broader framework of the various cognitive, emotional, habitual, and environmental factors known to influence motivation and behavior (e.g., PRIME Theory of Motivation) (West 2007).
Our data add to an emerging literature on COVID-19 protective and risky behaviors. While most prior studies of COVID-19 behaviors have focused on a few specific, recommended preventive behaviors separately (de Bruin & Bennett, 2020; Lee & You, 2020) or averaged across several protective behaviors (Harper et al., 2020; Kim & Cho, 2020), we assessed a wide range of both protective and risky behaviors. Two prior studies have linked higher trauma-related distress, as assessed with the Impact of Events Scale-Revised (IES-R), with reduced protective hygiene-specific COVID-19-related behaviors, which is inconsistent with our findings (Tan et al., 2020; Wang et al., 2020). However, both studies recruited from the general population in China, did not use a validated measure of PTSD symptoms, and only assessed six protective and no risky behaviors, which may have contributed to the apparently inconsistent findings. As such, future studies should expand to community samples, use validated measures of PTSD symptoms, more comprehensive assessments of protective and risky behaviors, and consider local and cultural factors. A better understanding of COVID-19 behavior patterns across individuals, groups, and contexts is urgently needed.
Limitations
There are several limitations to the current study. First, the data are observational and cross-sectional, limiting any conclusions about causality. Second, all measures were self-report and subject to potential response biases, including social desirability biases, which may have been mitigated by the online survey format (Kreuter et al., 2008). Third, we employed the self-report PCL-5 instead of the gold-standard CAPS-5 for assessment of PTSD symptoms, which forces reliance on a probable PTSD diagnosis and means that some reported symptoms may have been linked to multiple stressors rather than to the specified “worst trauma”. Moreover, reported PTSD symptoms may have arisen from COVID-19-related trauma exposure or worsened due to early pandemic experiences, which may confound the association between self-reported PTSD symptoms and COVID-19-related behaviors. However, given the low levels of self-reported COVID-19 infection and the fact that we adjusted for COVID-19-related exposures in analytic models, the concern of confounding by COVID-19 trauma is lessened. Fourth, the eligible sample included only 25% of those initially contacted, raising the possibility of non-response bias, and includes mostly women, limiting generalizability to men. Finally, multiple broader structural and environmental factors influence protective and risky behaviors for COVID-19 as well as risk for PTSD, such as socio-economic resources influencing one’s need to take public transportation and local COVID-19 restrictions influencing the options available for risky behaviors. Although we adjusted for socio-demographic factors and US region, we were unable to fully capture the range of structural influences in our study.
Conclusions
In a sample of 845 individuals who covered almost all US states and generally reflected the racial/ethnic distribution of the country (U.S. Census Bureau, 2020), we found that features of PTSD might enhance engagement in protective behaviors against COVID-19, but also make it more challenging to avoid risky behaviors for contracting the disease. Given that the COVID-19 pandemic is associated with increases in traumatic stress exposure and increases in PTSD, these findings might be particularly relevant as the pandemic evolves over time. Indeed, our findings reflect behavior engagement in August-September 2020, when COVID-19 case rates were relatively lower, compared to earlier in the pandemic or the winter 2020 surge, but also prior to the availability of effective vaccines against COVID-19. It is important to consider that some behaviors that are favorable in the context of the pandemic (e.g., isolating oneself), but may otherwise be detrimental for well-being; future research should examine PTSD and patterns of protective and risky behaviors in other contexts as well as ongoing patterns of COVID-related behaviors in PTSD. Although additional research is needed, it will be beneficial for clinicians and their patients with PTSD to consider and discuss both protective and risky behaviors related to COVID-19. Moreover, when designing public health and clinical interventions, it is advisable to consider the potential impact of mental health on both protective and risky health behaviors.
Supplementary Material
Acknowledgments
This work was supported by the UCSF Department of Psychiatry Rapid Award (AOD), a UCSF Faculty Resource Fund Award (AOD), the National Institutes of Mental Health (AOD; K01MH109871), and KN is supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the SFVAHCS, and the Department of Veterans Affairs Sierra-Pacific Mental Illness Research, Education, and Clinical Center. There are no conflicts of interest.
References
- Ahmadian AJ, Lin JE, Neylan TC, Woolley JD, O’Donovan A, & Cohen BE (2020). Social integration and inflammation in individuals with and without posttraumatic stress disorder. Brain, Behavior, and Immunity, 89, 168–174. 10.1016/j.bbi.2020.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, & Swinson RP (1998). Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. 10.1037/1040-3590.10.2.176 [DOI] [Google Scholar]
- Ben-Zur H, & Zeidner M (2009). Threat to life and risk-taking behaviors: A review of empirical findings and explanatory models. Personality and Social Psychology Review, 13(2), 109–128. 10.1177/1088868308330104 [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Brennan RT, Vinck P, VanderWeele TJ, Spencer-Walters D, Jeong J, Akinsulure-Smith AM, & Pham P (2016). Associations between mental health and Ebola-related health behaviors: A regionally representative cross-sectional survey in post-conflict Sierra Leone. PLoS Medicine, 13(8), Article e1002073. 10.1371/journal.pmed.1002073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, Burling TA, & Spain DA (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23(2), 463–477. 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020a). Implementation of mitigation strategies for communities with local COVID-19 transmission. US Department of Health and Human Services, CDC. [Google Scholar]
- Centers for Disease Control and Prevention. (2020b). Coronavirus Disease 2019 (COVID-19) in the U.S US Department of Health and Human Services, CDC. [Google Scholar]
- Choi KW, Batchelder AW, Ehlinger PP, Safren SA, & O’Cleirigh C (2017). Applying network analysis to psychological comorbidity and health behavior: Depression, PTSD, and sexual risk in sexual minority men with trauma histories. Journal of Consulting and Clinical Psychology, 85(12), 1158–1170. 10.1037/ccp0000241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Caldas SV, Dolan M, Lagdon S, & Armour C (2018). PTSD’s factor structure and measurement invariance across subgroups with differing count of trauma types. Psychiatry Research, 264, 76–84. 10.1016/j.psychres.2018.03.065 [DOI] [PubMed] [Google Scholar]
- Curran PG (2016). Methods for the detection of carelessly invalid responses in survey data. Journal of Experimental Social Psychology, 66, 4–19. 10.1016/j.jesp.2015.07.006 [DOI] [Google Scholar]
- de Bruin WB, & Bennett D (2020). Relationships between initial COVID-19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine, 59(2), 157–167. 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/s0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, & Zvolensky MJ (2007). Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review, 27(1), 14–45. 10.1016/j.cpr.2006.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, & Bryant RA (2013). 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8(6), 651–662. 10.1177/1745691613504115 [DOI] [PubMed] [Google Scholar]
- Golden SD, & Earp JAL (2012). Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health Education & Behavior, 39(3), 364–372. 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- Hall KS, Hoerster KD, & Yancy WS Jr (2015). Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiologic Reviews, 37(1), 103–115. 10.1093/epirev/mxu011 [DOI] [PubMed] [Google Scholar]
- Harper CA, Satchell LP, Fido D, & Latzman RD (2020). Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction, 1–14. 10.1007/s11469-020-00281-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Kim Y-J, & Cho J-H (2020). Correlation between preventive health behaviors and psycho-social health based on the leisure activities of South Koreans in the COVID-19 crisis. International Journal of Environmental Research and Public Health, 17(11), Article 4066. 10.3390/ijerph17114066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, & Stone ER (2006). Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology, 36(12), 2980–2992. 10.1111/j.0021-9029.2006.00138.x [DOI] [Google Scholar]
- Kirk A, Meyer JM, Whisman MA, Deacon BJ, & Arch JJ (2019). Safety behaviors, experiential avoidance, and anxiety: A path analysis approach. Journal of Anxiety Disorders, 64, 9–15. 10.1016/j.janxdis.2019.03.002 [DOI] [PubMed] [Google Scholar]
- Kreuter F, Presser S, & Tourangeau R (2008). Social desirability bias in CATI, IVR, and web surveys: The effects of mode and question sensitivity. Public Opinion Quarterly, 72(5), 847–865. 10.1093/poq/nfn063 [DOI] [Google Scholar]
- Kronish IM, Edmondson D, Li Y, & Cohen BE (2012). Post-traumatic stress disorder and medication adherence: Results from the Mind Your Heart study. Journal of Psychiatric Research, 46(12), 1595–1599. 10.1016/j.jpsychires.2012.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius RA, Rabellino D, Boyd JE, Harricharan S, Frewen PA, & McKinnon MC (2017). The innate alarm system in PTSD: Conscious and subconscious processing of threat. Current Opinion in Psychology, 14, 109–115. 10.1016/j.copsyc.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Lee M, & You M (2020). Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19). International Journal of Environmental Research and Public Health, 17(9), Article 2977. 10.3390/ijerph17092977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SY, & Park CL (2018). Trauma exposure, posttraumatic stress, and preventive health behaviours: A systematic review. Health Psychology Review, 12(1), 75–109. 10.1080/17437199.2017.1373030 [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-u [DOI] [PubMed] [Google Scholar]
- Makhanova A, & Shepherd MA (2020). Behavioral immune system linked to responses to the threat of COVID-19. Personality and Individual Differences, 167, Article 110221. 10.1016/j.paid.2020.110221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles AN, Woolley JD, Tripp P, Pesquita A, Vinogradov S, Neylan TC, & O’Donovan A (2020). Randomized controlled trial testing mobile-based attention-bias modification for posttraumatic stress using personalized word stimuli. Clinical Psychological Science, 8(4), 756–772. 10.1177/2167702620902119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Armstrong T, McHugo M, & Zald DH (2013). Heightened attentional capture by threat in veterans with PTSD. Journal of Abnormal Psychology, 122(2), 397–405. 10.1037/a0030440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Safren SA, & Mayer KH (2009). Stressful or traumatic life events, post-traumatic stress disorder (PTSD) symptoms, and HIV sexual risk taking among men who have sex with men. AIDS Care, 21(12), 1481–1489. 10.1080/09540120902893258 [DOI] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(1), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Rubin DB (2004). Multiple imputation for nonresponse in surveys (Vol. 81). John Wiley & Sons. [Google Scholar]
- Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, Zhao X, Zou Y, Hu Y, & Luo X (2020). Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain, Behavior, and Immunity, 87, 84–92. 10.1016/j.bbi.2020.04.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2020). U.S. Census Bureau QuickFacts: United States
- Van Buuren S, Brand JP, Groothuis-Oudshoorn CG, & Rubin DB (2006). Fully conditional specification in multivariate imputation. Journal of Statistical Computation and Simulation, 76(12), 1049–1064. 10.1080/10629360600810434 [DOI] [Google Scholar]
- van den Berk-Clark C, Secrest S, Walls J, Hallberg E, Lustman PJ, Schneider FD, & Scherrer JF (2018). Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: A systematic review and meta-analysis. Health Psychology, 37(5), 407. 10.1037/hea0000593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M (2018). Crowdsourcing trauma: Psychopathology in a trauma-exposed sample recruited via Mechanical Turk. Journal of Traumatic Stress, 31(4), 549–557. 10.1002/jts.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, & Ho C (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale Available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- West R (2007). The PRIME Theory of motivation as a possible foundation for addiction treatment. In Henningfield J, Santora P and Bickel W (Eds) Drug addiction treatment in the 21st century: Science and policy issues, John’s Hopkins University Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


