Abstract
Intraosseous hemangiomas are uncommon slow-growing benign bone tumors. Most of these lesions are located in the spine or skull and long bone location is rare. Here we present the case of a 63-year-old female with a pathological fracture of the left proximal humerus through an intraosseous hemangioma. Imaging features can be highly unspecific when these tumors are found in the long bones. In this case a pathological fracture obscured the diagnosis even further, prompting the need for tissue sampling to exclude an underlying malignancy.
Keywords: Intraosseous Hemangioma, Pathological Fracture, Humerus
Introduction
Intraosseous hemangiomas are slow progressing tumors that account for less than 1% of all bone tumors [1,2]. These benign vascular lesions are located in the spine and skull in 80% of cases and rarely cause any symptoms [[1], [2], [3], [4], [5]–6]. Histologically they are characterized as blood-containing, thin-walled vessels or sinuses that are lined by endothelium [7]. Intraosseous hemangiomas rarely affect the long tubular bones, however, when present they are most often located in the diaphysis or metaphysis and can develop in the medullary cavity, periosteum, or intracortical bone [8].
Intraosseous hemangiomas of the long bones (IHLB) tend to be associated with a difficult diagnosis due to the rarity of these tumors and their inconsistent radiologic appearance [3,9]. On plain radiographs, IHLBs most often appear as osteolytic lesions with coarse, beehive-like trabeculae [9]. On computed tomography (CT), vertebral lesions have a “polka-dot” appearance on axial projections and a corduroy sign on the sagittal projections [9]. Lastly, magnetic resonance imaging (MRI) reveals a hyperintense signal on T2-weighted imaging, intermediate signal intensity on T1-weighted imaging and contrast enhancement [10]. However, these general diagnostic features are not always present, and the lesions can oftentimes appear atypical, making the tumor simulate a more aggressive entity, prompting the oncology orthopedic surgeon to obtain a biopsy for determination of the proper diagnosis [9]. In view of this, we present an unusual case of a pathological fracture of the humerus secondary to an IHLB.
Case report
A 63-year-old female was referred to our orthopedic oncology clinic for further evaluation and management of a left proximal humerus pathological fracture. 2 months prior to the initial consultation the patient felt sudden severe pain in her proximal left humerus as she was receiving a massage. The patient immediately afterwards developed swelling and ecchymosis in the left upper arm. Her pain persisted despite taking narcotic medication prescribed by her primary care physician. A venous duplex exam of the left upper extremity was obtained, and a deep vein thrombosis was ruled out. The patient was then referred for a general orthopedic evaluation.
The orthopedic surgeon ordered additional diagnostic imaging studies to further evaluate the left upper arm. Radiographs of the left shoulder revealed a displaced, angulated and impacted fracture of the anatomic neck of the left proximal humerus with callus bone formation surrounding the fracture line (Fig. 1). An MRI of the left humerus and shoulder with and without Gadolinium contrast media confirmed the presence of a displaced fracture in the left humeral neck. Additionally, bone marrow edema was observed with hypointense T1 and hyperintense T2 signal intensity at the level of the humeral head extending down to the mid humeral shaft. Soft tissue edema was noted surrounding the fracture site; however, soft tissues were otherwise unremarkable (Fig. 2). Due to the bone marrow edema the presence of an underlying lytic lesion was unable to be assessed. Furthermore, a whole-body nuclear medicine bone scan with Tc99 revealed increased uptake at the level of the left humeral head and neck, but the scan was otherwise unremarkable showing no abnormal uptake in the pelvis, spine, or chest wall (Fig. 3). Unable to exclude the presence of an underlying malignancy, the orthopedic surgeon referred the patient to our orthopedic oncology clinic for further evaluation and management.
Fig. 1.
Left humerus anteroposterior (A) and lateral (B) radiographs showing a proximal humerus displaced, impacted and angulated fracture with new bone formation (white arrow).
Fig. 2.
Left humerus MRI with and without Gadolinium contrast demonstrating the fracture of the proximal left humerus with shortening, displacement, and angulation. Associated extensive bone marrow edema (*) is also shown within humeral head extending to the neck and shaft, hypointense in the T1-weighted sequence (A), hyperintense in the short tau inversion recovery sequence (B) and with Gadolinium enhancement in the T1-fat suppressed post-contrast-sequence (C). Surrounding soft tissues edema is also noted (arrowhead). An underlying lytic lesion could not be excluded due to the extensive bone marrow edema.
Fig. 3.
Nuclear medicine Tc 99 bone scan demonstrating intense increased uptake in the left humeral head and proximal shaft. A single focus of abnormal uptake in the mid-shaft of the left humerus is also observed.
During the initial consultation, the patient mentioned the persistence of moderate to severe left upper arm pain despite taking narcotic medication as prescribed. She denied experiencing any fevers, chills, sudden weight loss, or numbness or tingling in the left upper extremity. On physical examination, there was severe tenderness to palpation, swelling, and a reduced range of motion of the left shoulder. The range of motion of her left elbow, wrist, and digits were within normal limits, and she was neurovascularly intact with palpable pulses and brisk capillary refill distally. Unable to confirm the presence of a malignancy through diagnostic imaging, a decision was made to proceed with a core needle biopsy of the left humeral head under imaging guidance. The histology revealed benign reactive fragments of lamellar bone admixed with fibrous tissue. Multiple levels were examined. Keratin AE1/AE3 immunostaining was negative and CD138 positive plasma cells were few and polytypic for kappa and lambda light chains. No evidence of malignancy in the osseous tissue was found suggesting that a non-diagnostic sample was obtained.
Given that the histopathologic analysis was inconclusive the patient required a repeat biopsy to obtain a diagnostic sample. The biopsy was done under fluoroscopic guidance and appropriate samples of tissue were obtained through a lateral bone window. Histopathologic analysis of the bone biopsy revealed reactive new bone formation, periosteum with fibrosis and scattered multinucleated giant cells. The bone marrow component showed increased number of dilated vascular channels with thin walls and flattened endothelium (Fig. 4). These findings were consistent with a diagnosis of bone hemangioma. Again, no evidence of a malignancy or metastatic disease was found. After discussing the diagnosis and reassuring the patient that there was no evidence of malignancy, she was referred to a shoulder specialist for left shoulder reconstruction.
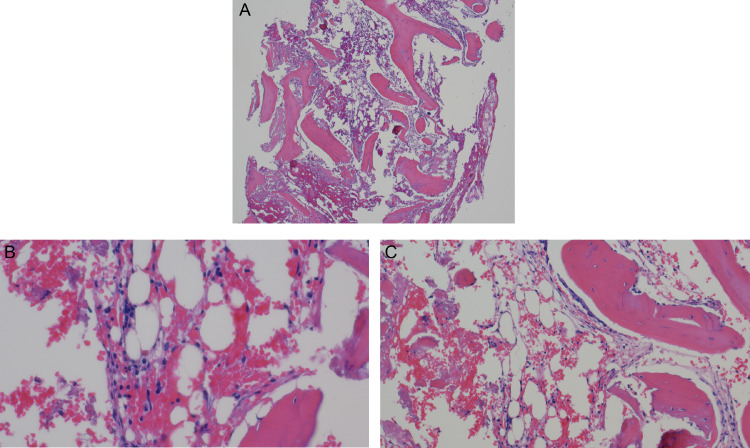
Fig. 4.
Histopathological examination of the left proximal humerus open bone biopsy. Low and high-power views (A: H&E, 10x; B and C: H&E, 20x) of reactive woven bone formation with increased number of small and medium size capillaries and dilated vascular channels with thin walls. No atypia is noted.
Discussion
Intraosseous hemangioma is a rare bone tumor (less than 1%) with even more infrequent presentation within long bones [3]. This slow progressing benign tumor is most commonly found in the vertebra and calvarium [5,11]. Patients are usually in the fourth or fifth decade of life with female predominance [11]. Trauma has been considered to be a possible etiology for this lesion, although this has not been proven [12]. Intraosseous hemangiomas can be difficult to diagnose solely based on imaging findings due to the non-specific imaging features of this tumor. Diagnosis is usually made through histologic findings upon biopsy [13].
Long bone intraosseous hemangiomas on plain radiographs are visualized as irregular and lytic lesions with a honeycomb pattern [9]. These same tumors when in a vertebral location appear differently, with a coarse vertical and trabecular pattern with osseous reinforcement [9]. On CT scan images in the axial plane, the vertical trabeculation depicts a polka-dot appearance with small punctate sclerotic lesions. On sagittal and coronal planes, the corduroy sign is visualized similarly to plain radiographs. Trabecular thickening is unapparent on MRI regardless of the sequence [10]. In lipid-rich intraosseous hemangiomas the T1-sequence appears as hyperintense while T2 sequences demonstrate high intensity due to the high-vascular component of the hemangioma. MRI is the ideal imaging modality to determine complications secondary to mass-effect, neurovascular impingement, and extraosseous extension. Nuclear medicine scans can demonstrate either increased or normal uptake [14].
In the case presented, besides the usual highly unspecific features of intraosseous hemangioma, there was an associated pathologic fracture. The presence of new bone formation, bone marrow edema, surrounding fracture hematoma and displaced bone fragments along the absence of imaging prior to the fracture obscure the diagnosis even more. The intraosseous hemangioma in this case was hypointense on T1 weighted sequences and hyperintense on T2 possibly due to a higher percentage of adipose tissue and the presence of blood-containing vessels characteristic if intraosseous hemangiomas [7,15]. The noted hypo intensity on the T2 weighted sequences is unusual compared to previous reports from the literature, which prompted the need to exclude an underlying malignant cause for the pathological humerus fracture. Nuclear medicine bone scans revealed increased uptake which was expected with an intraosseous hemangioma although this finding is not distinctive as well. All imaging modalities for an intraosseous hemangioma are non-specific and mostly are used to help rule out other types of neoplasms and lesions.
Conclusion
Intraosseous hemangiomas are rarely encountered in the long tubular bones. Although diagnostic imaging methods, such as radiographs, MRI, CT scans, and full body Tc99 bone scans are necessary in the diagnostic process, there must be clinical and pathological correlation with the findings. The patient in this case presented with an associated pathological fracture, resulting in extensive bone marrow edema within the humerus, hematoma, new bone formation and displaced bone fragments which limited and obscured the evaluation for any potential underlying malignancy prompting the need for tissue sampling for diagnostic confirmation.
Footnotes
Acknowledgments: No funding was received for the purpose of this manuscript.
Competing Interests: Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial association (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Patient Consent: The Patient was informed and consented for publication.
References
- 1.Ching BC, Wong JS, Tan MH, Jara-Lazaro AR. The many faces of intraosseous haemangioma: a diagnostic headache. Singapore Med J. 2009;50(5):e195–e198. PMID: 19495509. [PubMed] [Google Scholar]
- 2.Xia Z, Sittampalam K, Howe TS, Lo NN. Successful treatment of solitary intraosseous haemangioma of the femoral neck. Singapore Med J. 2015;56(4):e65–e70. doi: 10.11622/smedj.2014200. PMID: 25917479; PMCID: PMC4415109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaleem Z, Kyriakos M, Totty WG. Solitary skeletal hemangioma of the extremities. Skeletal Radiol. 2000;29(9):502–513. doi: 10.1007/s002560000251. PMID: 11000295. [DOI] [PubMed] [Google Scholar]
- 4.Haro A, Nagashima A. A rare case report of rib hemangioma mimicking a malignant bone tumor or metastatic tumor. Int J Surg Case Rep. 2015;16:141–145. doi: 10.1016/j.ijscr.2015.09.036. Epub 2015 Oct 3. PMID: 26454500; PMCID: PMC4643469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demirkale İ, De Iure F, Terzi S, Gasbarrini A. Aggressive hemangioma of the spine in a pregnant female: a case report and literature review. Eklem Hastalik Cerrahisi. 2016;27(1):46–50. doi: 10.5606/ehc.2016.09. PMID: 26874635. [DOI] [PubMed] [Google Scholar]
- 6.Goff R, Weindling S, Gupta V, Nassar A. Intraosseous Hemangioma of the Middle Turbinate: A Case Report of a Rare Entity and Literature Review. Neuroradiol J. 2015;28(2):148–151. doi: 10.1177/1971400915576653. Epub 2015 Apr 13. PMID: 25923679; PMCID: PMC4757143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdel Razek AA, Castillo M. Imaging appearance of primary bony tumors and pseudo-tumors of the spine. J Neuroradiol. 2010;37(1):37–50. doi: 10.1016/j.neurad.2009.08.006. Epub 2009 Sep 24. PMID: 19781780. [DOI] [PubMed] [Google Scholar]
- 8.Kenan S, Abdelwahab IF, Klein MJ, Lewis MM. Hemangiomas of the long tubular bone. Clin Orthop Relat Res. 1992;(280):256–260. PMID: 1611755. [PubMed] [Google Scholar]
- 9.Cao L, Wen JX, Han SM, Wu HZ, Peng ZG, Yu BH, et al. Imaging features of hemangioma in long tubular bones. BMC Musculoskelet Disord. 2021;22(1):27. doi: 10.1186/s12891-020-03882-2. PMID: 33407312; PMCID: PMC7786894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou Q, Lu L, Yang Z, Su S, Hong G. Hemangioma of long tubular bone: imaging characteristics with emphasis on magnetic resonance imaging. Skeletal Radiol. 2020;49(12):2029–2038. doi: 10.1007/s00256-020-03527-4. Epub 2020 Jun 27. PMID: 32594199. [DOI] [PubMed] [Google Scholar]
- 11.Heckl S, Aschoff A, Kunze S. Cavernomas of the skull: review of the literature 1975-2000. Neurosurg Rev. 2002;25(1-2):56–62. doi: 10.1007/s101430100180. discussion 66-7PMID: 11954766. [DOI] [PubMed] [Google Scholar]
- 12.Powers DB, Fisher E, Erdmann D. Zygomatic intraosseous hemangioma: case report and literature review. Craniomaxillofac Trauma Reconstr. 2017;10(1):1–10. doi: 10.1055/s-0036-1592087. Epub 2016 Nov 4. PMID: 28210401; PMCID: PMC5309129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park BH, Hwang E, Kim CH. Primary intraosseous hemangioma in the frontal bone. Arch Plast Surg. 2013;40(3):283–285. doi: 10.5999/aps.2013.40.3.283. Epub 2013 May 16. PMID: 23730614; PMCID: PMC3665882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. Radiographics. 1995;15(4):893–917. doi: 10.1148/radiographics.15.4.7569134. PMID: 7569134. [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein D, Foremny G, Singer A, Clifford P, Pretell-Mazzini J, Kerr DA, et al. Differential diagnosis of T2 hypointense masses in musculoskeletal MRI. Skeletal Radiol. 2021;50(10):1981–1994. doi: 10.1007/s00256-021-03711-0. Epub 2021 Mar 2. PMID: 33651128. [DOI] [PubMed] [Google Scholar]