Summary
Background
The coronavirus disease 2019 (COVID-19) pandemic is co-occurring with a drug addiction and overdose crisis.
Methods
We fit overdispersed Poisson models, accounting for seasonality and secular trends, to estimate the excess fatal drug overdoses (i.e., deaths greater than expected), using data on all deaths in California from 2016 to 2020.
Findings
Between January 5, 2020 and December 26, 2020, there were 8605 fatal drug overdoses—a 44% increase over the same period one year prior. We estimated 2084 (95% CI: 1925 to 2243) fatal drug overdoses were excess deaths, representing 5·28 (4·88 to 5·68) excess fatal drug overdoses per 100,000 population. Excess fatal drug overdoses were driven by opioids (4·48 [95% CI: 4·18 to 4·77] per 100,000), especially synthetic opioids (2·85 [95% CI: 2·56 to 3·13] per 100,000). The non-Hispanic Black and Other non-Hispanic populations were disproportionately affected with 10·1 (95% CI: 7·6 to 12·5) and 13·26 (95% CI: 11·0 to 15·5) excess fatal drug overdoses per 100,000 population, respectively, compared to 5·99 (95% CI: 5.2 to 6.8) per 100,000 population in the non-Hispanic white population. There was a steep, nonlinear educational gradient with the highest rate among those with only a high school degree. There was a strong spatial patterning with the highest levels of excess mortality in the southernmost region and consistently lower levels at progressively more northern latitudes (7·73 vs 1·96 per 100,000).
Interpretation
Fatal drug overdoses disproportionately increased in 2020 among structurally marginalized populations and showed a strong geographic gradient. Local, tailored public health interventions are urgently needed to reduce growing inequities in overdose deaths.
Funding
US National Institutes of Health and Department of Veterans Affairs.
Keywords: Synthetic opioids, COVID-19, Excess mortality, Substance use, Opioids
Research in context.
Evidence before this study
We searched PubMed for relevant articles in English, published since 2020, on Feb 11, 2022, using the search terms "excess"[Text Word] AND ("drug poisoning"[Text Word] OR "overdose"[Text Word]) AND "covid"[Text Word], which returned four results. Two of the four results were related to excess drug-related mortality during the COVID-19 pandemic. Both noted elevated drug-related mortality in 2020 compared to baseline. One article discussed the impact of shelter-in-place policies, using mobile phones as a proxy of human mobility. The second focused on excess mortality in US adults aged 25 to 44 years and looked at excess mortality broadly with drug overdoses as a subanalysis.
Added value of this study
We systematically analysed excess drug-related mortality in the California, by substance type, region, educational attainment, and race and ethnicity. We estimated excess deaths by using a previously developed statistical framework that accounted for secular trends and seasonality. We found over 2000 more fatal drug overdoses than would have been expected given historical trends. These excess fatal drug overdoses were driven by opioids, especially synthetic opioids such as illicitly-manufactured fentanyl. The most structurally vulnerable populations were the most impacted. Specifically, non-Hispanic Black and Other non-Hispanic (which includes American Indian or Alaska Native) experienced about twice as many excess fatal drug overdoses as the non-Hispanic white population. Similarly, those with only a high school degree experienced three times more excess fatal drug overdoses as those with less than a high school degree or some college but no four-year degree. Lastly, we identified a stark spatial gradient with higher excess fatal drug overdoses in the southernmost region of California and consistent decreases in more northern regions.
Implications of all the available evidence
Our findings highlight the importance of local, targeted public health interventions in stemming the growing substance use and addiction crisis in the US. Structurally vulnerable and marginalized populations were at highest risk. Our findings are consistent with other research that suggests interventions such as expansion of naloxone availability, expanding access to pharmacotherapy and psychosocial treatments for opioid use disorder, harm reduction efforts such as syringe exchange programs are necessary to reduce the crisis broadly. In addition, peer-to-peer services and partnerships with community and faith-based organizations to target local marginalized or high-risk communities are likely necessary to ensure interventions are equitable.
Alt-text: Unlabelled box
Introduction
In 2020, during the coronavirus disease 2019 pandemic, US drug-related deaths soared to over 93,000 deaths — nearly 30% higher than in 2019 — primarily driven by opioids. In 2021, the US topped 100,000 drug-related deaths for the first time.1 There is substantial variation in opioid-related mortality across geographic region and type of opioid, with recent increases in synthetic opioid deaths and cooccurrence of opioids with other illicit substances2 in the total population and recent increases in opioid-related mortality in the non-Hispanic Black and non-Hispanic American Indian or Alaska Native populations.3, 4, 5, 6, 7, 8
Simultaneously, over 900,000 US residents have died from COVID-19,9 with additional unreported COVID-19 deaths and deaths due to other causes,10, 11, 12 shifting the leading causes of death in 2020.13 Recent studies have used excess mortality to quantify the full mortality burden of the COVID-19 pandemic noting substantial variation in excess mortality over time, sociodemographic characteristics such as age, race and ethnicity, and educational attainment, and across geography.14, 15, 16, 17, 18
In this study, we estimate excess deaths due to fatal drug-related overdose in California, from January 5, 2020 to December 26, 2020. California is home to nearly 12% of the US population (39 million residents) and is both sociodemographically diverse and geographically expansive, which allowed us to estimate excess mortality for the total population, stratified by race and ethnicity, educational attainment, and geographic region for all fatal drug-related overdoses combined and by drug type separately.
Methods
Data
We used data provided by the California Department of Public Health – Vital Records on July 24, 2021, which contains death certificates from all deaths that occurred in California between January 1, 2016 and December 26, 2020. In addition to containing information on the underlying cause of death and up to twenty contributory causes of death, which are coded using the International Classification of Disease, Revision 10 (ICD-10), these data also contain information about the decedent's race and ethnicity, age, sex, education, county of residence, and date of death. We categorized decedents’ race and ethnicity as non-Hispanic white, non-Hispanic Black, Hispanic, and Asian using single-race classifications. All other racial and ethnic categories, including mixed and unknown, were classified as other. Separately, for decedents at least 25 years old, we categorized educational attainment as less than high school, high school diploma or equivalent, some college without a 4-year degree, 4-year college degree, or graduate degree. We assigned all deaths to the corresponding California Census Region (Figure S1), hereafter referred to as “region.”
For population denominators, we used the US Census Bureau's public-use microdata to extract education- and race-specific population estimates from 2015 to 2019 (the last year of available microdata). We linearly interpolated the populations within each stratum within years and linearly extrapolated the population within each stratum for the period from 2019 to 2020. Consistent with the CDC estimation of excess deaths, we removed all deaths containing the ICD-10 code for COVID-19 (U07·1) as either an underlying cause or a contributory cause from our analysis.12
This study was approved by the California Health and Human Services Institutional Review Board (Project 2020-109).
Defining deaths of interest
We categorized fatal drug-related overdoses according to recommended guidelines for poisoning deaths.19 Specifically, a drug-related overdose death was defined as any death with an underlying cause of death code of: X40-X44 (Unintentional), X60-X64 (Intentional / Self-harm), X85 (Assault), or Y10-Y14 (Unknown). We defined drug-specific overdose deaths as those that included any of the drug poisoning codes in the underlying cause and at least one drug-related code as a contributory cause: heroin (T40.1), natural or semi-natural opioids such as morphine (T40.2), synthetic and semi-synthetic opioids such as illicitly-manufactured fentanyl (T40.4), any opioid (T40.0 to T40.4 and T40.6), cocaine (T40.5), benzodiazepines (T42.4), and psychostimulants with abuse potential, excluding cocaine (T43.6), which is primarily (but not only) comprised of methamphetamine. In addition, we examined all deaths involving alcohol (T51). Deaths involving more than one substance were included in each substance-specific model.
Analysis
We aggregated death counts to the weekly level. For the counterfactual baseline model of expected deaths, we fit an overdispersed Poisson using data from January 1, 2016 through December 31, 2019, and stratified our analyses by race and ethnicity, educational attainment, and state region for all drug poisonings and for all opioids, specific opioid types, benzodiazepines, cocaine, alcohol, and methamphetamine. This model, described in detail elsewhere,20 assumes deaths are Poisson-distributed with a seasonal trend, long-term trend, and auto-correlated errors. The seasonal trend was modeled as a yearly periodic function using 1 to 4 harmonics. The long-term trend was modeled using natural cubic splines with 0 to 2 internal knots over the whole period. Therefore, there were 12 candidate models for each combination of subpopulation and outcome. For each combination of subpopulation and outcome, we used timeseries cross-validation for model selection to find the optimal candidate model to be used as our counterfactual model (Supplemental Materials Text S1).
We estimated excess deaths as the difference between the observed number of weekly deaths (from January 5, 2020 to December 26, 2020) and the expected number of weekly deaths derived from our baseline model. To account for differences in population size, we present results as excess deaths per 100,000 California residents. We limited our analyses to racial and ethnic, educational, or regional groups and outcomes with an average of more than two deaths per week, which precluded the analysis of Non-Hispanic American Indian or Alaska Natives as a group separate from the “Other Non-Hispanic” category.
We assessed the robustness of our results in several different sensitivity analyses. First, due to potential differences in educational attainment by ethnicity, we re-analysed the education groups stratified by Hispanic ethnicity. Second, we refit our models after aggregating deaths up to the monthly level, which mitigates the potential for autocorrelation at the cost of lower precision. Lastly, we fit an alternative family of baseline models based on autoregressive integrated moving average models called dynamic harmonic regression to assess the sensitivity or our results to model selection.15 Our excess deaths model assumes we are able to properly detect a secular trend in the training data, which is not possible if there is a sudden change in slope in 2019; therefore, in supplemental analyses, we estimated mortality trends by race and ethnicity and educational attainment using joinpoint analyses to detect natural changes in the slope of the crude mortality rate.
Role of the funding source
The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of this manuscript.
Results
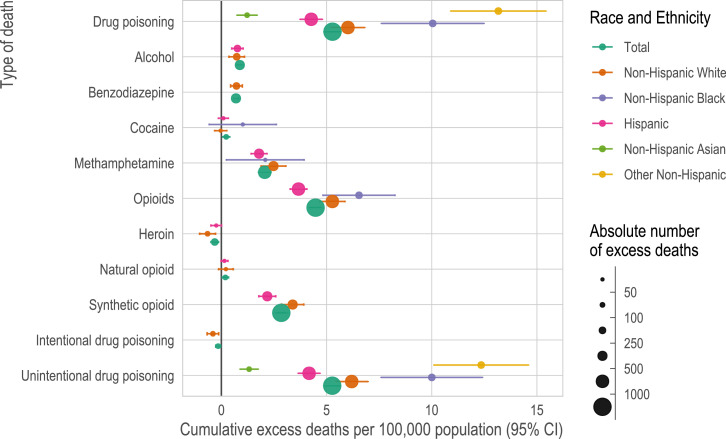
From the 1,367,218 deaths among California residents that occurred between January 1, 2016 through December 26, 2020, we identified 29,568 fatal drug-related overdoses (70% among men with a mean [SD] age of 44·8 [14·9] years and 30% among women with a mean [SD] age of 48·3 [15·3] years). Between January 5, 2020 and December 26, 2020, there were 8605 fatal drug-related overdoses, an increase of 44% compared with the same period one year prior (Table S1). We estimated 2084 (95% CI: 1925 to 2243) of these fatal drug-related overdoses were excess deaths representing 5·28 (4·88 to 5·68) excess fatal drug-related overdoses per 100,000 population (Figure 1). Excess fatal drug-related overdoses appeared to be driven largely by opioids, especially synthetic opioids, and were largely unintentional (Figures 1, S3, Table S1). Reflecting the pattern seen in fatal overdoses, excess overdoses were more frequent among men than women (Figure S4) and primarily driven by individuals aged 18 to 64 (Figure S5). The stratified analyses showed substantial variation by underlying substance, race and ethnicity, educational attainment, and geography (Figure 1, Figure 2, Figure 3). Deaths with missing data were excluded in subgroup analyses for race and ethnicity (N = 240; 0·8%) and education (N = 1908; 6%).
Figure 1.
Cumulative excess fatal drug overdoses per 100,000 population (x-axis) by race and ethnicity (colour) and type of death (y-axis). We show the cumulative excess fatal drug poisonings per 100,000 population (95% CI) for each race and ethnicity and type of death for January 5, 2020 to December 26, 2020. Excess deaths are defined as the difference between observed deaths and the expected number of deaths (and can therefore be negative).
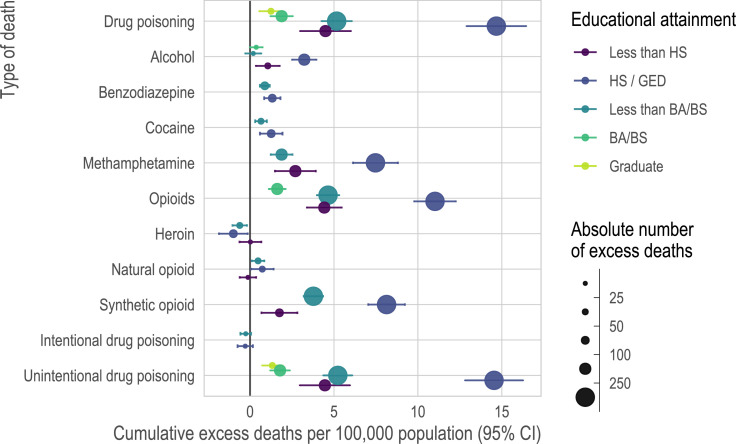
Figure 2.
Cumulative excess fatal drug poisonings per 100,000 population (x-axis) by educational attainment (colour) and type of death (y-axis) among those over 24 years of age. We show the cumulative excess fatal drug overdoses per 100,000 population (95% CI) by educational attainment and type of death for January 5, 2020 to December 26, 2020. Excess deaths are defined as the difference between observed deaths and the expected number of deaths and can therefore be negative.
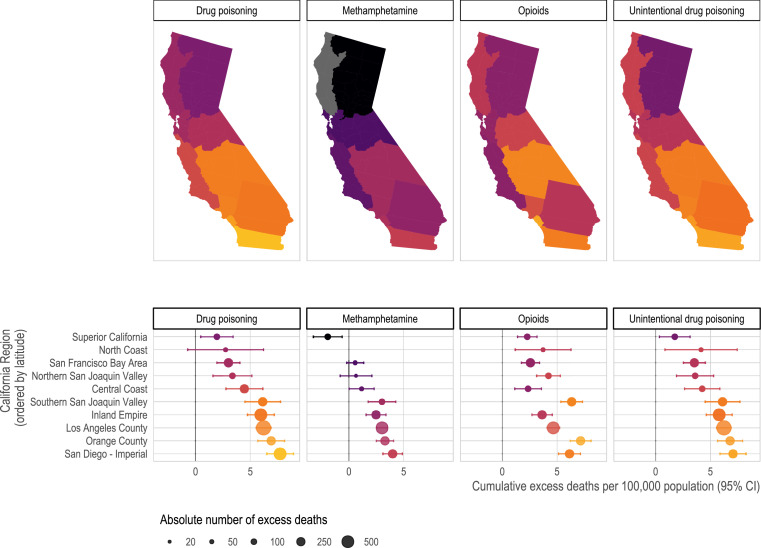
Figure 3.
Cumulative excess fatal drug poisonings per 100,000 population (colour) by California Census Region and type of death (panels). We show the cumulative excess fatal drug poisonings per 100,000 population (95% CI) by California Census Region for January 5, 2020 to December 26, 2020. A spatial gradient by latitude is evident, such that more northerly regions had lower excess fatal drug poisonings. This gradient is not evident for excess deaths from any cause (Figure S9). We present additional outcomes with sufficient sample size and 95% confidence intervals in Figure S8. Excess deaths are defined as the difference between observed deaths and expected deaths and therefore can be negative.
There were 5297 opioid-related overdoses from January 5, 2020 to December 26, 2020, resulting in an estimated 1766 (95% CI: 1651 to 1882) excess fatal overdoses or 4·48 (95% CI: 4·18 to 4·77) excess fatal overdoses per 100,000 population (Figure 1, Table S1). The number of opioid-related overdoses was more than double the excess deaths from methamphetamine (813; 2·06 [95% CI: 1·76 to 2·36] excess fatal overdoses per 100,000), and more than five-fold the excess deaths from alcohol (346; 0·88 [95% CI: 0·70 to 1·05] per 100,000), benzodiazepines (273; 0·69 [95% CI: 0·58 to 0·81] per 100,000), or cocaine (90; 0·23 [95% CI: 0·06 to 0·40] per 100,000) (Figure 1, Table S1). The excess opioid-related overdoses appeared to be driven primarily by synthetic opioids, which increased 242% over the same period one year prior (1593 in 2019 vs 3854 in 2020). This sharp increase resulted in an estimated 1124 (95% CI: 1011 to 1236) excess synthetic opioid overdoses or 2·85 (95% CI: 2·56 to 3·13) per 100,000 population. There were no excess deaths attributable to heroin (-125 [95% CI: -195 to -54]) and only 75 (95% CI: 16 to 134) excess deaths were attributable to natural/semi-synthetic opioids (Figure 1, Table S1).
Although a larger absolute number of excess fatal drug overdoses occurred in the non-Hispanic white population (851 [95% CI: 738 to 964]) compared with the non-Hispanic Black population (219 [95% CI: 166 to 273]), the non-Hispanic Black and Other non-Hispanic populations were disproportionately affected relative to their population size (Table S1 and Figure S3). There were 10·1 (95% CI: 7·61 to 12·49) excess fatal drug overdoses per 100,000 population in the non-Hispanic Black population and 13·3 (95% CI: 11·0 to 15·5) per 100,000 in the Other non-Hispanic population compared with 5·99 (95% CI: 5·19 to 6·78) per 100,000 population in the non-Hispanic white population and 4·28 (95% CI: 3·75 to 4·81) per 100,000 population in the Hispanic population (Figures. 1 and S3, Table S1). Non-Hispanic Asian population had on significant increase in excess mortality per 100,000 (1·23 [95% CI: 0·75 to 1·71). The racial and ethnic patterns overall were consistent across underlying substances, with opioids driving the excess drug overdoses, followed by methamphetamine and cocaine (Figure 1, Table S1). Small sample sizes limited our ability to analyse opioid type by race and ethnicity in the non-Hispanic Black, non-Hispanic Asian, and Other non-Hispanic populations; however, synthetic opioids accounted for two-thirds of opioid-related excess deaths in the non-Hispanic white population and three-fifths of opioid-related excess deaths in the Hispanic population (Table S1).
Nearly 90% of drug-related overdose deaths that occurred in California from January 1, 2016 to December 26, 2020 occurred among individuals aged 25 years or older. Among those 25 years or older, individuals with a high school diploma or equivalent accounted for 43% of excess fatal drug-related overdoses and had both the highest absolute number of excess drug overdoses (809 [95% CI: 711 to 906]) and the highest number of excess fatal drug-related overdoses per 100,000 population at 14·7 (95% CI: 12·9 to 16·4) (Figures. 2, S6, Table S2). Those with some college but no 4-year degree had approximately half the number at 5·14 (95% CI: 4·24 to 6·04; N = 389) excess fatal drug-related overdoses per 100,000 population. The excess fatal drug-related overdose rate was even lower among those with a 4-year degree (1·91 [95% CI: 1·24 to 2·58] per 100,000; 116) and among those with graduate degrees (1·25 [95% CI: 0·55 to 1·95] per 100,000; 45) (Figure 2). Notably, those with less than a high school education experienced fewer excess drug overdoses (4·48 [95% CI: 2·97 to 5·99] per 100,000; 190) than those with a high-school degree. This education gradient appears to be driven by non-Hispanic groups (Figure S7).
When examining excess fatal drug-related overdoses by census region, there was a clear spatial gradient over centroidal latitude, with the highest levels of excess fatal drug overdoses in southern regions and a nearly monotonic decrease in more northerly regions (Figures. 3, S8, Table S3). Specifically, the southernmost region, San Diego – Imperial, had 7·73 (95% CI: 6·51 to 8·94) excess fatal drug-related overdoses per 100,000, which was higher than the second southernmost region, Orange County (6·91 [95% CI: 5·69 to 8·13] per 100,000) and so on until Superior California, the northernmost region, which had 1·96 (95% CI: 0·49 to 3·44) excess fatal drug-related overdoses per 100,000 (Figure 3). This spatial patterning was not observed when examining excess deaths from all causes (Figure S10). The only exceptions to this spatial pattern were the Inland Empire (5·99 [95% CI: 4·77 to 7·22] excess fatal drug-related overdoses per 100,000) and Southern San Joaquin Valley (6·16 [95% CI: 4·53 to 7·79] excess fatal drug-related overdoses per 100,000), which had rates nearly identical to each other (Figure 2). This spatial pattern was evident for unintentional drug overdose and methamphetamine-related overdose but was less consistent for opioid-related overdose (Figure 3). Notably, for the two regions with sufficient sample size, Los Angeles County had high levels of excess fatal synthetic opioid-related overdoses at 2·64 (95% CI: 2·08 to 3·21) per 100,000, while the San Francisco Bay Area did not experience any excess synthetic opioid-related overdoses (0·05 [95% CI: -0·88 to 0·99] per 100,000) (Figure S8).
Unintentional fatal drug-related overdoses accounted for 94% (N = 8,118) of all drug-related overdose deaths in 2020. Nearly all 2084 (95% CI: 1925 to 2243) excess fatal drug-related overdoses were deemed unintentional drug overdoses (2078 [95% CI: 1925 to 2231]), resulting in an estimated 5·27 (95% CI: 4·88 to 5·65) excess fatal unintentional drug-related overdoses per 100,000 population. There were no excess fatal intentional drug-related overdoses (-0·15 [95% CI: -0·27 to -0·04] per 100,000). Importantly, excess drug-related overdoses represented less than 5% of the estimated 44,325 (95% CI: 43,103 to 45,548) excess deaths from all causes (including COVID-19) observed in California over the same period (or 60% of the estimated 14,420 (95% CI: 13,227 to 15,613) excess deaths from all causes excluding COVID-19).
Discussion
Over 2000 more Californians died of drug-related overdose in 2020 than would have been predicted from historical mortality trends. Overall, both US and California death rates increased starkly in 2020. In California, the drug-related mortality rate had the greatest percent increase of any cause of death from 2019 to 2020.21 Long-standing race and ethnic and socioeconomic inequities in California appear to have exacerbated the death toll of the overdose crisis among structurally vulnerable populations just as they have for COVID-19. Consistent with the wider opioid and substance use crisis, our results appear to be driven primarily by males (Figure S4) and those aged 18 to 64 (Figure S5).5
The stark spatial patterning of excess drug overdoses, following a south-to-north pattern that is notably absent evident in all excess mortality from all causes, might be attributable to differences in drug supply,22 which is plausible given that research studies have found an increased presence of heroin laced with fentanyl along the Mexico-California border.23 A better understanding of these geographic patterns may inform better public health resource allocation and more targeted program implementation.
Consistent with other studies, the largest increase in drug-related overdose deaths occurred due to synthetic opioids, which have become more available in the Western US in recent years.3,24 We found no excess deaths that were due to heroin, further evidence of a crisis that has shifted from overdoses due to opioid prescriptions and heroin to overdoses due to synthetic opioids and poly-drug use.25 In California, reporting an overdose death due to multiple drugs is not systematized (i.e., death certificates may not list all the drugs involved, and when involved drugs are listed, the reporting is inconsistent) making public health surveillance difficult and slow to calculate the true mortality burden of evolving drug trends (i.e., fentanyl-laced products).26 More timely and accurate surveillance of overdose outbreaks may be achieved through enhancing cross-sector collaboration, implementing an electronic record system,27 and utilization of certified medical examiners.
Consistent with past trends28 and recent careful analyses of death rates,3 the non-Hispanic Black population experienced the greatest excess mortality burden due to drug-related overdose, further exacerbating the mortality burden due to COVID-19.29 Structurally and socially disadvantaged populations often experience disproportionate worsening of their population health profiles in the setting of environmental and/or social crises.30, 31, 32, 33, 34 Barriers to accessing health care, especially behavioural health care, existed for racial/ethnic minorities prior to — and were exacerbated by — the COVID-19 pandemic.35, 36, 37, 38 This analysis has demonstrated that pre-existing health inequities have worsened, highlighting an urgent need for interventions tailored to cultural-context, specific region, and drug type.7
This study has important limitations. For all excess mortality estimation, one must assume the baseline model accurately represents the unobserved counterfactual, making model selection critical. In sensitivity analyses, we used an alternative level of aggregation (monthly vs weekly) and a different family of model to estimate our counterfactual. Our results were consistent across these sensitivity analyses (Figure S10), but the true underlying counterfactual model cannot be known. Opioid-related mortality in the United States was increasing prior to the COVID-19 pandemic (Figures S11 and S12); thus, how much of the increase in mortality is due to pandemic-related causes (e.g., disruption of care) and how much of it is attributable to a rapidly shifting drug supply is unclear and likely unknowable given existing data. When estimating excess deaths in 2019, in the absence of COVID-19, we found substantially fewer excess deaths than in 2020 for all substances including opioids (Figure S13). All non-opioid deaths were null or nearly null, and consistent with our joinpoint sensitivity analysis, this suggests an increasing rate of opioid-related deaths in 2019. Results of specific substances at the region level should be interpreted with caution due to variation in post-mortem drug testing and reporting on death certificates.39 Descriptive analyses of drug reporting quality show overall high quality, but notable variation across space and over time (Supplemental Table S4). While polysubstance fatal overdose rates are outside the scope of this paper, such deaths are increasingly common and warrant future research to identify potential interventions.2 Patterns of polysubstance fatal overdoses are complex and have changed over time and across racial and ethnic groups and our stratified analyses cannot convey the full complexity of these changing patterns (Supplemental Figure S14). Consistent with previous research, we removed COVID-19 deaths from our estimation of excess mortality; however, it is likely that people who use drugs are at higher risk of contracting and dying from COVID-19 and this competing risk may bias our estimates of excess drug-related mortality.
Although the optimal combination of social and structural interventions needed to address the overdose crisis is unknown, the call to action remains the same: there is an urgent need to reduce deaths due to drug-related overdoses and to simultaneously address the worsening health inequities. Synergistically interacting epidemics — known as syndemics — can magnify the overall disease burden when the two colliding epidemics share environmental and social determinants of health.31 Both the expansion of existing evidence-based interventions and the implementation of novel, tailored interventions are necessary to address factors that are currently known to contribute to the development of opioid use disorder and its morbidity and mortality. The epidemic model of the Stanford-Lancet Commission on the North American Opioid Crisis indicates that expansion of naloxone availability is the policy with the greatest power to reduce overdose deaths in the short term.40 In addition, the Commission report shows smaller but important benefits of expanding access to pharmacotherapy and psychosocial treatments for opioid use disorder and to syringe exchange programs, as well as prescription drug monitoring programs that reduce risky opioid prescribing.41 Other interventions such as an expansion of peer-to-peer services42,43 and partnerships with faith-based or community organizations to improve substance use disorder awareness, prevention and treatment, are designed to reach marginalized or high-risk communities are likely to be particularly effective for communities of colour. Simultaneously the large-scale social and structural forces responsible for the overdose crisis must also be addressed44, 45, 46 and de-stigmatizing messaging and interventions adopted.47, 48, 49 which includes increasing the affordability, accessibility, and equity of health care.37,41,50,51
Contributors
Mathew V. Kiang: conceptualization, data curation, analysis, investigation, methodology, visualization, writing - original draft, writing - review & editing. Rolando J. Acosta: analysis, methodology, software, writing - review & editing. Yea-Hung Chen: conception, data curation, writing - review & editing. Ellicott C. Matthay: writing - review & editing. Alexander C. Tsai: writing - review & editing. Sanjay Basu: writing - review & editing. M. Maria Glymour: conception, writing - review & editing. Kirsten Bibbins-Domingo: conception, data curation, resources, writing - review & editing. Keith Humphreys: conception, writing - original draft, writing - review & editing, supervision. Kristen N. Arthur: writing - original draft, writing - review & editing, supervision.
Mathew V. Kiang, Yea-Hung Chen, and Kristen N. Arthur have accessed and verified the data.
Reproducible code and data sharing statement
All analyses were conducted in R 4·1. Reproducible code is available in an online repository at https://github.com/mkiang/excess_drug_overdoses. Our data use agreement prevents us from sharing raw, decedent-level data; however, to the extent allowed, we provided aggregated data for some racial/ethnic groups and outcomes in the same online repository.
Declaration of interests
The authors have no competing interests.
Acknowledgments
We thank the participants at the NIDA CTN Western Node Speaker Series and University of California, Berkeley Department of Demography's Brown Bag Speaker Series, especially Dr. Ayesha Mahmud, for comments on an early version of this work.
Funding
Mathew V. Kiang and Keith Humphreys receive support from the National Institute on Drug Abuse (R00DA051534 and 2UG1DA015815). In addition, Keith Humphreys receives support from the Veteran Affairs Research Career Scientist Award (04-141). Rolando J. Acosta is supported in part by the National Institute of Environmental Health Sciences (T32ES007142). Ellicott C. Matthay is supported in part by the National Institute for Alcohol Abuse and Alcoholism (K99AA028256). Alexander C. Tsai is supported in part by the Sullivan Family Foundation. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of this manuscript. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or Veterans Affairs.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100237.
Appendix. Supplementary materials
References
- 1.Ahmad FB, Rossen LM, Spencer MR, Warner M, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics 2018.
- 2.Townsend T., Kline D., Rivera-Aguirre A., et al. Racial/ethnic and geographic trends in combined stimulant/opioid overdoses, 2007–2019. Am J Epidemiol. 2022 doi: 10.1093/aje/kwab290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman J., Hansen H., Bluthenthal R.N., Harawa N., Jordan A., Beletsky L. Growing racial/ethnic disparities in overdose mortality before and during the COVID-19 pandemic in California. Prev Med. 2021;153 doi: 10.1016/j.ypmed.2021.106845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman J., Beletsky L., Jordan A. Surging racial disparities in the US. overdose crisis. Am J Psychiat. 2022;179:166–169. doi: 10.1176/appi.ajp.2021.21040381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jalal H., Buchanich J.M., Roberts M.S., Balmert L.C., Zhang K., Burke D.S. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361:eaau1184. doi: 10.1126/science.aau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiang M.V., Basu S., Chen J., Alexander M.J. Assessment of changes in the geographical distribution of opioid-related mortality across the United States by opioid type, 1999–2016. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiang M.V., Tsai A.C., Alexander M.J., Rehkopf D.H., Basu S. Racial/ethnic disparities in opioid-related mortality in the USA, 1999–2019: the extreme case of Washington DC. J Urban Health. 2021:589–595. doi: 10.1007/s11524-021-00573-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander M.J., Kiang M.V., Barbieri M. Trends in black and white opioid mortality in the United States, 1979–2015. Epidemiology. 2018;29:707–715. doi: 10.1097/EDE.0000000000000858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC. CDC COVID data tracker. 2021; published online Sept 15. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed 15 September 2021.
- 10.Kiang M.V., Irizarry R.A., Buckee C.O., Balsari S. Every body counts: measuring mortality from the COVID-19 pandemic. Ann Intern Med. 2020 doi: 10.7326/m20-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC. NVSS - provisional death counts for COVID-19. 2021; published online Sept 15. https://www.cdc.gov/nchs/covid19/mortality-overview.htm. Accessed 15 September 2021.
- 12.CDC. Excess deaths associated with COVID-19. 2021; published online Sept 15. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed 15 September 2021.
- 13.Ahmad F.B., Anderson R.N. The leading causes of death in the US for 2020. JAMA. 2021;325:1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y.H., Glymour M., Riley A., et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y.H., Glymour M.M., Catalano R., et al. Excess mortality in California during the coronavirus disease 2019 pandemic, March to August 2020. JAMA Intern Med. 2021;181 doi: 10.1001/jamainternmed.2020.7578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woolf S.H., Chapman D.A., Sabo R.T., Zimmerman E.B. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. 2021;325 doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faust J.S., Krumholz H.M., Du C., et al. All-cause excess mortality and COVID-19–related mortality among US adults Aged 25–44 years, March-July 2020. JAMA. 2021;325:785–787. doi: 10.1001/jama.2020.24243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinberger D.M., Chen J., Cohen T., et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ISW7 . Proceedings of the Safe States Alliance Injury Surveillance Workgroup. Vol. 7. 2012. Consensus recommendations for national and state poisoning surveillance. [Google Scholar]
- 20.Acosta RJ, Irizarry RA. A flexible statistical framework for estimating excess mortality. medRxiv 2021. 10.1101/2020.06.06.20120857v3. [DOI] [PMC free article] [PubMed]
- 21.CDPH. California department of public health data brief: 2020 increases in deaths in California. 2021; published online Sept 30. https://skylab.cdph.ca.gov/communityBurden/_w_b69bfae4/xMDA/2020_Excess_Mortality.html. Aaccessed 11 October 2021.
- 22.Monnat S.M. The contributions of socioeconomic and opioid supply factors to U.S. drug mortality rates: urban-rural and within-rural differences. J Rural Stud. 2019;68:319–335. [Google Scholar]
- 23.Fleiz C., Arredondo J., Chavez A., et al. Fentanyl is used in Mexico's northern border: current challenges for drug health policies. Addiction. 2020;115:778–781. doi: 10.1111/add.14934. [DOI] [PubMed] [Google Scholar]
- 24.Shover C.L., Falasinnu T.O., Dwyer C.L., et al. Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend. 2020;216 doi: 10.1016/j.drugalcdep.2020.108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatr. 2021;34:344–350. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DEA. 2019 Drug enforcement administration national drug threat assessment. 2019; published online Dec 1. https://www.dea.gov/sites/default/files/2020-02/DIR-007-20%202019%20National% 20Drug%20Threat %20Assessment%20-%20low%20res210.pdf.
- 27.Rosenbaum J.E., Stillo M., Graves N., et al. Timeliness of provisional United States mortality data releases during the COVID-19 pandemic: delays associated with electronic death registration system and weekly mortality. J Public Health Pol. 2021;42:536–549. doi: 10.1057/s41271-021-00309-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Furr-Holden D., Milam A.J., Wang L., Sadler R. African Americans now outpace whites in opioid-involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116:677–683. doi: 10.1111/add.15233. [DOI] [PubMed] [Google Scholar]
- 29.Lawton R., Zheng K., Zheng D., Huang E. A longitudinal study of convergence between Black and White COVID-19 mortality: a county fixed effects approach. Lancet Reg Health Am. 2021;1 doi: 10.1016/j.lana.2021.100011. –100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morello-Frosch R., Zuk M., Jerrett M., Shamasunder B., Kyle A.D. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff. 2017;30:879–887. doi: 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- 31.Tsai A.C., Mendenhall E., Trostle J.A., Kawachi I. Co-occurring epidemics, syndemics, and population health. Lancet. 2017;389:978–982. doi: 10.1016/S0140-6736(17)30403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hansen H., Netherland J. Is the prescription opioid epidemic a white problem? Am J Public Health. 2016;106:2127–2129. doi: 10.2105/AJPH.2016.303483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Netherland J., Hansen H. White opioids: pharmaceutical race and the war on drugs that wasn't. Biosocieties. 2017;12:217–238. doi: 10.1057/biosoc.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gravlee C.C. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am J Hum Biol. 2020;32:e23482. doi: 10.1002/ajhb.23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alsan M., Wanamaker M. Tuskegee and the health of black men. Q J Econ. 2018;133 doi: 10.1093/qje/qjx029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alsan M., Garrick O., Graziani G. Does diversity matter for health? Experimental evidence from Oakland. Am Econ Rev. 2019;109:4071–4111. [Google Scholar]
- 37.Owens G.P., Rogers S.M., Whitesell A.A. Use of mental health services and barriers to care for individuals on probation or parole. J Offender Rehabil. 2011;50:37–47. [Google Scholar]
- 38.Rapp R.C., Xu J., Carr C.A., Lane D.T., Wang J., Carlson R. Treatment barriers identified by substance abusers assessed at a centralized intake unit. J Subst Abuse Treat. 2006;30:227–235. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones C.M., Warner M., Hedegaard H., Compton W. Data quality considerations when using county-level opioid overdose death rates to inform policy and practice. Drug Alcohol Depend. 2019;204 doi: 10.1016/j.drugalcdep.2019.107549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rao I.J., Humphreys K., Brandeau M.L. Effectiveness of policies for addressing the US opioid epidemic: a model-based analysis from the Stanford-lancet commission on the North American opioid crisis. Lancet Reg Health Am. 2021 doi: 10.1016/j.lana.2021.100031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Humphreys K., Shover C.L., Andrews C.M., et al. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford–Lancet Commission. Lancet. 2022;399:555–604. doi: 10.1016/S0140-6736(21)02252-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eddie D., Hoffman L., Vilsaint C., et al. Lived experience in new models of care for substance use disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol. 2019;10:1052. doi: 10.3389/fpsyg.2019.01052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bill Text - SB-803 Mental health services: peer support specialist certification. n.d. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200SB803. Aaccessed 26 October 2021.
- 44.Venkataramani A.S., Bair E.F., O'Brien R.L., Tsai A.C. Association between automotive assembly plant closures and opioid overdose mortality in the United States. JAMA Intern Med. 2020;180:254–262. doi: 10.1001/jamainternmed.2019.5686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dasgupta N., Beletsky L., Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2017;108:e1–e5. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruhm C.J. Drivers of the fatal drug epidemic. J Health Econ. 2019;64:25–42. doi: 10.1016/j.jhealeco.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 47.Paquette C.E., Syvertsen J.L., Pollini R.A. Stigma at every turn: health services experiences among people who inject drugs. Int J Drug Policy. 2018;57:104–110. doi: 10.1016/j.drugpo.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsai A.C., Kiang M.V., Barnett M.L., et al. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PloS Med. 2019;16 doi: 10.1371/journal.pmed.1002969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McCradden M.D., Vasileva D., Orchanian-Cheff A., Buchman D.Z. Ambiguous identities of drugs and people: a scoping review of opioid-related stigma. Int J Drug Policy. 2019;74:205–215. doi: 10.1016/j.drugpo.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 50.Bill Text - SB-110 Substance use disorder services: contingency management services. n.d. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=202120220SB110. Accessed 26 October 2021.
- 51.James K., Jordan A. The opioid crisis in black communities. J Law Med Ethics. 2018;46:404–421. doi: 10.1177/1073110518782949. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.