Extended Data Fig. 3. Risks and 12-month burdens of incident post-acute COVID-19 composite cardiovascular outcomes in participants without any history of cardiovascular outcomes prior to COVID-19 exposure compared to the contemporary control cohort.
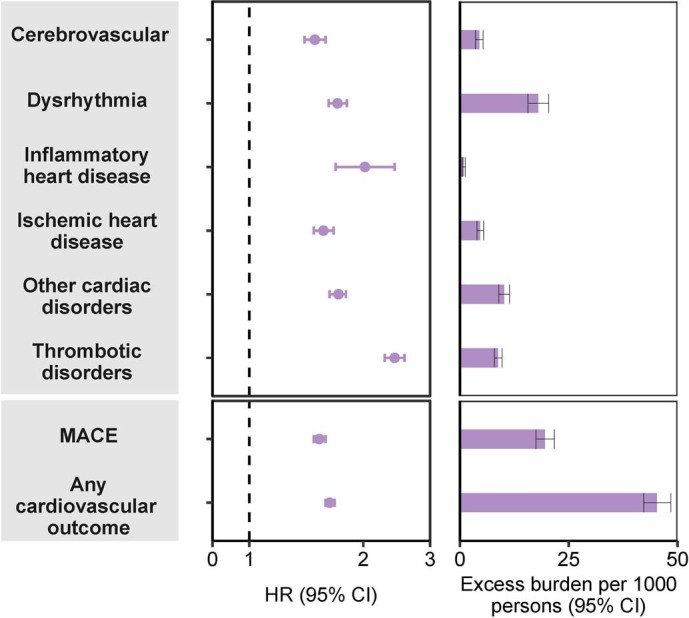
Composite outcomes consisted of cerebrovascular (stroke and TIA), dysrhythmias (atrial fibrillation, sinus tachycardia, sinus bradycardia, ventricular arrhythmias, and atrial flutter), inflammatory heart disease (pericarditis, myocarditis), ischemic heart disease (acute coronary disease, myocardial infarction, ischemic cardiomyopathy, and angina), other cardiac disorders (heart failure, non-ischemic cardiomyopathy, cardiac arrest, and cardiogenic shock), thrombotic disorders (pulmonary embolism, deep vein thrombosis, and superficial vein thrombosis), MACE (all-cause mortality, stroke, and myocardial infarction), and any cardiovascular outcome (incident occurrence of any cardiovascular outcome studied). Outcomes were ascertained 30 days after the COVID-19 positive test until the end of follow-up. COVID-19 cohort without any history of cardiovascular outcomes (N = 126,575) and contemporary control cohort without any history of cardiovascular outcomes (N = 5,010,542). Adjusted hazard ratios and 95% confidence intervals are presented. Length of the bar represents the excess burden per 1000 persons at 12 months and associated 95% confidence intervals are also shown. MACE, major adverse cardiac events; TIA, transient ischemic attack.
