Abstract
Background
The Affordable Care Act (ACA) increased funding for Federally Qualified Health Centers (FQHCs). We defined FQHC service areas based on patient use and examined the characteristics of areas that gained FQHC access post-ACA.
Methods
We defined FQHC service areas using total patient counts by ZIP code from the Uniform Data System (UDS) and compared this approach with existing methods. We then compared the characteristics of ZIP codes included in Medically Underserved Areas/Populations (MUA/Ps) that gained access vs. MUA/P ZIP codes that did not gain access to FQHCs between 2011–15.
Results
FQHC service areas based on UDS data vs. Primary Care Service Areas or counties included a higher percentage of each FQHC’s patients (86% vs. 49% and 71%) and ZIP codes with greater use of FQHCs among low-income residents (29% vs. 22% and 22%), on average. MUA/Ps that gained FQHC access 2011–2015 included more poor, uninsured, publicly insured, and foreign-born residents than underserved areas that did not gain access, but were less likely to be rural (p < .05).
Conclusions
Measures of actual patient use provide a promising method of assessing FQHC service areas and access. Post-ACA funding, the FQHC program expanded access into areas that were more likely to have higher rates of poverty and uninsurance, which could help address disparities in access to care. Rural areas were less likely to gain access to FQHCs, underscoring the persistent challenges of providing care in these areas.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-022-07685-0.
Keywords: Access to care, Underserved populations, Primary care safety net, Rural health, Health disparities
Background
Federally Qualified Health Centers (FQHCs) are a critical component of the US primary care safety net [1]. The Affordable Care Act established the Community Health Center Fund (CHCF) to support the expansion of FQHCs between 2011–2015, allocating $11 billion over five years. The creation of the CHCF, along with the ACA’s Medicaid expansion, led to a dramatic increase in both the funding and growth of FQHCs [2]. FQHC delivery sites are owned by FQHC Grantee organizations (Grantees), which may operate multiple FQHC sites. During the initial CHCF authorization period from 2010 to 2015, the number of Grantees grew from 1,124 to 1,375, the number of FQHC delivery sites increased from 6,949 to 9,754, and the total number of patients served grew 25%, from 19.5 million to 24.3 million [3]. Despite the new funding and growth in sites and patients, there remains no standard by which to assess this growth – in part because of uncertainty on how to best define the area served by an FQHC. In this paper we seek to assess how the post-ACA expansion of FQHC sites expanded geographic access to care and for which populations using data on the locations of FQHC patients.
Expansion of FQHC sites to underserved areas could help reduce geographic health disparities. FQHCs are required to include Medically Underserved Areas (MUAs) or Populations (MUPs), which are designated by the Health Resources and Services Administration (HRSA) or specially designated on the state level. They are also required to provide care to patients regardless of ability to pay, making them a critical source of care for the uninsured. Geographic proximity to FQHCs has been associated with a greater probability of having a usual source of care and having physician visits in the past year [4–6]. Moreover, some studies have demonstrated that low-income patients receiving care from FQHC- vs. non-FQHC providers have better care quality, such as receipt of cancer screening, better access to dental care, better diabetes outcomes, and fewer preventable hospitalizations and emergency room visits [6–14].
The post-ACA expansion of the FQHC program has been shown to improve primary care access in shortage areas; provider availability has improved and more patients have a usual source of care [13, 15]. Findings are limited and mixed, however, on which types of underserved areas were more likely to benefit from recent expansions of the FQHC program [16, 17]. A contributing factor to these varied findings is the challenge of defining an FQHC’s service area.
Data on FQHCs are collected on the Grantee level, but organizations might have up to hundreds of FQHC delivery sites. Depending on the number of FQHCs and the range of locations operated by a Grantee, these service areas vary considerably in size and can encompass non-contiguous geographic areas. In addition, patients’ use of FQHCs could vary as a function of both FQHC capacity and the local availability of non-FQHC providers. Thus, access is likely predicated on patient need and behavior given available options and might not map cleanly to administrative geographic boundaries.
Previous studies have used pre-existing geographic boundaries, such as counties [18] or Primary Care Services Areas (PCSAs) as defined by the Dartmouth Atlas [17], while others have sought to define service areas based on commuting time from FQHC delivery sites [16]. These approaches could be poor reflections of actual access, as reflected in patient use. They may underestimate the care provided by centers, and hinder evaluations that seek to characterize the populations gaining access to FQHCs.
In this analysis we evaluated the performance of an approach adapted from hospital market share definitions to empirically define the service areas of FQHCs using information on the ZIP code locations of patients receiving care at FQHCs. We then applied this approach to examine the characteristics of medically underserved areas that gained access to an FQHC during the initial authorization of the CHCF.
Methods
Data sources and study population
The data for this study are from 2010–2015 Uniform Data System (UDS) for FQHCs. The UDS requires FQHCs to report information at the FQHC Grantee level, including yearly counts of each FQHC Grantee’s patients by residential five-digit ZIP code, Grantee characteristics, and addresses of FQHC delivery sites by year. To limit this analysis to FQHCs accessible to the general population, we focus on the 1,158 Grantees that received Community Health Center Funding located in the 50 United States and Washington, D.C., excluding 109 special population health centers designated as migrant health centers, healthcare for the homeless, or public housing primary care, between 2010–2015. We also excluded 22 Grantees with missing ZIP code data for more than 50% of their patients.
For area-level characteristics, we obtained data from the American Community Survey, the Area Health Resource File, HRSA data on geographic areas designated as Medically Underserved Areas/Populations (MUA/P) or Health Professional Shortage Areas (HPSA), and US Department of Agriculture Rural–Urban Commuting Area (RUCA) Codes.
FQHC service area definitions
We adapted a previously used hospital market share definition method to define FQHC Grantee service areas (“FQHC service areas”) based on UDS patient count data, with the goal of identifying ZIP codes with a high degree of FQHC usage [19]. This method allows for the definition of service areas based on actual patient use while accounting for the complexity of the Grantee-level (multi-site) data that is available for FQHCs. To implement this approach, we included any ZIP code that contributed at least 3% of each FQHC Grantee’s patient population, plus additional ZIP codes (from largest to smallest by patient count) until at least 40% of the Grantee’s patients were included (base approach). In addition, we modified this base approach by also including in each Grantee’s service area the ZIP codes of all the organization’s individual FQHC delivery site locations and all ZIP codes where at least 40% of the ZIP code’s population was served by the Grantee (modified approach). This 40% threshold was used to account for rural ZIP codes that could have small population counts but high local use of FQHCs. In sensitivity analyses, we compared the base approach and the modified approach and examined other thresholds for including ZIP codes with a high proportion of residents served (30% and 50%); findings were similar.
To compare the performance of the UDS-based service areas with two other common approaches to define service areas, we also defined FQHC service areas using the county or Primary Care Service Areas (PCSAs, 2013) that included the ZIP code with the largest proportion of a Grantee’s patients. We linked ZIP codes with counties using the 2015 Department of Housing and Urban Development and United States Postal Service ZIP Code Crosswalk files [20]. PCSAs were developed by the Dartmouth group using data on Medicare ambulatory care visits, validated for younger populations using Medicaid data, and then adjusted to compromise continuous ZIP codes [21]. There were 6,871 PCSAs in 2013.
We compared the proportion of each FQHC Grantee’s patients in 2015 who were included in the service areas defined by each of the three approaches as well as the average number of ZIP codes included in each definition. We then examined FQHC use rates per population for the included ZIP codes in each definition to assess whether there were differences across service area definitions in the area-level FQHC penetration. Because 92% of all FQHC patients have incomes under 200% FPL [3], we calculated the use rate as the number of patients from each ZIP code as reported in the UDS, divided by the Zip Code Tabulation Area (ZCTA) population under 200% FPL, which we obtained from the American Community Survey.
To visually examine differences across service area definitions, we mapped ZIP codes that were included in FQHC service areas in 2010 and newly included ZIP codes between 2011–2015 using QGIS version 3 and 2010 Census TIGER/Line Shapefiles for ZCTAs [22]. To assess how these areas corresponded with the location of FQHC delivery sites, we geocoded delivery site addresses using OpenStreetMap [23] and MMQGIS package using data from the UDS. We illustrate our methods for Louisiana.
Changes in FQHC service areas
We identified MUA/P areas that were classified as FQHC services areas in 2010, those newly classified as FQHC service areas between 2011–2015, and those not included in FQHC service areas in any year 2010–2015. This category of newly classified service area ZIP codes allows us to identify the geographic impact of both new delivery sites and the expansion of existing delivery sites in capacity or geographic reach post-ACA funding. This analysis was limited to ZIP codes that were designated as MUA/Ps by HRSA because FQHCs are required to serve a MUA or MUP. MUAs are defined as geographic areas that have a shortage of primary care services, and MUPs are specific populations within an established geographic area that have a shortage of primary care services (e.g., low-income populations, populations experiencing homelessness) [24]. MUA/Ps are designated by HRSA (and occasionally by states) at the Census tract level, county level, and minor civil divisions. To link these with ZIP code level data in the UDS, we used crosswalk files available from the U.S. Department of Housing and Urban Development (HUD) [20]. All ZIP codes that contained an MUA/P in 2015 or were contained in an MUA/P were included in our analyses.
Analysis
We examined the characteristics of MUA/P ZIP codes that were included in FQHC service areas in 2010 (pre-ACA) vs. 2011–2015 (post-ACA) vs. MUA/P ZIP codes not included anytime 2010–2015. To characterize the sociodemographic characteristics of MUA/P ZIP codes we used five-year estimates from the 2011–2015 American Community Survey to examine sociodemographic characteristics, including age, sex, race, ethnicity, insurance coverage mix (percentage with public insurance, private insurance, or uninsured), urbanicity, and region. To assess urbanicity, we used the four category RUCA classification as of August 2020 to designate ZIP codes as urban, large rural, small rural, and isolated [25].These designations are based on population density and commuting patterns. We used the 2015 Area Health Resource File to identify ZIP codes with Rural Health Clinics. We also used 2015 HRSA data on Health Professional Shortage Areas (HPSAs), to identify ZIP codes in primary care HSPAs, mental health HPSAs, and dental HSPAs. In this definition we used all designated HPSAs, including minor civil divisions, census tracts, counties, and single-point HPSAs, and used 2015 HUD crosswalk files to link these areas with ZIP codes. Medicaid-expansion ZIP codes were defined including ZIP codes in all states that expanded Medicaid prior to 2016 [26].
To compare the characteristics of MUA/P ZIP codes that were newly included in FQHC service areas 2011–2015 vs. not included anytime between 2010–2015, we used multivariate logistic regression.
Results
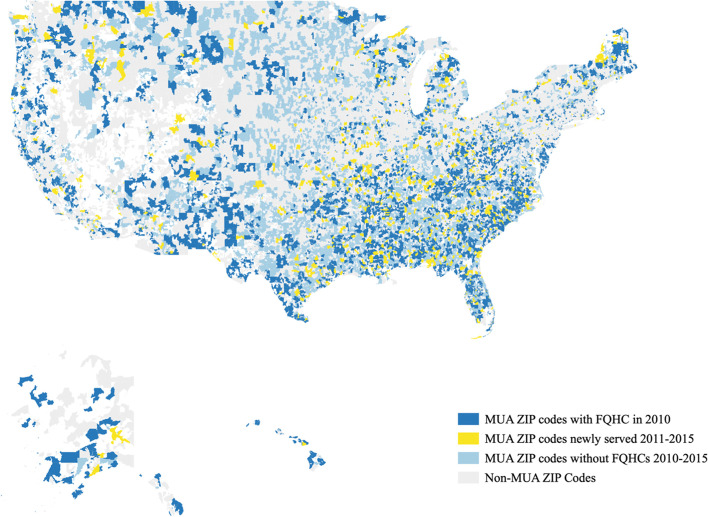
There were 11,369 ZIP codes that were designated as MUA/Ps in 2015, and thus potentially eligible to receive an FQHC. Using the UDS-based definition, 4,600 of these ZIP codes were in an FQHC service area in 2010 (representing 64% of the MUA/P population), another 1,242 ZIP codes (13% of the MUA/P population) were newly included in an FQHC service area between 2011–2015, and 5,527 ZIP codes (23% of the MUA/P population) were not included in an FQHC service area before 2011 nor by 2015. Figure 1 shows a map of these ZIP codes for the United States.
Fig. 1.
ZIP codes with MUA/P designations included in FQHC Service Areas in 2010 vs. 2011–2015 using UDS-based definition
Comparison of service area definitions
The UDS-based approach captured a larger percentage of patients who received care in an FQHC (86% [IQR: 80–94%]), compared with both the PCSA (49% [IQR: 30–68%]) and county-based definitions (71% [IQR: 54–92%], Table 1), while on average including a similar or fewer number of ZIP codes (8.9 [IQR: 6–11] vs. 8.0 [IQR: 3–11] for PCSA and 24.3 [IQR: 8–31] for county). Furthermore, among the ZIP codes included in empirically defined FQHC service areas, there was a higher rate of FQHC use among the residents with incomes < 200% FPL compared with the other two approaches (roughly 29%, vs. 22% and 22%).
Table 1.
Comparison of UDS-based approach for defining FQHC service areas vs. Primary Care Service Area and County (2015)
| UDS-based service areas | Primary Care Service Areasb | Countyc | |
|---|---|---|---|
| Mean [IQR] # ZIP codes per FQHC included in service area | 8.9 [6-11] | 8.0 [3-11] | 24.3 [8-31] |
| Mean [IQR] proportion of FQHC patients included | 86% [80–94] | 49% [30–68] | 71% [54–92] |
| Total # of ZIP codes included in FQHC service areas | 8,713 | 8,568 | 10,105 |
| Total population included in FQHC service areas (millions) | 167.1 | 107.7 | 215.7 |
| % of FQHC service area population with income < 200% FPL that visited an FQHCa | 29% | 22% | 22% |
| % of delivery site ZIP codes included in FQHC service areas | 100% | 53% | 74% |
aEstimated by calculating total number of patients from FQHC’s defined service area divided by population of service area under 200% FPL
bDefined by identifying ZIP codes with largest proportion of patients per FQHC, linking ZIP code to associated PCSA, and then including all ZIP codes linked that PCSA in the service area
cDefined by identifying ZIP codes with largest proportion of patients per FQHC, linking ZIP code to the associated county, and then including all ZIP codes linked that PCSA in the service area
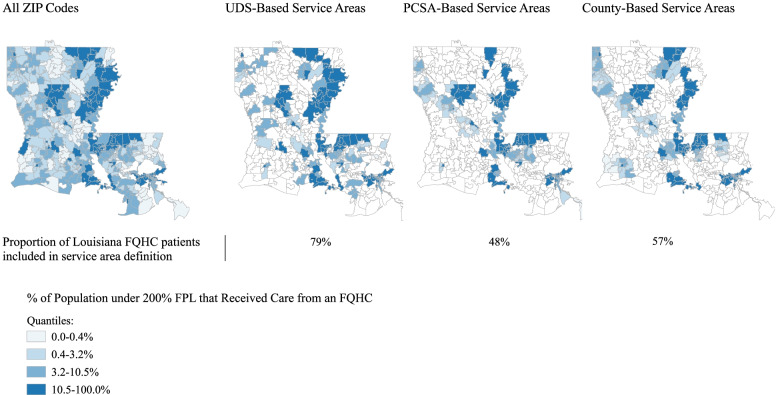
Figure 2 compares these three approaches in Louisiana, a state with one of the largest increases in the total number of FQHC grantees. The UDS-based service areas included 79% of FQHC patients in Louisiana in 2015, compared with 48% and 57% of patients in the PCSA and county definitions, respectively (Supplemental Table 1), as well as a greater proportion of ZIP codes in the highest quartile of FQHC use (roughly 74%, vs. 65% and 72%; see Fig. 2).
Fig. 2.
Density of FQHC Patients in Louisiana, 2015: All ZIP Codes vs. Three Service Area Definitions
Characteristics of areas served in 2010
Among 4,600 ZIP codes included in FQHC service areas in 2010 using the UDS-based definition, the mean population was 20,577 (Table 2). Within these ZIP codes, 63.5% of the population was White, 20.4% Black, 4.3% Asian, and 16.3% of residents were born outside the United States. We found that 44.5% of patients living in these ZIP codes had incomes below the 200% FPL, with 16.6% of residents uninsured, and 37.6% on public insurance. The majority of these 2010 ZIP codes were urban (50.8%), and regionally the highest proportion were in the South (46.1%).
Table 2.
Characteristics of MUA/P ZIP Codes included and not included in FQHC service areas using UDS-based approach
| Characteristics | ZIP Codes with FQHCs in 2010 | Newly Included in Service Areas ZIP Codes 2011–2015 | ZIP Codes without FQHCs 2010- 2015 |
aOR (Newly Included vs. Not Included in Service Areas) |
|---|---|---|---|---|
| Total ZIP codes | 4,600 | 1,242 | 5,527 | - |
| Mean ZIP population (SD) | 20,577 (18,598) | 14,820 (14,508) | 6,471 (8,918) | - |
| Total population (2015, millions) | 94.7 | 18.4 | 35.8 | |
| Population-Level Characteristics: | ||||
| Age: < = 20 years old | 26.8% | 25.8% | 25.2% | 0.99 [0.98–1.00] |
| 20–64 years old | 60.1% | 59.6% | 58.5% | - |
| 65 + years old | 13.1% | 14.6% | 16.3% | 0.98 [0.97–0.99] |
| Race: White | 63.5% | 75.1% | 81.5% | - |
| Black | 20.4% | 13.6% | 9.5% | 1.09 [1.04–1.14] |
| Asian | 4.3% | 3.7% | 2.5% | 0.87 [0.69–1.1] |
| American Indian/ Alaska Native | 0.9% | 0.7% | 1.3% | 0.69 [0.58–0.81] |
| Native Hawaiian/ Pacific Islander | 0.2% | 0.1% | 0.1% | 0.75 [0.21–2.7] |
| Other | 7.6% | 4.0% | 2.5% | 1.00 [0.81–1.23] |
| Two Plus | 3.1% | 2.7% | 2.5% | 1.47 [1.11–1.94] |
| Ethnicity: Hispanic | 25.7% | 15.7% | 10.9% | 0.87 [0.80–0.95] |
| Place of birth: Foreign born | 16.3% | 10.7% | 7.3% | 1.52 [1.28–1.81] |
| HH income: < 200% FPL | 44.5% | 37.9% | 33.3% | 1.32 [1.10–1.57] |
| Insurance type: Private | 53.7% | 61.6% | 65.5% | - |
| Public | 37.6% | 33.1% | 32.6% | 1.14 [1.04–1.26] |
| Uninsured | 16.6% | 14.4% | 12.5% | 1.19 [1.05–1.34] |
| ZIP Code-Level Characteristics: | ||||
| Urbanicity: Urban | 50.8% | 33.2% | 20.6% | - |
| Large rural | 23.2% | 32.0% | 36.4% | 0.53 [0.44–0.64] |
| Small rural | 9.1% | 13.1% | 13.1% | 0.56 [0.44–0.72] |
| Isolated rural | 16.9% | 21.7% | 29.8% | 0.45 [0.36–0.56] |
| Rural Health Clinic | 42.7% | 49.6% | 58.2% | 0.72 [0.62–0.83] |
| HSPA: Primary Care | 74.6% | 69.3% | 65.1% | 1.08 [0.92–1.27] |
| Mental Health | 72.0% | 72.1% | 67.6% | 1.38 [1.15–1.65] |
| Dental Health | 71.5% | 66.3% | 58.5% | 1.37 [1.16–1.61] |
| Medicaid Expansion State | 57.9% | 51.0% | 51.9% | 1.06 [0.89–1.26] |
| Northeast | 14.8% | 9.8% | 11.2% | - |
| South | 46.1% | 51.5% | 45.9% | 1.02 [0.78–1.34] |
| Midwest | 18.4% | 22.6% | 30.7% | 1.12 [0.87–1.46] |
| West | 20.7% | 16.0% | 12.1% | 1.57 [1.17–2.10] |
Analysis performed in STATA v.14.0. Adjusted odds ratios for continuous variables were calculated for a 10-percentage point difference. All characteristics are population-weighted means
Comparing newly served and unserved areas
ZIP codes that were newly included vs. not included in FQHC service areas were more likely to have a larger proportion of Black residents (13.6% vs. 9.5%; OR 1.09 [95% CI: 1.04–1.14] for a 1 percentage point increase), foreign-born residents (10.7% vs. 7.3%, OR 1.52 [1.28–1.81]), residents with incomes below 200% FPL (37.9% vs. 33.3%, OR 1.32 [1.10–1.57]), uninsured (14.4% vs. 12.5%, OR 1.19 [1.05–1.34]), and publicly insured (33.1% vs. 32.6%, OR 1.14 [1.04–1.26])) residents (Table 2). ZIP codes that were newly included vs. not included in FQHC service areas were also more likely to be shortage areas, with 72.1% vs. 67.6% in mental health HPSAs (OR 1.38 [1.15–1.65]), and 66.3% vs. 58.5% in dental health HPSAs (OR 1.37 [1.16–1.61]).
MUA/P ZIP codes that were newly included in FQHC service areas were less likely to be in rural areas (e.g., 21.7% vs. 29.8% in isolated rural areas, OR 0.45 [0.36–0.56]. These areas also had a lower proportion of residents that were age 65 + (14.6% vs 16.3, OR 0.98 [0.97–0.99]) or American Indian/Alaska Native (0.7% vs. 1.3%, OR 0.69 [0.58–0.81]) patients vs. areas not included in FQHC service areas.
Discussion
In this study, we assessed how the ACA changed geographic access to FQHC services by adapting a method used to assess hospital market share to the definition of FQHC service areas based on public patient use data reported by FQHCs to HRSA. This approach captures a greater proportion of FQHC patients and identifies ZIP codes with greater FQHC use, on average, than previously used methods that use pre-existing geographic boundaries or require contiguous geography. Using this approach, we found that the initial expansion of the FQHC program under ACA funding increased access to safety net primary care services for about 18.4 million residents living in medically underserved ZIP codes in 2015.
In contrast to other studies that have examined changes in geographic access to FQHCs, our approach did not measure changes in FQHC service areas solely associated with the location of new delivery sites, which could vary in capacity and service offerings [16, 17]. While providing funds for new delivery sites was a crucial component of CHCF funding, FQHCs could also use the funding to expand service offerings, improve infrastructure, and hire additional staff [2], enabling existing delivery sites to expand capacity and geographic reach. Our measure of FQHC service areas and their change over time could thus better reflect changes in access to and use of FQHCs associated with ACA-related revenue increases than prior measures, as well as changes in local need for care or local supply of non-FQHC care.
Our study adds to the limited evidence on changes in area-level access to FQHCs following the ACA. Similar to one national study, which compared FQHC service areas in 2014 to 2007 based on PCSAs, we found that areas newly included in service areas had a lower proportion of residents below federal poverty standards than pre-ACA FQHC service areas [17]. However, among medically underserved areas that did not previously have access to an FQHC, we found newly served ZIP codes were more likely to have higher rates of poverty, uninsurance, a greater proportion of Black residents, and were more likely to be designated as mental health and dental health professional shortage areas. These findings suggest that the growth of the FQHC program post-ACA expanded access to medically underserved areas with populations that could face greater structural barriers to health care access (e.g., related to discrimination, socioeconomic status, provider supply), and to groups that were disproportionately impacted by the COVID-19 pandemic. FQHCs have faced many financial challenges during the pandemic that led to some temporary closures of delivery sites and staff downsizing, but FQHCs have also served as critical providers of COVID-19 testing, care, and vaccinations for racial/ethnic minority and low-income patients [27, 28].
Underserved rural vs. urban areas, however, were less likely to be included in FQHC service areas post-ACA, which may reflect compounding challenges of staffing, reimbursement, and volume that health care facilities face in rural settings. Rural residents receiving care at FQHCs have previously been found to be more likely to receive certain preventive services, such as Pap smear and pneumococcal vaccinations compared with the general rural population [29]. Greater expansion of FQHCs or similar interventions in rural areas could help address health disparities present in rural communities and potentially address reductions in the availability of emergency and hospital care [30]. These findings support future investigations into barriers in the development of rural FQHCs and the consideration of policy interventions to better target these rural communities.
The Community Health Center Fund has been reauthorized by Congress multiple times at levels of funding similar to that of the ACA [31]. It comprises a growing share of federal Sect. 330 funds for FQHCs, and is currently authorized through September 30, 2023 [32]. In addition, the American Rescue Plan included $7.6 billion in emergency COVID-19 funding for FQHCs. This continued funding has contributed to sustained growth of the FQHC program, which served 29.8 million patients in 2019 [33].
Limitations
This study has several limitations. We defined service areas based on aggregate data at the FQHC level; using these data, we are not able to quantify the regularity or types of services received by individual patients, which could improve measures of service areas and access to care. We also were not able to directly capture a distinction between newly offered services or new delivery sites and services that shifted to serve new geographic areas. In addition, we could not identify patients with visits to multiple FQHCs and we could overestimate use of FQHCs within a given ZIP code; in prior work using claims data, however, we found that use of multiple FQHCs was uncommon [9].
Conclusions
Through data on patient use, the findings of this study suggest that the ACA increased access to safety net primary care to underserved populations that experience significant health disparities – but gaps for rural areas remain.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- ACA
Affordable Care Act
- CHCF
Community Health Center Fund
- FQHC
Federally Qualified Health Center
- HPSA
Health Professional Shortage Area
- HUD
U.S. Department of Housing and Urban Development
- MUA
Medically Underserved Area
- MUP
Medically Underserved Population
- PCSA
Primary Care Service Area
- RUCA
Rural–Urban Commuting Area
- UDS
Uniform Data System
- ZCTA
Zip Code Tabulation Area
Authors’ contributions
VF conceived of the original research question with assistance from JH, JN, PH, and CB in the design of the investigation and analysis. CB completed the analysis and design of all tables and figures with supervision from VF. CB and VF drafted the manuscript with assistance from JH, JN, and PH. All authors discussed the results and contributed to the final manuscript. The author(s) read and approved the final manuscript.
Funding
Paper funded by AHRQ R01HS025378.
Availability of data and materials
FQHC UDS data are available from the corresponding author on reasonable request. American Community Survey data are available through the U.S. Census Bureau, https://www.census.gov/programs-surveys/acs/data.html. Area Health Resource Files and Health Professional Shortage Areas available through the Health Resources and Services Administration Data Warehouse; https://data.hrsa.gov/data/download, Rural–Urban Commuting Codes are available from the U.S. Department of Agriculture Economic Research Service, https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.
Declarations
Ethics approval and consent to participate
This study was approved by the Mass General Brigham Institutional Review Board. All methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
Caroline Behr has no competing interests to disclose.
Peter Hull has no competing interests to disclose.
John Hsu consults or has consulted for the following: Cambridge Health Alliance, Alta Med Health Center, Columbia University, Community Servings, Delta Health Alliance, RWJF, USC.
Joseph Newhouse has no competing interests to disclose.
Vicki Fung has no competing interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care–the growing importance of the community health center. N Engl J Med. 2010;362(22):2047–2050. doi: 10.1056/NEJMp1003729. [DOI] [PubMed] [Google Scholar]
- 2.Kaiser Family Foundation. Community Health Center Financing: the Role of Medicaid and Section 330 Grant Funding Explained. Washington, DC; 2019 March 26. Available from: https://www.kff.org/report-section/community-health-center-financing-the-role-of-medicaid-and-section-330-grant-funding-explained-issue-brief/. Cited March 16th, 2022.
- 3.National Association of Community Health Centers . Community Health Center Chartbook. 2018. [Google Scholar]
- 4.Brown ER, Davidson PL, Yu H, Wyn R, Andersen RM, Becerra L, et al. Effects of community factors on access to ambulatory care for lower-income adults in large urban communities. Inquiry. 2004;41(1):39–56. doi: 10.5034/inquiryjrnl_41.1.39. [DOI] [PubMed] [Google Scholar]
- 5.Gresenz CR, Rogowski J, Escarce JJ. Health care markets, the safety net, and utilization of care among the uninsured. Health Serv Res. 2007;42(1 Pt 1):239–264. doi: 10.1111/j.1475-6773.2006.00602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadley J, Cunningham P. Availability of safety net providers and access to care of uninsured persons. Health Serv Res. 2004;39(5):1527–1546. doi: 10.1111/j.1475-6773.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shin P, Alvarez C, Sharac J. A profile of community health center patients: implications for policy. Washington, DC: The Henry J. Kaiser Family Foundation; 2013. [Google Scholar]
- 8.Evans CS, Smith S, Kobayashi L, Chang DC. The Effect of Community Health Center (CHC) Density on Preventable Hospital Admissions in Medicaid and Uninsured Patients. J Health Care Poor Underserved. 2015;26(3):839–851. doi: 10.1353/hpu.2015.0081. [DOI] [PubMed] [Google Scholar]
- 9.Myong C, Hull P, Price M, Hsu J, Newhouse JP, Fung V. The impact of funding for federally qualified health centers on utilization and emergency department visits in Massachusetts. PLoS One. 2020;15(12):e0243279. doi: 10.1371/journal.pone.0243279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Probst JC, Laditka JN, Laditka SB. Association between community health center and rural health clinic presence and county-level hospitalization rates for ambulatory care sensitive conditions: an analysis across eight US states. BMC Health Serv Res. 2009;9:134. doi: 10.1186/1472-6963-9-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falik M, Needleman J, Herbert R, Wells B, Politzer R, Benedict MB. Comparative effectiveness of health centers as regular source of care: application of sentinel ACSC events as performance measures. J Ambul Care Manage. 2006;29(1):24–35. doi: 10.1097/00004479-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Nocon RS, Lee SM, Sharma R, Ngo-Metzger Q, Mukamel DB, Gao Y, et al. Health Care Use and Spending for Medicaid Enrollees in Federally Qualified Health Centers Versus Other Primary Care Settings. Am J Public Health. 2016;106(11):1981–1989. doi: 10.2105/AJPH.2016.303341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saloner B, Wilk AS, Levin J. Community Health Centers and Access to Care Among Underserved Populations: A Synthesis Review. Med Care Res Rev. 2020;77(1):3–18. doi: 10.1177/1077558719848283. [DOI] [PubMed] [Google Scholar]
- 14.Mehta PP, Santiago-Torres JE, Wisely CE, Hartmann K, Makadia FA, Welker MJ, et al. Primary Care Continuity Improves Diabetic Health Outcomes: From Free Clinics to Federally Qualified Health Centers. J Am Board Fam Med. 2016;29(3):318–324. doi: 10.3122/jabfm.2016.03.150256. [DOI] [PubMed] [Google Scholar]
- 15.Xue Y, Greener E, Kannan V, Smith JA, Brewer C, Spetz J. Federally qualified health centers reduce the primary care provider gap in health professional shortage counties. Nurs Outlook. 2018;66(3):263–272. doi: 10.1016/j.outlook.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Evans L, Charns MP, Cabral HJ, Fabian MP. Change in geographic access to community health centers after Health Center Program expansion. Health Serv Res. 2019;54(4):860–869. doi: 10.1111/1475-6773.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang CH, PWB J, Lurie JD. Geographic Expansion of Federally Qualified Health Centers 2007–2014. J Rural Health. 2019;35(3):385–94. doi: 10.1111/jrh.12330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nath JB, Costigan S, Lin F, Vittinghoff E, Hsia RY. Access to Federally Qualified Health Centers and Emergency Department Use Among Uninsured and Medicaid-insured Adults: California, 2005 to 2013. Acad Emerg Med. 2019;26(2):129–139. doi: 10.1111/acem.13494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zwanziger J, Melnick GA. The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California. J Health Econ. 1988;7(4):301–320. doi: 10.1016/0167-6296(88)90018-5. [DOI] [PubMed] [Google Scholar]
- 20.Office of Policy Development and Research. HUD-USPS ZIP Code Crosswalk. Washington, D.C. 2015. Available from: https://www.huduser.gov/portal/datasets/usps_crosswalk.html. Cited March 16th, 2022
- 21.Goodman DC, Mick SS, Bott D, Stukel T, Chang CH, Marth N, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003;38(1 Pt 1):287–309. doi: 10.1111/1475-6773.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Census Bureau. TIGER/Line Shapefile ZIP Code Tabulation Areas ed2010. Available from: https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html. Cited March 16th, 2022.
- 23.OpenStreetMap Foundation. OpenStreeMap. Cambridge, UK. Available from: https://www.openstreetmap.org/#map=8/9.629/-84.253. Cited March 16th, 2022.
- 24.U.S. Department of Health and Human Services. Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas/Populations (MUA/P) Shortage Designation Types 2019. Available from: https://www.hhs.gov/guidance/document/hpsa-and-muap-shortage-designation-types. Cited March 16th, 2022.
- 25.United States Department of Agriculture Economic Research Service. 2010 Rural-Urban Commuting Area (RUCA) Codes Washington, D.C. 2016. Available from: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Cited March 16th, 2022.
- 26.Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision Washington, DC 2021. Updated July 9 2021. Available from: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D#note-1. Cited March 16th, 2022.
- 27.Corallo BA, S.; Tolbert, J. Are Health Centers Facilitating Equitable Access to COVID-19 Vaccinations? A June 2021 Update: Kaiser Family Foundation; 2021. Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/are-health-centers-facilitating-equitable-access-to-covid-19-vaccinations-a-june-2021-update/. Cited March 16th, 2022.
- 28.Health Resources & Services Administration. Health Center COVID-19 Survey. 2021 Available from: https://bphc.hrsa.gov/emergency-response/coronavirus-health-center-data. Cited March 16th, 2022.
- 29.Regan J, Schempf AH, Yoon J, Politzer RM. The role of federally funded health centers in serving the rural population. J Rural Health. 2003;19(2):117–24. doi: 10.1111/j.1748-0361.2003.tb00552.x. [DOI] [PubMed] [Google Scholar]
- 30.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC; 2016 June. 377p. Available from: https://www.medpac.gov/document/http-www-medpac-gov-docs-default-source-reports-june-2016-report-to-the-congress-medicare-and-the-health-care-delivery-system-pdf/. Cited March 16th, 2022.
- 31.National Association of Community Health Centers. Federal Grant Funding 2021 Available from: https://www.nachc.org/focus-areas/policy-matters/health-center-funding/federal-grant-funding/. Cited March 16th, 2022.
- 32.H.R.133 - Consolidated Appropriations Act, 116th Congress. 2020. Available from: https://www.congress.gov/bill/116th-congress/house-bill/133. Cited March 16th, 2022.
- 33.United States Health Resources and Services Administration. National Health Center Data Washington, DC. 2019. Available from: https://data.hrsa.gov/tools/data-reporting/program-data/national. Cited March 16th, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
FQHC UDS data are available from the corresponding author on reasonable request. American Community Survey data are available through the U.S. Census Bureau, https://www.census.gov/programs-surveys/acs/data.html. Area Health Resource Files and Health Professional Shortage Areas available through the Health Resources and Services Administration Data Warehouse; https://data.hrsa.gov/data/download, Rural–Urban Commuting Codes are available from the U.S. Department of Agriculture Economic Research Service, https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.