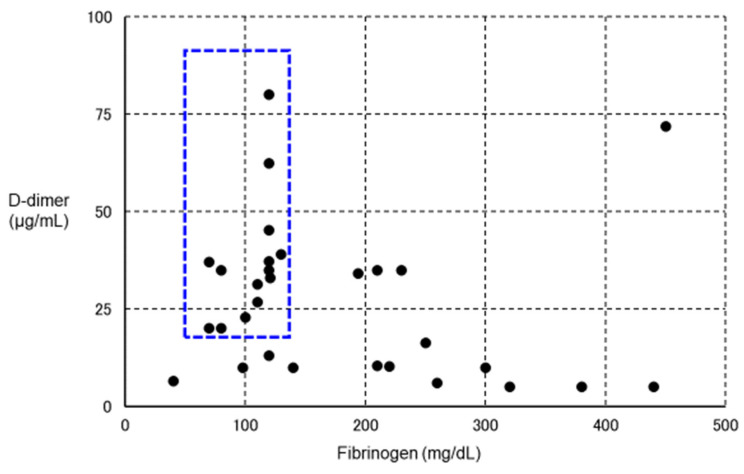
Figure 4.
Relationship between VITT and fibrinolytic pathophysiology. We plotted fibrinogen on the horizontal axis and D-dimer on the vertical axis for 30 definitive VITT cases (using data from Reference [222]) in which both fibrinogen and D-dimer values were known. The lower the level of fibrinogen, the higher the level of D-dimer. In particular, patients with blue dotted squares showed a decrease in fibrinogen and a marked increase in D-dimer, suggesting the complication of enhanced-fibrinolytic-type DIC (a subject for further investigation). If anticoagulants are administered to the same intensity as in other cases, the risk of bleeding is considered high. To confirm the diagnosis of enhanced-fibrinolytic-type DIC, measurement of not only the coagulation activation marker TAT, but also the fibrinolysis activation marker PIC is essential. Patients with markedly decreased α2PI are at high risk of bleeding. Importantly, in enhanced-fibrinolytic-type DIC, the increase in FDP is more prominent than the increase in D-dimer (discrepancy between FDP and D-dimer). Antithrombin, as a coagulation inhibitor, does not often decrease, even in patients with a marked decrease in α2PI, a fibrinolytic inhibitor (except in patients with reduced hepatic reserve). Abbreviations: VITT, vaccine-induced immune thrombotic thrombocytopenia; DIC, disseminated intravascular coagulation; TAT, thrombin–antithrombin complex; PIC, plasmin–α2 plasmin inhibitor complex; α2 PI, α2 plasmin inhibitor; FDP, fibrin/fibrinogen degradation products.