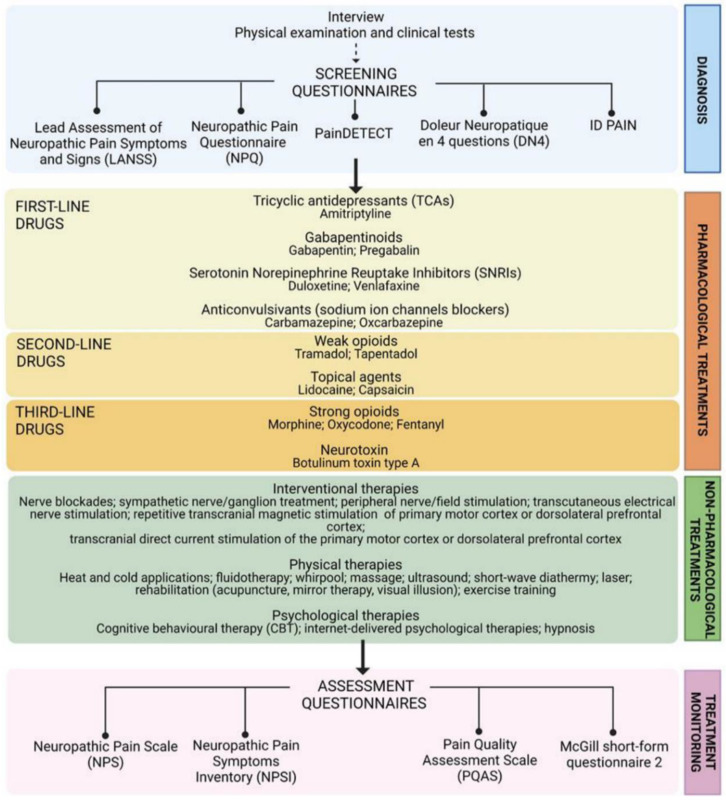
Figure 1.
Scheme of the multidisciplinary approach for the management of neuropathic pain. Patient interview, physical and clinical tests and screening questionnaires-Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) [14], Neuropathic Pain Questionnaire (NPQ) [15], painDETECT [16], Douleur Neuropathique en 4 Questions (DN4) [17], ID PAIN [18]—are the main steps of a comprehensive diagnosis [8] required to characterize neurological lesions, determine the presence of comorbidities, identify typical neuropathic symptoms and signs [19] and also assess the emotional, social, and economic impact of NP on patients’ lives [20]. Focusing on clinical symptoms rather than causative events/factors [2,10], NP treatment currently includes both pharmacological and non-pharmacological (interventional, physical, and psychological) options [8,9,10,21,22] whose efficacy and safety are constantly monitored with the following assessment questionnaires: Neuropathic Pain Scale (NPS) [23], Neuropathic Pain Symptoms Inventory (NPSI) [24], Pain Quality Assessment Scale (PQAS) [25], and the McGill short-form questionnaire 2 [26]. Among pharmacological options, according to the Grading of Recommendation, Assessment, Development and Evaluation (GRADE) system, gabapentinoids, tricyclic antidepressants (TCAs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and anticonvulsants (sodium ion channel blockers) are strongly recommended for use and proposed by international guidelines as first-line drugs; weak opioids, lidocaine patches, and 8% capsaicin patches are weakly recommended for use and classified as second-line drugs; strong opioids and botulinum toxin type A have only weak GRADE recommendation and are relegate among third-line drugs.