Abstract
Disease modification has become a well-established concept in several therapeutic areas; however, no widely accepted definition of disease modification exists for SLE.
We reviewed established definitions of disease modification in other conditions and identified a meaningful effect on ‘disease manifestations’ (ie, signs, symptoms and patient-reported outcomes) and on ‘disease outcomes’ (eg, long-term remission or progression of damage) as the key principles of disease modification, indicating a positive effect on the natural course of the disease. Based on these findings and the treatment goals and outcome measures for SLE, including lupus nephritis, we suggest a definition of disease modification based on disease activity indices and organ damage outcomes, with the latter as a key anchor. A set of evaluation criteria is also suggested.
Establishing a definition of disease modification in SLE will clarify which treatments can be considered disease modifying, provide an opportunity to harmonise future clinical trial outcomes and enable comparison between therapies, all of which could ultimately help to improve patient outcomes. This publication seeks to catalyse further discussion and provide a framework to develop an accepted definition of disease modification in SLE.
Keywords: lupus nephritis; therapeutics; lupus erythematosus, systemic; outcome assessment, health care
Key messages.
What is already known about this subject?
Disease modification has become a well-established concept in rheumatology and other therapeutic areas; however, in systemic lupus erythematosus (SLE), a definition of disease modification does not currently exist.
What does this study add?
We reviewed definitions of disease modification that exist in other diseases and identified meaningful effects on disease manifestations and outcomes as core principles of disease modification.
Guided by the established definitions of disease modification in other therapeutic areas along with current treatment goals and outcome measures in SLE, we propose a framework for the definition of disease modification in SLE. Organ damage prevention (or slowing), minimisation of disease activity, and avoidance of treatment-associated toxicities are the core components of successful disease modification.
This work, which provides criteria for a medication to be classified as a disease-modifying therapy, serves as a foundation for an exchange of ideas that could lead to further refinement of this concept in SLE.
How might this impact on clinical practice or future developments?
Establishing a definition of disease modification in SLE will provide a method to demonstrate the ability of a medication to modify the course of disease. This would not only be a powerful addition to clinical trial objectives but would also positively impact the care of patients.
Introduction
Disease modification is a well-known concept in rheumatology and other therapeutic areas.1–7 However, no widely accepted definition of disease modification exists for SLE. In this article, we explore the core principles of the definitions of disease modification in other conditions, and we propose a conceptual framework for the definition of disease modification in SLE. The demonstration of a medication’s capacity to modify the course of a disease would be a powerful addition to current clinical trial objectives and would ultimately help to improve patient care and clinical outcomes.
Natural history of SLE
SLE is a chronic inflammatory autoimmune disease with fluctuating periods of relative inactivity and disease flares in most patients.8 9 A loss of tolerance to ubiquitous self-antigens in SLE leads to an increase in the number of pathogenic autoantibodies, which drives inflammation and tissue injury, and the onset of clinical manifestations, which may culminate in irreversible tissue damage.10 11 SLE is heterogeneous in its clinical presentations, with multiple organs being affected by varying degrees of severity,9 12 13 which can lead to diagnostic delays and difficulties in evaluating therapeutic outcomes.10 13
Approximately 30%–50% of patients with SLE will develop organ damage within 5 years of diagnosis,14 15 and 50% or more by 10 years postdiagnosis.15 Patients with SLE-associated organ damage have worse health-related quality of life (HRQoL) and increased healthcare costs, morbidity and mortality versus patients with SLE who have lesser or no organ damage.16–23 Damage can develop in several different organ systems, including but not limited to the ocular, musculoskeletal, neuropsychiatric and renal systems.24 Patients with SLE frequently develop lupus nephritis (LN), which can progress to end-stage kidney disease (ESKD), with a 15-year risk ranging from 10% to 30% in patients with severe LN (class III, IV and V) to 44% (95% CI 32% to 56%) in patients with class IV LN.25 26 Organ damage results from potentially modifiable risks such as uncontrolled disease activity/severe flares, exposure to glucocorticoids and/or immunosuppressive therapies and hypertension.27–34 Other known risk factors for accelerated organ damage accrual include pre-existing organ damage, African-American race, older age at SLE diagnosis and male sex.34 35
Treatment goals and outcomes assessments in SLE
According to the European Alliance of Associations for Rheumatology (EULAR) recommendations for SLE management, treatment goals for SLE include control of disease activity; prevention of flares and organ damage; optimisation of HRQoL; and ultimately, prolongation of life. Control of disease activity in SLE should aim to achieve remission or low disease activity and prevent flares in all organs, while minimising treatment-associated toxicities, including exposure to glucocorticoids.36 In patients with LN, the goals of treatment also include preservation of kidney function and prevention of ESKD.37
The complex immunopathogenesis of SLE and heterogeneity of clinical manifestations present challenges in the assessments of outcomes and the designs of clinical trials.10 According to the Outcome Measures in Rheumatology Clinical Trials (OMERACT) initiative, the four core areas that should be assessed in clinical trials of SLE are disease activity, organ damage, HRQoL and adverse events/medication side effects (evaluation of economic cost may also be beneficial, where applicable).38 A summary of key outcome measures and instruments used in clinical trials of SLE and LN is shown in table 1. We will consider the EULAR recommendations for SLE management, the OMERACT areas and established SLE assessments and instruments with the aim of selecting those most suitable for framing a definition of disease modification in SLE that can help inform prescribers and patients. Where appropriate, measures specific to LN also will be considered.
Table 1.
Key outcome measures and instruments in SLE and LN for consideration in the definition of disease modification in SLE
| Type of outcome measure | Specific instrument |
| Disease activity indices/measures | SLEDAI, BILAG, SFI, CLASI*, uPCR†, kidney histological findings† |
| HRQoL measures and PROs | SF-36, FACIT-Fatigue scale, FSMC, EQ-5D, LIT, LupusQoL, LupusPRO |
| Global assessments | PGA, PtGA |
| Damage measures | SDI, eGFR decline >30%–40% and average eGFR slope reduction (>0.5–1.0 mL/min/1.73 m2 per year over a 2-year to 3-year follow-up period in RCTs)†, chronicity index progression on kidney biopsy/histology† |
| Responder indices | SLEDAI-based and BILAG-based responder indices (SRI-4 and BICLA), different composite indices based on uPCR, eGFR and rescue medications† |
*For mucocutaneous involvement.
†For LN.
BICLA, BILAG-based Combined Lupus Assessment; BILAG, British Isles Lupus Assessment Group; CLASI, Cutaneous Lupus Erythematosus Disease Area and Severity Index; eGFR, estimated glomerular filtration rate; EQ-5D, European Quality of Life Five Dimension; FACIT, Functional Assessment of Chronic Illness Therapy; FSMC, Fatigue Scale for Motor and Cognitive Functions; HRQoL, health-related quality of life; LIT, Lupus Impact Tracker; LN, lupus nephritis; LupusPRO, Lupus Patient-Reported Outcome; LupusQoL, Lupus Quality of Life; PGA, Physician Global Assessment; PRO, patient-reported outcome; PtGA, Patient/Parent Global Assessment; RCTs, randomised controlled trials; SDI, Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index; SELENA, Safety of Estrogens in Lupus Erythematosus National Assessment; SF-36, Medical Outcomes Survey Short Form-36; SFI, SELENA-SLEDAI Flare Index; SLEDAI, SLE Disease Activity Index; SRI-4, SLE Responder Index-4; uPCR, urinary protein-creatinine ratio.
How has disease modification been defined in other disease areas?
The concept of disease modification was first established in rheumatoid arthritis with the introduction of the term disease-modifying antirheumatic drugs in the 1980s and 1990s.39–41 The various definitions of disease modification across multiple therapeutic areas identified in our literature search are summarised in online supplemental table 1.
lupus-2021-000634supp001.pdf (261.3KB, pdf)
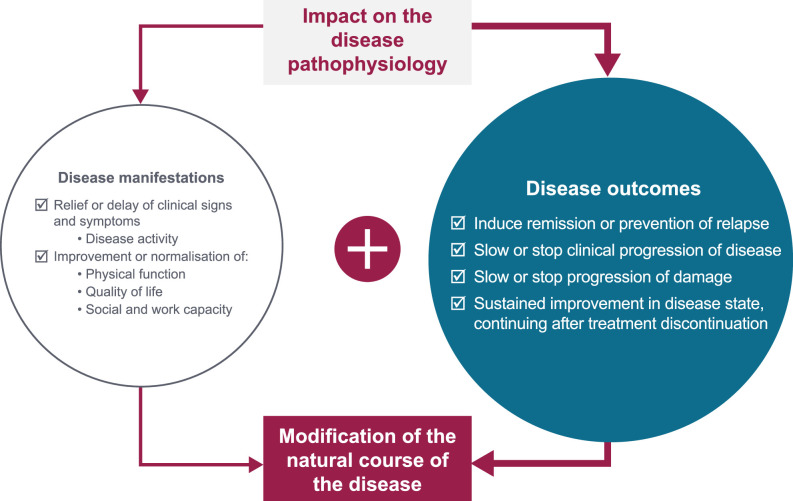
Across all the disease areas reviewed, affecting a progressive component or the natural course of the disease is central to the definition of disease modification (online supplemental table 1). Improving the signs and symptoms of the disease is a common component within most definitions, which sits alongside modifying the natural progression of the disease but never as a standalone component.1 7 42–44 Two definitions of disease modification therapies referred to those that induce remission or prevent relapses.3 45 The concept of an enduring effect was seen in the definition of disease modification in neurodegenerative disorders and respiratory diseases but not in the other disease areas.46–50 Impact on the disease pathophysiology and quality of life, and evaluation of biomarkers were not consistently included as specific components of a disease modification definition across the disease areas reviewed.7 44 47 48 51 52 Last, in the majority of disease areas, expert-led publications have led the way in setting out possible definitions of disease modification rather than guidance by regulatory authorities.
What are the considerations when defining disease modification in SLE?
Drawing on the definitions from other therapeutic areas, we developed a framework for the definition of disease modification. Two key considerations were incorporated into our formulation, disease manifestations (encompassing signs and symptoms (ie, disease activity) and patient-reported outcomes (PROs)) and disease outcomes (encompassing long-term remission and slowing or stopping organ damage accumulation), and we conceptualise how both considerations may be interpreted to define a long-term meaningful change in the disease course (figure 1).
Figure 1.
Components of the definitions of disease modification from disease areas other than SLE.
SLE disease activity is routinely assessed in clinical trials using established instruments, such as the SLE Disease Activity Index (SLEDAI)53 or the British Isles Lupus Assessment Group (BILAG) Disease Activity Index,54 or their modifications (table 1).55–58 Although these measurements are used commonly in clinical trials, they are infrequently used in clinical practice.59 60 The frequency and severity of SLE flares are indicators of global disease control and relevant in both clinical trials and in clinical practice but are not uniformly defined yet.59–62 Reduction in steroid use is a key treatment goal in SLE, due to an increased understanding of the risks associated with long-term exposure.36
Recently, treat-to-target objectives in SLE, in the form of the Definitions of Remission in SLE (DORIS) criteria,63 the Lupus Low Disease Activity State (LLDAS) criteria64 and low disease activity criteria,65 have been associated with reduced disease flares and organ damage accrual in patients with SLE.66–69 Inclusion of these measures, along with flare prevention and glucocorticoid reduction, could be considered key targets in the disease manifestations component of the proposed disease modification definition framework.
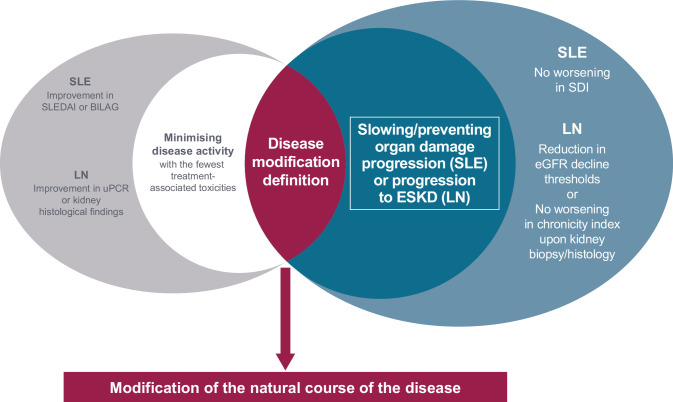
The Systemic Lupus International Collaborating Clinics (SLICC)/American College of Rheumatology (ACR) Damage Index (SDI) is a validated measure of organ damage in SLE. However, demonstrating significant effects of an intervention on damage accrual rates requires studies that are longer than 1 year in duration.70–75 In the absence of long-term trials, disease activity, a key driver of organ damage,76 could serve as an interim surrogate measure of organ damage progression to determine whether an intervention is on track to achieve disease modification. Therefore, assessment of both the SDI and key drivers of organ damage should form part of a definition of disease modification in SLE with the direct assessment on organ damage via SDI as the key anchor. In addition, it is particularly important that disease activity is only considered in conjunction with the fewest treatment-associated toxicities, because treatments such as glucocorticoids and immunosuppressants, which reduce SLE disease activity and flares, can promote organ damage progression.29 31–33
In LN, long-term assessment of disease outcomes is focused on slowing or preventing progression to ESKD; and these outcomes can be evaluated by kidney biopsy and other clinical measures of damage, including estimated glomerular filtration rate (eGFR) slope and chronic kidney disease (CKD) staging. Histological findings and chronicity indices determined by kidney biopsy are the gold-standard methods to assess the extent of tissue inflammation and damage.77 78 Histopathology can also be predictive of renal outcome, with fibrinoid necrosis, fibrous crescents and interstitial fibrosis/tubular atrophy ≥25% predictive of progression to ESKD.79 A collaborative effort between the US National Kidney Foundation, the Food and Drug Administration and the European Medicines Agency suggested an eGFR decline of >30%–40% and average eGFR slope reduction (of >0.5–1.0 mL/min/1.73 m2 per year over a 2-year to 3-year follow-up period in clinical trials) as accepted surrogate end points for CKD progression.80 81 Additionally, evaluating SDI at a later timepoint in patients with LN may be valuable to confirm that treatment-associated damage has not taken place.80 81
Improvement in HRQoL and PROs is an important treatment goal in SLE.36 37 82 PROs can be measured using generic instruments such as the 36-item Short-Form Health Survey (SF-36), the Patient Reported Outcomes Measurement Information System item-bank (PROMIS) and Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue scale, and disease-specific instruments, such as the Lupus Quality of Life (LupusQoL), the Lupus Patient-Reported Outcomes (LupusPRO) and the Lupus Impact Tracker (LIT).83 HRQoL in patients with SLE is complex and can be driven by the disease itself, by comorbid conditions associated with the disease or both; but the precise mechanism by which these processes affect HRQoL is not yet fully understood.84 As such, there is a lack of consensus on the best instrument for their quantification. Given these factors, and taking into account that HRQoL and PROs measures were included in only one disease modification definition (EULAR disease modification definition for RA),43 we suggest that HRQoL and PROs should be supportive elements of the disease modification definition in SLE for the time being.
Last, although definitions of disease modification in neurodegenerative disorders involve targeting the pathogenic mechanisms of the disease and biomarkers, this was not the case with the other disease areas. Indeed, in SLE there are a number of established immunological/serological biomarkers of disease, some of which (anti-double-stranded DNA immunoglobulin (Ig) G, anti-nucleosome IgG, anti-La IgG and anti-Sm IgG, interferon-inducible protein 10, monocytic chemotactic protein 1, macrophage inflammatory protein-3β and complement C3) may correlate with clinical measures of disease activity (using SLEDAI).85 However, the pathophysiology of SLE is complex and heterogeneous among patients and not yet fully elucidated;85 86 as such, there is no single, gold standard biomarker for assessing disease activity, rather a panel of biomarkers would likely be required. Additionally, improvement in clinical and immunological measures do not always occur to the same extent or over the same time course. In fact, immunological responses may mirror, precede or lag behind the clinical responses. Therefore, we felt there would be limited value including pathophysiology and/or biomarkers as a mandatory component of a disease modification definition in SLE; however, it could be considered as a supportive element.
Working definition of SLE-specific disease modification
Based on the framework developed from the definitions of disease modification in other areas, and the treatment goals and outcome measures for SLE, including LN, we suggest the following working definition of SLE disease modification:
'Disease modification in SLE requires minimising disease activity with the fewest treatment-associated toxicities and slowing or preventing organ damage progression (or, in the case of LN, progression to ESKD).'
The evaluation criteria for this working definition is shown in figure 2. The most definitive criteria are slowing or preventing organ damage progression in SLE as judged by no worsening in the SDI and, in LN, by showing a reduction or no worsening in key surrogates of progression to ESKD, that is, kidney histopathology or eGFR decline.
Figure 2.
Preliminary evaluation criteria for the working definition of disease modification in SLE and LN. BILAG, British Isles Lupus Assessment Group; eGFR, estimated glomerular filtration rate; ESKD, end-stage kidney disease; LN, lupus nephritis; SDI, Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index; SLEDAI, SLE Disease Activity Index; uPCR, urinary protein-creatinine ratio.
Application of SLE-specific disease-modifying criteria
The disease modification definition for SLE could be applied to both clinical trials and clinical practice (with the notable difference that clinical trials include a comparison arm while clinical practice does not) using specific measures at year 1 to determine an impact on minimising disease activity with the fewest treatment-associated toxicities and at year 5 or later to evaluate slowing or preventing organ damage progression, with interim measures suggested for years 2–5 to determine whether an intervention is on track for achieving disease modification at the 5-year mark, as outlined in table 2.
Table 2.
Proposed matrix for application of the SLE-specific disease modification criteria in clinical trials and clinical practice
| Disease Modification definition category | Interim timepoints for assessment of disease modification POTENTIAL in clinical trials (vs standard therapy alone) and clinical practice (no comparison) | Disease modification CONFIRMED | ||
| Outcomes year 1 | Outcomes years 2–5 | Outcomes year >5 |
||
| Extra renal | Minimising disease activity with minimal treatment-associated toxicity AND Slowing/Preventing organ damage progression |
|
|
No change in SDI or delayed progression |
| Renal | Minimising disease activity with minimal treatment-associated toxicity AND Slowing/Preventing organ damage progression |
|
|
No change in SDI or delayed progression |
*≤7.5 mg/day per 2019 EULAR SLE treatment guidelines and LLDAS;36 64 ≤5 mg/day per DORIS remission definition.63
BILAG, British Isles Lupus Assessment Group; DORIS, Definitions Of Remission In SLE; eGFR, estimated glomerular filtration rate; EULAR, European Alliance of Associations for Rheumatology; GC, glucocorticoid; LLDAS, Lupus Low Disease Activity State; SDI, Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index; SELENA, Safety of Estrogens in Lupus Erythematosus National Assessment; SFI, SELENA-SLEDAI Flare Index; SLEDAI, SLE Disease Activity Index; SRI-4, SLE Responder Index-4; uPCR, urinary protein-creatinine ratio.
The 1-year and 5-year timeframes were chosen to assess early markers and confirmed disease modification, respectively, based on thresholds for assessment of disease activity and organ damage in clinical trials and longitudinal studies.38 80 Examples of tools to be used to assess disease activity were provided, without specifying a single tool, to allow for evolution of this definition and how it can be assessed. A range of steroid thresholds are suggested to reflect the range recommended in treatment guidelines and criteria for remission and low disease activity state.36 63 64
Conclusions
Using the established definitions of disease modification from multiple conditions as a guide and taking into consideration SLE and LN treatment goals, we have put forward a definition of disease modification in SLE, with organ damage outcomes as the key anchor.
Establishing an accepted definition of disease modification in SLE presents the opportunity for harmonising future clinical trial outcomes and will enable comparison of treatments, which could ultimately lead to improved patient care and clinical outcomes.
This article provides a preliminary definition of disease modification in SLE and will require more formal evaluation and testing before a consensus definition can be adopted. However, we anticipate that this work will provide the foundation for debates on how to achieve disease modification in SLE and the criteria that must be met for a drug to be classified as a disease-modifying therapy. As several SLE treatments may fit the disease modification criteria proposed here, the application of the criteria to current treatments is the focus of an ongoing review.
Acknowledgments
Medical writing support was provided by Cristina Teles, PhD, of Fishawack Indicia, UK, and Hannah Jedrey, PhD, and Meer Basharat, PhD, of TVF Communications, UK, and was funded by GSK.
Footnotes
Twitter: @Lupusdoc
Contributors: The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors, take responsibility for the integrity of the work as a whole, contributed to the writing and reviewing of the manuscript and have given final approval for the version to be published.
Competing interests: RvV has received consulting fees from AbbVie, AstraZeneca, Biogen, Biotest, BMS, Galapagos, Gilead, Janssen, Pfizer, Sanofi, Servier, UCB and Vielabio; speaker honoraria with AbbVie, Galapagos, GSK, Janssen, Pfizer and UCB, and support for educational programmes and institutional grants from Pfizer and Roche. ADA has received consulting fees from AbbVie, Amgen, Aurinia, AstraZeneca, BMS and GSK; and has been an investigator for GSK, Janssen, Pfizer, UCB, Vielo, AstraZeneca and Eli Lilly. ASB has received consulting fees from Alexion, Principio, Calliditas, Aurinia, Catalyst, Travere, GSK, Visterra, Silence, Novo Nordisk, Otsuka, ChemoCentrx and Novartis. INB is a National Institute for Health Research (NIHR) Senior Investigator and is funded by the NIHR Manchester Biomedical Research Centre. His institution has received research grants from GSK and Genzyme/Sanofi and consultancy fees from GSK, UCB, Eli Lilly, BMS, Merck Serono, Aurinia and IL-TOO. INB has received speaker fees from GSK, AstraZeneca and UCB. MD’E has received consulting fees from Aurinia, AstraZeneca, Biogen, Gilead, Pfizer and GSK. AS has received research grant support from GSK, Novartis and Pfizer; and has been an advisory board and speaker bureau member for GSK. MBU has received research grant support from GSK and has been an advisory board and speaker bureau member for GSK, and an advisory board member for AstraZeneca, Eli Lilly and UCB. M-HZ has been a consultant or advisory board member for GSK, AstraZeneca and Roche. RF has received research support from GSK and is an advisory board member for GSK. AC, MD, RAL and HAQ are employees of GSK and hold stocks and shares in the company.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. JAMA 2018;320:1360–72. 10.1001/jama.2018.13103 [DOI] [PubMed] [Google Scholar]
- 2.American College of rheumatology . ACR glossary: disease modifying antirheumatic drugs (DMARDs), 2021. Available: https://www.rheumatology.org/Learning-Center/Glossary/ID/453
- 3.Finkelsztejn A. Multiple sclerosis: overview of disease-modifying agents. Perspect Medicin Chem 2014;6:65–72. 10.4137/PMC.S13213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morant AV, Jagalski V, Vestergaard HT. Labeling of disease-modifying therapies for neurodegenerative disorders. Front Med 2019;6:223. 10.3389/fmed.2019.00223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morant AV, Vestergaard HT, Lassen AB, et al. Us, EU, and Japanese regulatory guidelines for development of drugs for treatment of Alzheimer's disease: implications for global drug development. Clin Transl Sci 2020;13:652–64. 10.1111/cts.12755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olanow CW, Kieburtz K. Defining disease-modifying therapies for PD--a road map for moving forward. Mov Disord 2010;25:1774–9. 10.1002/mds.23288 [DOI] [PubMed] [Google Scholar]
- 7.European Medicines Agency . Guideline on the Clinical Investigation of Medicines for the Treatment of Alzheimer’s Disease, 2020. Available: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicines-treatment-alzheimers-disease-revision-2_en.pdf [Accessed Aug 2021].
- 8.American College of rheumatology . Lupus, 2020. Available: https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus [Accessed Sep 2021].
- 9.Györi N, Giannakou I, Chatzidionysiou K, et al. Disease activity patterns over time in patients with SLE: analysis of the Hopkins lupus cohort. Lupus Sci Med 2017;4:e000192. 10.1136/lupus-2016-000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Z, Davidson A. Taming lupus-a new understanding of pathogenesis is leading to clinical advances. Nat Med 2012;18:871–82. 10.1038/nm.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zamansky GB. Sunlight-induced pathogenesis in systemic lupus erythematosus. J Invest Dermatol 1985;85:179–80. 10.1111/1523-1747.ep12276644 [DOI] [PubMed] [Google Scholar]
- 12.Giles JL, Polak OJ, Landon J. Disease modifying drugs for rheumatological diseases: a brief history of everything. Adv Protein Chem Struct Biol 2020;120:313–48. 10.1016/bs.apcsb.2019.11.007 [DOI] [PubMed] [Google Scholar]
- 13.Gergianaki I, Bertsias G. Systemic lupus erythematosus in primary care: an update and practical messages for the general practitioner. Front Med 2018;5:161. 10.3389/fmed.2018.00161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Urowitz MB, Gladman DD, Ibañez D, et al. Evolution of disease burden over five years in a multicenter inception systemic lupus erythematosus cohort. Arthritis Care Res 2012;64:132–7. 10.1002/acr.20648 [DOI] [PubMed] [Google Scholar]
- 15.Chambers SA, Allen E, Rahman A, et al. Damage and mortality in a group of British patients with systemic lupus erythematosus followed up for over 10 years. Rheumatology 2009;48:673–5. 10.1093/rheumatology/kep062 [DOI] [PubMed] [Google Scholar]
- 16.Barber MRW, Hanly JG, Su L, et al. Economic evaluation of damage Accrual in an international systemic lupus erythematosus inception cohort using a multistate model approach. Arthritis Care Res 2020;72:1800–8. 10.1002/acr.24092 [DOI] [PubMed] [Google Scholar]
- 17.Fialho SCMS, Bonfá E, Vitule LF, et al. Disease activity as a major risk factor for osteonecrosis in early systemic lupus erythematosus. Lupus 2007;16:239–44. 10.1177/0961203307076771 [DOI] [PubMed] [Google Scholar]
- 18.Hanly JG, Urowitz MB, Gordon C, et al. Neuropsychiatric events in systemic lupus erythematosus: a longitudinal analysis of outcomes in an international inception cohort using a multistate model approach. Ann Rheum Dis 2020;79:356–62. 10.1136/annrheumdis-2019-216150 [DOI] [PubMed] [Google Scholar]
- 19.Tselios K, Urowitz MB. Cardiovascular and pulmonary manifestations of systemic lupus erythematosus. Curr Rheumatol Rev 2017;13:206–18. 10.2174/1573397113666170704102444 [DOI] [PubMed] [Google Scholar]
- 20.Keeling SO, Vandermeer B, Medina J, et al. Measuring disease activity and damage with validated metrics: a systematic review on mortality and damage in systemic lupus erythematosus. J Rheumatol 2018;45:1448–61. 10.3899/jrheum.171310 [DOI] [PubMed] [Google Scholar]
- 21.Mok CC, Ho LY, Cheung MY, et al. Effect of disease activity and damage on quality of life in patients with systemic lupus erythematosus: a 2-year prospective study. Scand J Rheumatol 2009;38:121–7. 10.1080/03009740802415527 [DOI] [PubMed] [Google Scholar]
- 22.Murimi-Worstell IB, Lin DH, Nab H, et al. Association between organ damage and mortality in systemic lupus erythematosus: a systematic review and meta-analysis. BMJ Open 2020;10:e031850. 10.1136/bmjopen-2019-031850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwarting A, Friedel H, Garal-Pantaler E, et al. The burden of systemic lupus erythematosus in Germany: incidence, prevalence, and healthcare resource utilization. Rheumatol Ther 2021;8:375–93. 10.1007/s40744-021-00277-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taraborelli M, Cavazzana I, Martinazzi N, et al. Organ damage accrual and distribution in systemic lupus erythematosus patients followed-up for more than 10 years. Lupus 2017;26:1197–204. 10.1177/0961203317693096 [DOI] [PubMed] [Google Scholar]
- 25.Tektonidou MG, Dasgupta A, Ward MM. Risk of end-stage renal disease in patients with lupus nephritis, 1971-2015: a systematic review and Bayesian meta-analysis. Arthritis Rheumatol 2016;68:1432–41. 10.1002/art.39594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yuan F, Wei F, Wang J, et al. Clinical aspects and risk factors of lupus nephritis: a retrospective study of 156 adult patients. J Int Med Res 2019;47:5070–81. 10.1177/0300060519871812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernatsky S, Boivin J-F, Joseph L, et al. Mortality in systemic lupus erythematosus. Arthritis Rheum 2006;54:2550–7. 10.1002/art.21955 [DOI] [PubMed] [Google Scholar]
- 28.Frodlund M, Reid S, Wetterö J, et al. The majority of Swedish systemic lupus erythematosus patients are still affected by irreversible organ impairment: factors related to damage accrual in two regional cohorts. Lupus 2019;28:1261–72. 10.1177/0961203319860198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gladman DD, Urowitz MB, Rahman P, et al. Accrual of organ damage over time in patients with systemic lupus erythematosus. J Rheumatol 2003;30:1955–9. [PubMed] [Google Scholar]
- 30.Hill DD, Eudy AM, Egger PJ, et al. Impact of systemic lupus erythematosus disease activity, hydroxychloroquine and NSAID on the risk of subsequent organ system damage and death: analysis in a single US medical centre. Lupus Sci Med 2021;8. 10.1136/lupus-2020-000446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sung Y-K, Hur NW, Sinskey JL, et al. Assessment of damage in Korean patients with systemic lupus erythematosus. J Rheumatol 2007;34:987–91. [PubMed] [Google Scholar]
- 32.Segura BT, Bernstein BS, McDonnell T, et al. Damage accrual and mortality over long-term follow-up in 300 patients with systemic lupus erythematosus in a multi-ethnic British cohort. Rheumatology 2020;59:524–33. 10.1093/rheumatology/kez292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lopez R, Davidson JE, Beeby MD, et al. Lupus disease activity and the risk of subsequent organ damage and mortality in a large lupus cohort. Rheumatology 2012;51:491–8. 10.1093/rheumatology/ker368 [DOI] [PubMed] [Google Scholar]
- 34.Bruce IN, O'Keeffe AG, Farewell V, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the systemic lupus international collaborating clinics (SLICC) inception cohort. Ann Rheum Dis 2015;74:1706–13. 10.1136/annrheumdis-2013-205171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petri M, Purvey S, Fang H, et al. Predictors of organ damage in systemic lupus erythematosus: the Hopkins lupus cohort. Arthritis Rheum 2012;64:4021–8. 10.1002/art.34672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 2019;78:736–45. 10.1136/annrheumdis-2019-215089 [DOI] [PubMed] [Google Scholar]
- 37.Fanouriakis A, Kostopoulou M, Cheema K, et al. 2019 update of the joint European League against rheumatism and European renal Association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis. Ann Rheum Dis 2020;79:713–23. 10.1136/annrheumdis-2020-216924 [DOI] [PubMed] [Google Scholar]
- 38.Strand V, Gladman D, Isenberg D, et al. Endpoints: consensus recommendations from OMERACT IV. outcome measures in rheumatology. Lupus 2000;9:322–7. 10.1191/096120300678828424 [DOI] [PubMed] [Google Scholar]
- 39.Buer JK. A history of the term "DMARD". Inflammopharmacology 2015;23:163–71. 10.1007/s10787-015-0232-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bunch TW, O'Duffy JD. Disease-Modifying drugs for progressive rheumatoid arthritis. Mayo Clin Proc 1980;55:161–79. [PubMed] [Google Scholar]
- 41.Fries JF. Safety issues related to DMARD therapy. J Rheumatol Suppl 1990;25:14–17. [PubMed] [Google Scholar]
- 42.Aletaha D, Smolen JS. The definition and measurement of disease modification in inflammatory rheumatic diseases. Rheum Dis Clin North Am 2006;32:9–44. vii.. 10.1016/j.rdc.2005.09.005 [DOI] [PubMed] [Google Scholar]
- 43.Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 2020;79:685–99. 10.1136/annrheumdis-2019-216655 [DOI] [PubMed] [Google Scholar]
- 44.European Medicines Agency . Guideline on Medicinal Products for the Treatment of Alzheimer’s Disease and Other Dementias. Available: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-medicinal-products-treatment-alzheimers-disease-other-dementias-revision-1_en.pdf [Accessed Aug 2021].
- 45.Nagaraja V, Matucci-Cerinic M, Furst DE, et al. Current and future outlook on disease modification and defining low disease activity in systemic sclerosis. Arthritis Rheumatol 2020;72:1049–58. 10.1002/art.41246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chorostowska-Wynimko J. Disease modification in emphysema related to alpha-1 antitrypsin deficiency. COPD 2016;13:807–15. 10.1080/15412555.2016.1178224 [DOI] [PubMed] [Google Scholar]
- 47.Cummings J. Disease modification and neuroprotection in neurodegenerative disorders. Transl Neurodegener 2017;6:25. 10.1186/s40035-017-0096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cummings J, Fox N. Defining disease modifying therapy for Alzheimer's disease. J Prev Alzheimers Dis 2017;4:109–15. 10.14283/jpad.2017.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Halpin DMG, Tashkin DP. Defining disease modification in chronic obstructive pulmonary disease. COPD 2009;6:211–25. 10.1080/15412550902918402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.PMDA . Issues to Consider in the Clinical Evaluation and Development of Drugs for Alzheimer’s Disease, 2020. Available: https://www.pmda.go.jp/files/000221585.pdf [Accessed Oct 2021].
- 51.Cummings JL, Defining CJL. Defining and labeling disease-modifying treatments for Alzheimer's disease. Alzheimers Dement 2009;5:406–18. 10.1016/j.jalz.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 52.Food and Drug Administration . Early Alzheimer’s Disease: Developing Drugs for Treatment Guidance for Industry, 2020. Available: https://www.fda.gov/media/110903/download
- 53.Bombardier C, Gladman DD, Urowitz MB, et al. Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on prognosis studies in SLE. Arthritis Rheum 1992;35:630–40. 10.1002/art.1780350606 [DOI] [PubMed] [Google Scholar]
- 54.Hay EM, Bacon PA, Gordon C, et al. The BILAG index: a reliable and valid instrument for measuring clinical disease activity in systemic lupus erythematosus. Q J Med 1993;86:447–58. [PubMed] [Google Scholar]
- 55.Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 2002;29:288–91. [PubMed] [Google Scholar]
- 56.Isenberg DA, Rahman A, Allen E, et al. BILAG 2004. development and initial validation of an updated version of the British Isles lupus assessment group's disease activity index for patients with systemic lupus erythematosus. Rheumatology 2005;44:902–6. 10.1093/rheumatology/keh624 [DOI] [PubMed] [Google Scholar]
- 57.Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with systemic lupus erythematosus. N Engl J Med 2005;353:2550–8. 10.1056/NEJMoa051135 [DOI] [PubMed] [Google Scholar]
- 58.Touma Z, Urowitz MB, Gladman DD. SLEDAI-2K for a 30-day window. Lupus 2010;19:49–51. 10.1177/0961203309346505 [DOI] [PubMed] [Google Scholar]
- 59.Yavuz S, Lipsky PE. Current status of the evaluation and management of lupus patients and future prospects. Front Med 2021;8:682544. 10.3389/fmed.2021.682544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thanou A, Jupe E, Purushothaman M, et al. Clinical disease activity and flare in SLE: current concepts and novel biomarkers. J Autoimmun 2021;119:102615. 10.1016/j.jaut.2021.102615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morand EF, Furie R, Tanaka Y, et al. Trial of Anifrolumab in active systemic lupus erythematosus. N Engl J Med 2020;382:211–21. 10.1056/NEJMoa1912196 [DOI] [PubMed] [Google Scholar]
- 62.Navarra SV, Guzmán RM, Gallacher AE, et al. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet 2011;377:721–31. 10.1016/S0140-6736(10)61354-2 [DOI] [PubMed] [Google Scholar]
- 63.van Vollenhoven R, Voskuyl A, Bertsias G, et al. A framework for remission in SLE: consensus findings from a large international Task force on definitions of remission in SLE (DORIS). Ann Rheum Dis 2017;76:554–61. 10.1136/annrheumdis-2016-209519 [DOI] [PubMed] [Google Scholar]
- 64.Franklyn K, Lau CS, Navarra SV, et al. Definition and initial validation of a lupus low disease activity state (LLDAS). Ann Rheum Dis 2016;75:1615–21. 10.1136/annrheumdis-2015-207726 [DOI] [PubMed] [Google Scholar]
- 65.Polachek A, Gladman DD, Su J, et al. Defining low disease activity in systemic lupus erythematosus. Arthritis Care Res 2017;69:997–1003. 10.1002/acr.23109 [DOI] [PubMed] [Google Scholar]
- 66.Petri M, Magder LS. Comparison of remission and lupus low disease activity state in damage prevention in a United States systemic lupus erythematosus cohort. Arthritis Rheumatol 2018;70:1790–5. 10.1002/art.40571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tani C, Vagelli R, Stagnaro C, et al. Remission and low disease activity in systemic lupus erythematosus: an achievable goal even with fewer steroids? real-life data from a monocentric cohort. Lupus Sci Med 2018;5:e000234. 10.1136/lupus-2017-000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zen M, Iaccarino L, Gatto M, et al. Lupus low disease activity state is associated with a decrease in damage progression in Caucasian patients with SLE, but overlaps with remission. Ann Rheum Dis 2018;77:104–10. 10.1136/annrheumdis-2017-211613 [DOI] [PubMed] [Google Scholar]
- 69.Ugarte-Gil MF, Mendoza-Pinto C, Reátegui-Sokolova C, et al. Achieving remission or low disease activity is associated with better outcomes in patients with systemic lupus erythematosus: a systematic literature review. Lupus Sci Med 2021;8:e000542. 10.1136/lupus-2021-000542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pons-Estel GJ, Alarcón GS, McGwin G, et al. Protective effect of hydroxychloroquine on renal damage in patients with lupus nephritis: LXV, data from a multiethnic US cohort. Arthritis Rheum 2009;61:830–9. 10.1002/art.24538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Molad Y, Gorshtein A, Wysenbeek AJ, et al. Protective effect of hydroxychloroquine in systemic lupus erythematosus. prospective long-term study of an Israeli cohort. Lupus 2002;11:356–61. 10.1191/0961203302lu203ra [DOI] [PubMed] [Google Scholar]
- 72.Fessler BJ, Alarcón GS, McGwin G, et al. Systemic lupus erythematosus in three ethnic groups: XVI. Association of hydroxychloroquine use with reduced risk of damage accrual. Arthritis Rheum 2005;52:1473–80. 10.1002/art.21039 [DOI] [PubMed] [Google Scholar]
- 73.Urowitz MB, Ohsfeldt RL, Wielage RC, et al. Comparative analysis of long-term organ damage in patients with systemic lupus erythematosus using belimumab versus standard therapy: a post hoc longitudinal study. Lupus Sci Med 2020;7. 10.1136/lupus-2020-000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Urowitz MB, Ohsfeldt RL, Wielage RC, et al. Organ damage in patients treated with belimumab versus standard of care: a propensity score-matched comparative analysis. Ann Rheum Dis 2019;78:372–9. 10.1136/annrheumdis-2018-214043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gatto M, Saccon F, Zen M, et al. Early disease and low baseline damage as predictors of response to belimumab in patients with systemic lupus erythematosus in a real-life setting. Arthritis Rheumatol 2020;72:1314–24. 10.1002/art.41253 [DOI] [PubMed] [Google Scholar]
- 76.Nossent J, Kiss E, Rozman B, et al. Disease activity and damage accrual during the early disease course in a multinational inception cohort of patients with systemic lupus erythematosus. Lupus 2010;19:949–56. 10.1177/0961203310366572 [DOI] [PubMed] [Google Scholar]
- 77.Austin HA, Muenz LR, Joyce KM, et al. Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int 1984;25:689–95. 10.1038/ki.1984.75 [DOI] [PubMed] [Google Scholar]
- 78.Birmingham DJ, Merchant M, Waikar SS, et al. Biomarkers of lupus nephritis histology and flare: deciphering the relevant amidst the noise. Nephrol Dial Transplant 2017;32:i71–9. 10.1093/ndt/gfw300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rijnink EC, Teng YKO, Wilhelmus S, et al. Clinical and histopathologic characteristics associated with renal outcomes in lupus nephritis. Clin J Am Soc Nephrol 2017;12:734–43. 10.2215/CJN.10601016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Levey AS, Gansevoort RT, Coresh J, et al. Change in albuminuria and GFR as end points for clinical trials in early stages of CKD: a scientific workshop sponsored by the National kidney Foundation in collaboration with the US food and drug administration and European medicines Agency. Am J Kidney Dis 2020;75:84–104. 10.1053/j.ajkd.2019.06.009 [DOI] [PubMed] [Google Scholar]
- 81.Levey AS, Inker LA, Matsushita K, et al. Gfr decline as an end point for clinical trials in CKD: a scientific workshop sponsored by the National kidney Foundation and the US food and drug administration. Am J Kidney Dis 2014;64:821–35. 10.1053/j.ajkd.2014.07.030 [DOI] [PubMed] [Google Scholar]
- 82.Carter SA, Gutman T, Logeman C, et al. Identifying outcomes important to patients with glomerular disease and their caregivers. Clin J Am Soc Nephrol 2020;15:673–84. 10.2215/CJN.13101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Izadi Z, Gandrup J, Katz PP, et al. Patient-Reported outcome measures for use in clinical trials of SLE: a review. Lupus Sci Med 2018;5:e000279. 10.1136/lupus-2018-000279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Elera-Fitzcarrald C, Fuentes A, González LA, et al. Factors affecting quality of life in patients with systemic lupus erythematosus: important considerations and potential interventions. Expert Rev Clin Immunol 2018;14:915–31. 10.1080/1744666X.2018.1529566 [DOI] [PubMed] [Google Scholar]
- 85.Smith MA, Henault J, Karnell JL, et al. Sle plasma profiling identifies unique signatures of lupus nephritis and discoid lupus. Sci Rep 2019;9:14433. 10.1038/s41598-019-50231-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mohan C, Putterman C. Genetics and pathogenesis of systemic lupus erythematosus and lupus nephritis. Nat Rev Nephrol 2015;11:329–41. 10.1038/nrneph.2015.33 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
lupus-2021-000634supp001.pdf (261.3KB, pdf)