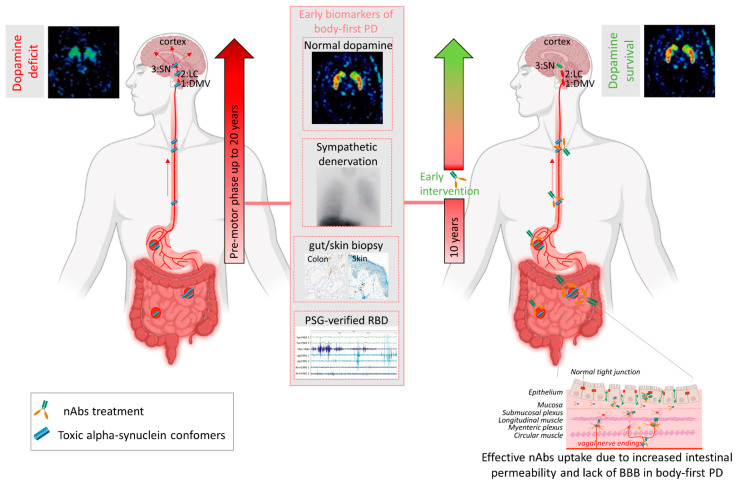
Figure 2.
Passive immunization of pre-motor body-first PD patients enhances dopamine survival. Patients with probable prodromal body-first PD could be identified by a combination of several early biomarkers, such as the presence of pathological alpha-synuclein (αsyn) in skin and/or gut biopsies, polysomnography-verified RBD, cardiac sympathetic denervation on MIBG scintigraphies, but normal or near-normal nigrostriatal dopaminergic innervation on DaT SPECT. Such detailed phenotyping in the pre-motor phase might reveal body-first PD, allowing early intervention and optimal patient selection for clinical trials. Pre-motor start of nAbs treatment increases treatment efficacy by delaying or blocking peripheral-to-brain propagation of pathology, before any irreversible damage to the dopamine system is done, hereby enhancing the probability of dopamine survival in body-first PD. Furthermore, increased gut permeability in prodromal body-first PD patients with ‘leaky gut’ or increased intestinal permeability might yield a better uptake of the administered nAbs near the source of pathogenic αsyn conformers, resulting in a better treatment efficacy, as opposed to brain-first cases where the source is located in the brain and only 0.1–0.2% of nAbs cross the blood–brain barrier. Abbreviations: nAbs: naturally occurring autoantibodies; DMV: dorsal motor nucleus of the vagus; LC: locus coeruleus; SN: substantia nigra, PAF: pure autonomic failure, PSG: polysomnography, BBB: blood brain barrier. Created using Biorender.com (accessed on 30 November 2021).