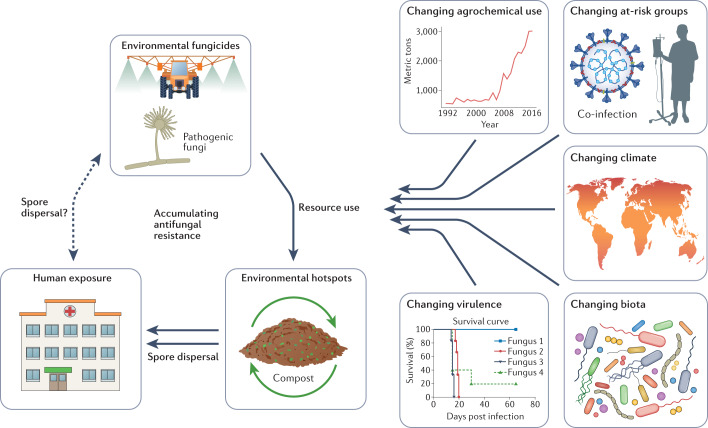
Fig. 2. Emerging antifungal resistance and environment–One Health drivers.
Fungi in the environment are exposed to broad-spectrum classes of antifungals that are also utilized as frontline antifungal treatments in the clinic. Ecological hotspots occur that can act as amplifiers of resistant genotypes. One example is green waste stockpiling and composting. Humans with invasive fungal diseases (IFDs) may also transmit resistant genotypes (for instance in nosocomial outbreaks); however, the extent to which humans and other animals contribute to the presence of antifungal resistance in the environment remains unknown. Multiple extrinsic factors exist that are expected to influence the incidence of antifungal resistance. These include changing patterns of fungicide use in the environment and in waste management33; changing at-risk human host groups including viral infections such as COVID-19; changing climates that may alter the geographical range of fungi and adaptive landscape for resistance50 as well as providing novel routes for infection (for example, natural disasters); changing biotic interactions that may include xenobiotic chemicals that are analogues to antifungals; and changing virulence of the fungi themselves owing to intrinsic genetic change or synergies with combinations of the above drivers47.