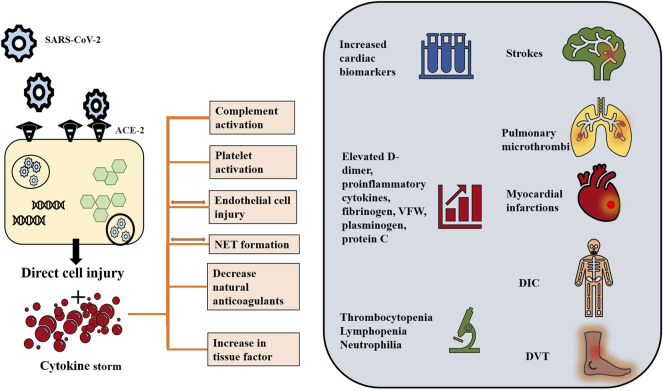
FIGURE 2.
COVID-19 induced hyperinflammatory and hypercoagulable states. Although the pathogenesis of COVID-19 induced coagulopathy has not been fully elucidated, interplay among immune dysregulation, hyperinflammation and thrombosis is proposed. SARS-CoV-2 virus, via its spike protein, interacts with the ACE-2 receptor to enter the cell through endocytosis. Endothelial cells as well as respiratory cells have high expression level of ACE-2. Inside the cell, the virus releases its genetic material and replicates using the cellular machinery. The viral effect is suggested to take place through two mechanisms: 1) Direct viral injury and 2) indirect cytokine-mediated injury. The viral cytopathic effect is implicated in direct damage and apoptosis of the host cell thus contributing to endothelitis. In turn, endothelial damage triggers platelet activation and aggregation. At the same time, the virus drives intense inflammation and immune dysregulation. It suppresses the lymphocytic activity and activates macrophages and polymorphonuclear cells, thus generating pro-inflammatory cytokines including IL-1, IL-2, IL-6, IL-10, IL-17, IL-18 and TNF-α, and leading to cytokine storm in severe illness. TF production, release of VWF and the initiation of coagulation cascade are triggered by cytokines and the injured epithelium. The cytokine storm also induces activation of complement system which contributes to coagulopathy by activating platelets, and increasing production of fibrin and thrombin. The cytokine storm is also associated with NETs, which in turn promotes VWF and TF activity and disables tissue factor inhibitor and thrombomodulin, therefore induing inflammation and microvascular thrombosis. These cellular processes are reflected on laboratory values, which ae usually remarkable for a combination of prolonged prothrombin time, normal to mildly prolonged activated partial thromboplastin time, thrombocytopenia, elevated D-dimer level, fibrinogen, fibrinogen degradation products, VFW, plasminogen, protein C, and factor VIII. Clinically, the hyperinflammatory response and endothelial dysfunction affect both venous and arterial systems. Venous thromboembolism includes pulmonary embolism and deep venous thrombosis. Arterial thromboembolism including myocardial injury and strokes have been also reported. Consumptive coagulopathy and ultimately DIC is also observed in critically ill patients (Lippi et al., 2020a; Iba et al., 2020b; Lippi et al., 2020b; Goshua et al., 2020; Guan et al., 2020; Levi and Thachil 2020; Mehta et al., 2020; Middleton et al., 2020; Tang et al., 2020; Varga et al., 2020; Zhang et al., 2020; Zhou et al., 2020; Tan et al., 2021). ACE-2: angiotensin converting enzyme-2; IL: Interleukin; VWF: von Willebrand factor; NET: neutrophil extracellular traps; TF: Tissue factor; DIC: disseminated intravascular coagulation.