Abstract
Objective:
To present cleft patients treated with protraction facemask and miniplate anchorage (FM/MP) in order to demonstrate the effects of FM/MP on maxillary hypoplasia.
Materials and Methods:
The cases consisted of cleft palate only (12 year 1 month old girl, treatment duration = 16 months), unilateral cleft lip and alveolus (12 year 1 month old boy, treatment duration = 24 months), and unilateral cleft lip and palate (7 year 2 month old boy, treatment duration = 13 months). Curvilinear type surgical miniplates (Martin, Tuttlinger, Germany) were placed into the zygomatic buttress areas of the maxilla. After 4 weeks, mobility of the miniplates was checked, and the orthopedic force (500 g per side, 30° downward and forward from the occlusal plane) was applied 12 to 14 hours per day.
Results:
In all cases, there was significant forward displacement of the point A. Side effects such as labial tipping of the upper incisors, extrusion of the upper molars, clockwise rotations of the mandibular plane, and bite opening, were considered minimal relative to that usually observed with conventional protraction facemask with tooth-borne anchorage.
Conclusions:
FM/MP can be an effective alternative treatment modality for maxillary hypoplasia with minimal unwanted side effects in cleft patients.
Keywords: Maxillary protraction, Facemask, Miniplate
INTRODUCTION
In Class III malocclusion patients with mild to moderate maxillary hypoplasia, the protraction facemask has been used to stimulate sutural growth at the circum-maxillary suture sites in growing patients.1–3 To transmit the orthopedic force from the protraction facemask to the maxilla, intraoral devices such as a labiolingual arch, quad helix, and rapid maxillary expansion (RME) have been used. However, the use of the upper dentition as anchorage cannot avoid unwanted side effects such as labioversion of the upper incisors, extrusion of the upper molars, counterclockwise rotation of the upper occlusal plane, and eventual clockwise rotation of the mandible.3–6 Therefore, labial inclined maxillary incisors and/or a vertical facial growth pattern would be contraindications for facemask therapy with tooth-borne anchorage.
To allow the direct transmission of orthopedic force to the circum-maxillary sutures, intentionally ankylosed primary canines, osseointegrated implants, and orthodontic miniscrews have been used as skeletal anchorage for protraction facemasks.7–11 Since surgical miniplates are a reliable means for applying orthodontic and orthopedic forces,12 Kircelli et al.,13 Cha et al.,14 and Kircelli and Pektas15 introduced the protraction facemask with miniplate anchorage (FM/MP) therapy to treat Class III malocclusion with maxillary hypoplasia and hypodontia (Figure 1).
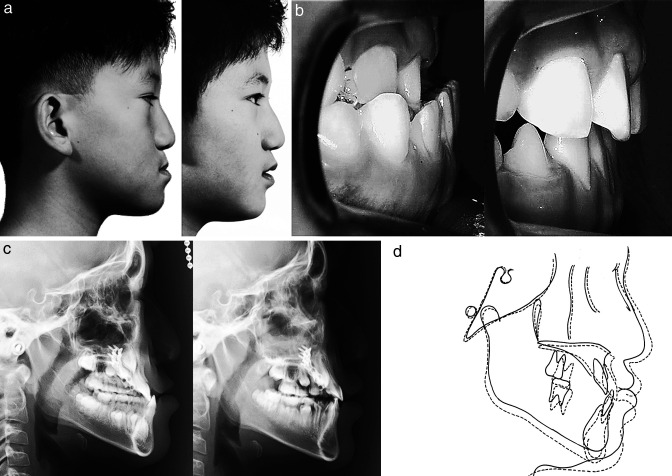
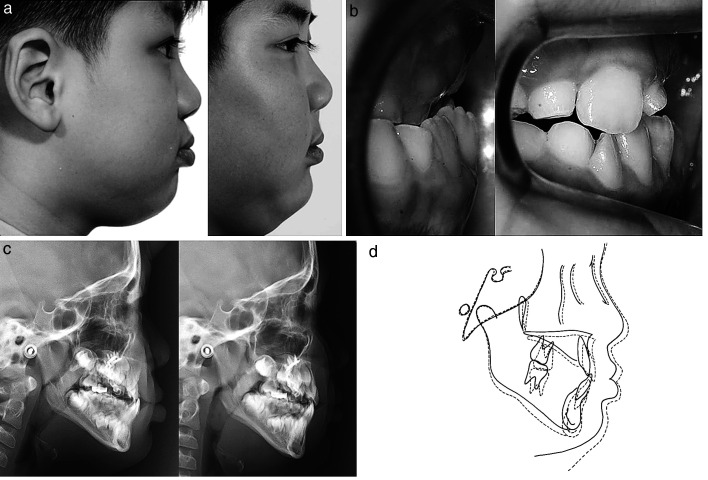
Figure 1.
Comparison of pretreatment (left) and posttreatment (right) in patient with Class III malocclusion. (a) Facial photographs. (b) Intraoral photographs. (c) Lateral cephalograms. (d) Superimposition (solid line: pretreatment; dotted line: posttreatment).
The protocol of FM/MP is as follows: (1) After an approximate 1–2 cm horizontal vestibular incision is made just below the zygomatic buttress area under local anesthesia, the zygomatic buttress is exposed with a subperiosteal flap. (2) Curvilinear type surgical miniplates (Martin, Tuttlinger, Germany) are bent according to the anatomical shape of the zygomatic buttress. (3) The distal end hole of the miniplate should be cut to make a hook for elastics. (4) After the miniplates are placed into the zygomatic buttress areas, three self-tapping type screws are used per side to fix the miniplates (Figure 2a). (5) The distal end of the miniplate should be exposed through the attached gingiva between the upper canine and first premolar to control the vector of elastic traction (Figure 2b). (6) Four weeks after placement of the miniplates, their mobility is checked and the orthopedic force (500 g per side, 30° downward and forward from the occlusal plane) is applied for 12 to 14 hours per day. (7) It is recommended to overcorrect the malocclusion into positive overjet and a slight Class II canine and molar relationship.
Figure 2.
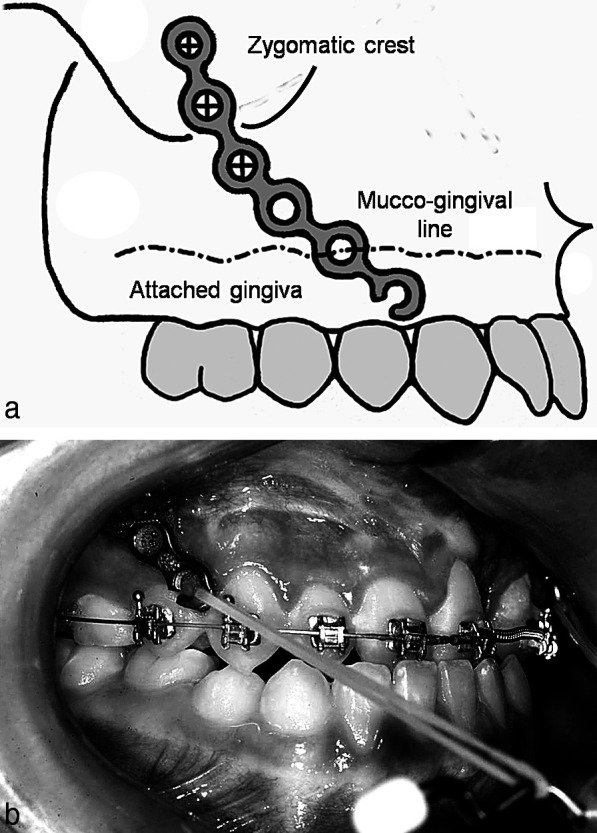
Schematic drawing of the surgical positioning (a) and intraoral position of the miniplate (b).
Cleft patients often develop Class III malocclusion with maxillary hypoplasia and vertical facial growth pattern due to the combined effects of the congenital deformity itself and the scar tissues after surgical repair.16 These are contraindications for conventional facemask therapy. However, little research has been done on the use of FM/MP in cleft patients. Therefore, the purpose of this case report is to present three cleft patients who were treated with FM/MP and to demonstrate the effect of FM/MP on maxillary hypoplasia in cleft patients.
CASE REPORTS
CASE 1
Skeletal Class III malocclusion with cleft palate (CP) and anterior open bite (Figure 3, Table 1).
Figure 3.
Comparison of pretreatment (left) and posttreatment (right) in patient with cleft palate (case 1). (a) Facial photographs. (b) Intraoral photographs. (c) Lateral cephalograms. (d) Superimposition (solid line: pretreatment; dotted line: posttreatment).
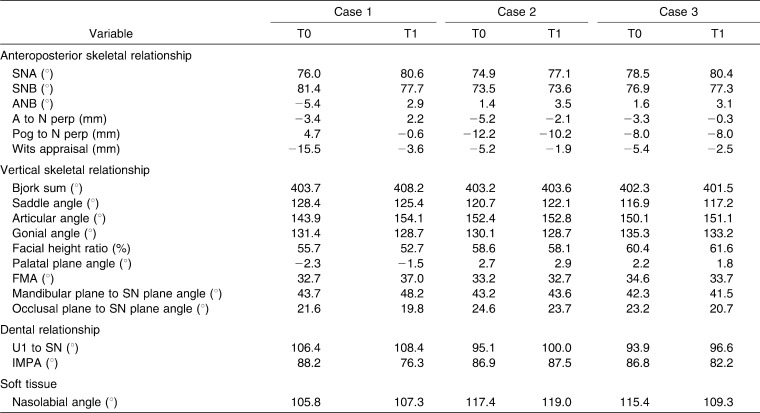
Table 1.
Comparison of the Skeletal, Dental, and Soft Tissue Variables Between Pretreatment (T0) and Posttreatment (T1)
Diagnosis
The patient was a 12 year 1 month old girl with CP only. She presented with concave facial profile, anterior crossbite (−9 mm overjet), and anterior open bite (−2 mm overbite). Cephalometric analysis showed skeletal Class III malocclusion with maxillary hypoplasia (ANB, −5.4°; A to N perp, −3.4 mm), steep mandibular plane angle (FMA, 32.7°), and a skeletal age after the pubertal growth spurt according to the cervical vertebrae maturation index (CVMI, stage 4).17 Her condition was one of the contraindications for conventional facemask therapy.
Treatment Plan
Although growth observation and reassessment after 2 years were proposed, her parents wanted to receive the FM/MP therapy. The possibility of orthognathic surgery after pubertal growth was explained.
Treatment Progress
FM/MP therapy was started 4 weeks after placement of the miniplates according to the protocol. During protraction, the fixed appliances were placed to align the dentition.
Treatment Results
After 16 months of FM/MP therapy, there was significant forward movement of the point A (ΔA to N perp, 5.6 mm). The ANB angle was changed from −5.4° to 2.9°, and a Class II canine and molar relationship, normal overbite, and overjet were obtained. A slight counterclockwise rotation of the occlusal plane angle (−1.8°) was interpreted to mean that there was almost no side effect such as extrusion of the upper molars. Although the FMA was increased 4.3°, the anterior open bite was corrected by downward and forward movement of the maxilla. Slight labial tipping of the upper incisors (ΔU1 to SN, 2.0°) occurred after correction of anterior crossbite and open bite.
CASE 2
Skeletal Class III malocclusion with unilateral cleft lip and alveolus (UCLA) and vertical facial growth pattern (Figure 4, Table 1).
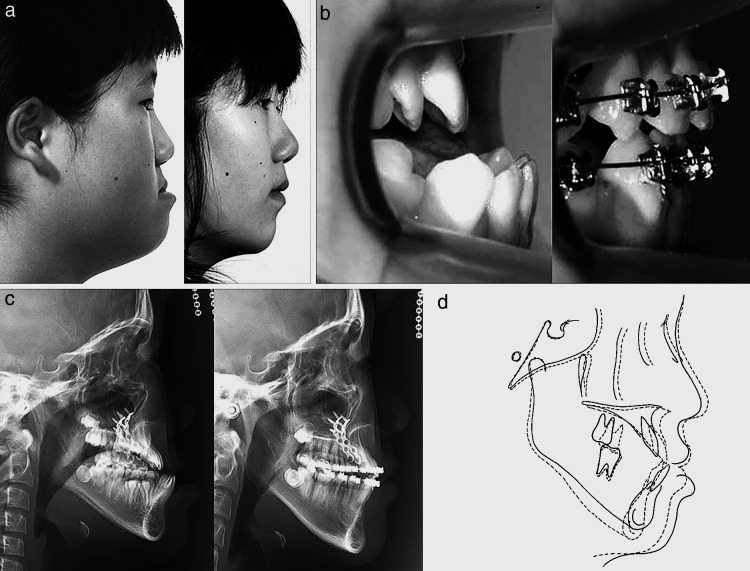
Figure 4.
Comparison of pretreatment (left) and posttreatment (right) in patient with unilateral cleft lip and alveolus (case 2). (a) Facial photographs. (b) Intraoral photographs. (c) Lateral cephalograms. (d) Superimposition (solid line: pretreatment; dotted line: posttreatment).
Diagnosis
The patient was a 12 year 1 month old boy with UCLA on the left side. Although he presented with a straight facial profile, he had an anterior crossbite (−2.5 mm overjet), upper anterior crowding, and peg laterals on the cleft side. Although the anteroposterior skeletal relationship (ANB, 1.4°) was within normal range and the upper and lower incisors were lingually inclined (U1 to SN, 95.1°; IMPA, 86.9°), a vertical facial growth pattern (FMA, 33.2°) existed. His skeletal age was before his pubertal growth spurt according to the CVMI (stage 3).17
Treatment Plan
Conventional facemask protraction with a tooth-borne anchorage device was not appropriate because the patient had a vertical facial growth pattern. Therefore, the FM/MP was used to avoid unwanted side effects.
Treatment Progress
Initially, the fixed orthodontic appliance was placed to correct the anterior crowding in the upper arch. The FM/MP therapy was started 4 weeks after placement of the miniplates according to the protocol.
Treatment Results
After 24 months of FM/MP therapy, there was a 3.1-mm forward movement of point A (ΔA to N perp). ANB angle was changed from 1.4° to 3.5°, and a Class II canine and molar relationship was obtained. The finding that there was a negligible counterclockwise rotation of the mandibular plane (0.4°) and occlusal plane angle (−0.9°) indicated that there were almost no side effects such as extrusion of the upper molars and bite opening. Labial tipping of the upper incisors (ΔU1 to SN, 4.9°) occurred due to alignment.
CASE 3
Skeletal Class III malocclusion with unilateral cleft lip and palate (UCLP) and vertical facial growth pattern (Figure 5, Table 1).
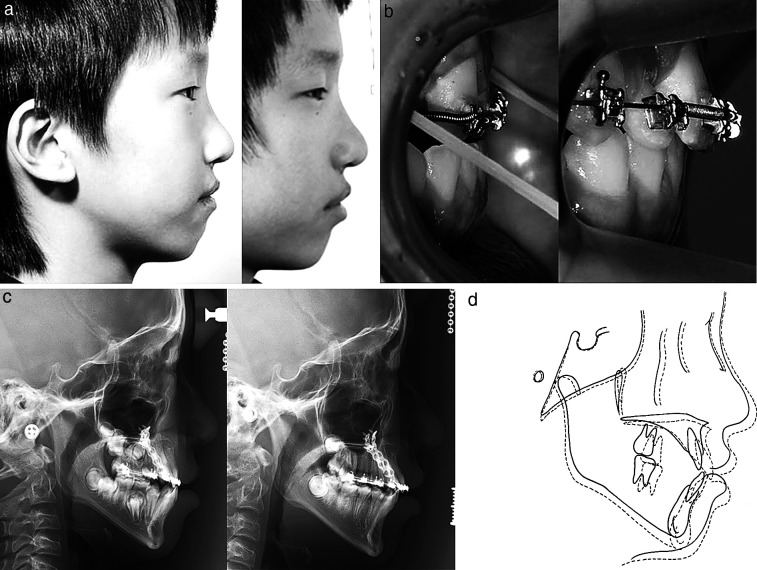
Figure 5.
Comparison of pretreatment (left) and posttreatment (right) in patient with unilateral cleft lip and palate (case 3). (a) Facial photographs. (b) Intraoral photographs. (c) Lateral cephalograms. (d) Superimposition (solid line: pretreatment; dotted line: posttreatment).
Diagnosis
The patient was a 7 year 2 month old boy with a UCLP on the right side. Although he presented with a straight facial profile, he had an anterior crossbite (−2.7 mm overjet). Although the anteroposterior skeletal relationship (ANB, 1.6°) was within normal range and the upper incisors were lingually inclined (U1 to SN, 93.9°), a vertical facial growth pattern existed (FMA, 34.6°). His skeletal age was before his pubertal growth spurt according to CVMI (stage 2).17
Treatment Plan
FM/MP was planned to maximize protraction of the maxilla and to avoid unwanted side effects.
Treatment Progress
FM/MP therapy was started 4 weeks after placement of the miniplates according to the protocol.
Treatment Results
Similar to Case 2, there was a 3.0-mm forward movement of point A (ΔA to N perp) after 13 months of protraction facemask therapy. The ANB angle was changed from 1.6° to 3.1°, and Class II canine and molar relationships were obtained. Although there was a slight counterclockwise rotation of the mandibular plane (−0.9°) and occlusal plane angle (−2.5°), there was no bite opening in the anterior teeth. Some labial tipping of the upper incisors (ΔU1 to SN, 2.7°) occurred after correction of the anterior crossbite.
DISCUSSION
Site for Placement of Miniplates
The zygomatic buttress area was used as the site for placement of the miniplates due to following reasons: (1) It has enough thickness and adequate bone quality.18 (2) It is near to the center of resistance of the nasomaxillary complex so that the force vector can be placed close to the center of rotation of the nasomaxillary complex.12,19
Vector Control
The direction of force vector was 30° downward and forward from the occlusal plane. Tanne et al.20 and Miyasaka-Hiraga et al.21 reported that downward and forward force produced uniform stretch and translatory repositioning of the nasomaxillary complex in an anterior direction. However, conventional dental anchorage usually results in counterclockwise rotation of the palatal plane, and clockwise rotation of the mandible, which would be unfavorable in a patient with vertical growth pattern.
The miniplate can transmit the orthopedic force directly to the maxilla and minimize rotational effect. Although there was a slight increase of FMA (4.3°) in Case 1, Cases 2 and 3 showed negligible changes of the palatal plane angle, FMA, and mandibular plane to SN angle (Table 1).
Conjunction with RME
Expansion of the maxilla before or during protraction of the maxilla has been performed to facilitate protraction by disarticulating the circum-maxillary sutures and initiating a cellular response in these sutures.1,3,5 Baik4 reported that there was more forward movement in the maxilla when protraction was in conjunction with RME compared with protraction without RME. Liou and Tsai22 presented the combined use of repeated rapid maxillary expansion and constriction and intraoral springs for maxillary protraction and concluded that significant advancement of the point A could be obtained.
However, a recent prospective, randomized clinical trial23 showed that facemask therapy, with or without RME, produced equivalent changes in the dentofacial complex and insisted that RME might not be indispensable to maxillary protraction unless a transverse deficiency exists. In our cases, we did not use RME because cleft lip and palate patients do not have some or whole parts of the midpalatal suture. Since this could affect the amount of maxillary advancement in cleft patients, further studies will be necessary.
Timing of Treatment
There are numerous articles that advocate the protraction therapy at an early stage.5,24–28 Because the palatomaxillary suture becomes highly interdigitated with increasing age, it becomes difficult to disarticulate the palatal bone from the pterygoid process.29 After the pubertal growth peak, side effects such as tooth movement and/or mandibular rotation rather than maxillary protraction are likely to be the major response to treatment.5,30 However, Baik4 and Sung and Baik31 insisted that there was no statistical difference when changes due to treatment were compared according to ages.
On the other hand, Kircelli and Pektas15 reported that protraction using the FM/MP in relatively older patients (11 to 13 years) was successful with minimum dentoalveolar side effects. We also confirmed that there was a significant maxillary protraction with fewer dentoalveolar side effects using the MP/FM in the patient after the pubertal growth peak and menarche (Case 1, CVMI stage 4).17
Comparison of the Amount of Maxillary Advancement
In cases of untreated Class III malocclusion with maxillary hypoplasia, Shanker et al.32 reported that point A came forward only 0.2 mm over a 6-month period. With conventional facemask therapy, Kim et al.33 from meta-analysis, reported that it produced 0.9 mm to 2.9 mm advancement of the point A. So25 insisted that the effect of protraction facemask therapy on the maxilla was two thirds skeletal and one third dental changes.
In cases with facemask and skeletal anchorage, amounts of the maxillary advancement have been reported to be 4.0 to 4.8 mm.9,15,34 Therefore, maxillary advancement can be enhanced by skeletal anchorage rather than conventional dental anchorage in growing patients.
In our cases, although a similar treatment protocol was used, the amounts of maxillary advancement varied according to cleft types (approximately 3.0 mm–5.6 mm). Since the duration of protraction (approximately 13–24 months) was relatively longer than in the other studies,9,15,34 the scar tissues of cleft patients can be one of the reasons for variations in the amount of maxillary protraction. This result was in accordance with Buschang et al.35 concerning limited protraction results in cleft patients.
Overcorrection
Ngan et al.36 and MacDonald et al.37 insisted that facemask therapy does not normalize the forward growth of the maxilla and that patients resume a Class III growth pattern by deficient maxillary growth during the follow-up period. Therefore, overcorrection into Class II canine and molar relationships is mandatory to compensate for deficient posttreatment maxillary growth.
Cleft patients seem to need more overcorrection than ordinary Class III malocclusion cases with maxillary hypoplasia because there are limitations in the amounts of maxillary advancement and a high relapse rate due to scar tissues.38 If the amount of maxillary advancement is large and the patients and parents want a relatively short-term treatment, distraction osteogenesis during adolescence or orthognathic surgery in adulthood can be recommended.
Advantages of FM/MP in Cleft Patients
In adolescent cleft patients, multiple orthodontic treatment procedures such as alignment, leveling, arch expansion, and preparation for bone graft surgery are needed. Because the miniplates are independent from dentition, simultaneous orthodontic treatment and maxillary protraction is an attractive advantage.
The FM/MP can be used over a relatively longer period than conventional facemask because it is independent of the upper dentition. According to Ishikawa et al.,39 the effects of conventional facemask therapy were significantly less in the second year, and no benefit from any treatment longer than 1 year was established. However, we confirmed that FM/MP could result in uniform advancement of the maxilla during the entire treatment period (Table 1).
In addition, cleft patients have more vertical growth pattern than noncleft patients,40 and excessive clockwise rotation of the mandible during facemask therapy can worsen the facial profile. FM/MP can minimize clockwise rotation of the mandible and prevent aggravation of the facial profile.
CONCLUSION
FM/MP can be an effective alternative treatment modality for cleft patients with maxillary hypoplasia with minimal unwanted side effects.
REFERENCES
- 1.McNamara J. A. An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21:598–608. [PubMed] [Google Scholar]
- 2.Delaire J. Maxillary development revisited: relevance to the orthopaedic treatment of Class III malocclusions. Eur J Orthod. 1997;19:289–311. doi: 10.1093/ejo/19.3.289. [DOI] [PubMed] [Google Scholar]
- 3.Nartallo-Turley P. E, Turley P. K. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998;68:217–224. doi: 10.1043/0003-3219(1998)068<0217:CEOCPE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Baik H. S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 5.Kapust A. J, Sinclair P. M, Turley P. K. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 6.Hickham J. H. Maxillary protraction therapy: diagnosis and treatment. J Clin Orthod. 1991;25:102–113. [PubMed] [Google Scholar]
- 7.Kokich V. G, Shapiro P. A, Oswald R, Koskinen-Moffett L, Clarren S. K. Ankylosed teeth as abutments for maxillary protraction: a case report. Am J Orthod. 1985;88:303–307. doi: 10.1016/0002-9416(85)90129-0. [DOI] [PubMed] [Google Scholar]
- 8.Silva Filho O. G, Ozawa T. O, Okada C. H, Okada H. Y, Carvalho R. M. Intentional ankylosis of deciduous canines to reinforce maxillary protraction. J Clin Orthod. 2003;37:315–320. [PubMed] [Google Scholar]
- 9.Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003;123:571–577. doi: 10.1067/mod.2003.S0889540603000520. [DOI] [PubMed] [Google Scholar]
- 10.Hong H, Nagn P, Li H. G, Qi L. G, Stephen H. Y. Use of onplants as stable anchorage for facemask treatment. Angle Orthod. 2005;75:453–460. doi: 10.1043/0003-3219(2005)75[453:UOOASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Vachiramon A, Urata M, Kyung H. M, Yamashita D. D, Yen S. L. Clinical applications of orthodontic microimplant anchorage in craniofacial patients. Cleft Palate Craniofac J. 2009;46:136–146. doi: 10.1597/06-219.1. [DOI] [PubMed] [Google Scholar]
- 12.Umemori M, Sugawara J, Mitani H, Nagasaka H, Kamamura H. Skeletal anchorage for open-bite correction. Am J Orthod Dentofacial Orthop. 1999;115:166–174. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- 13.Kircelli B. H, Pektaş Z. O, Uçkan S. Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Angle Orthod. 2006;76:156–163. doi: 10.1043/0003-3219(2006)076[0156:OPWSAI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Cha B. K, Lee N. K, Choi D. S. Maxillary protraction treatment of skeletal Class III children using miniplates anchorage. Korean J Orthod. 2007;37:73–84. [Google Scholar]
- 15.Kircelli B. H, Pektas Z. O. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Baek S. H, Moon H. S, Yang W. S. Cleft type and Angle's classification of malocclusion in Korean cleft patients. Eur J Orthod. 2002;24:647–653. doi: 10.1093/ejo/24.6.647. [DOI] [PubMed] [Google Scholar]
- 17.Hassel B, Farman A. G. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]
- 18.Sugawara J, Nishimura M, Nagasaka H, Kawamura H. Skeletal Anchorage System Using Orthodontic Miniplates. Vol. 15. St Louis, Mo: Mosby; 2009. Temporary anchorage devices in orthodontics; p. 320. [Google Scholar]
- 19.Tanne K, Matsubara S, Sakuda M. Location of the centre of resistance for the nasomaxillary complex studied in a three dimensional finite element model. Br J Orthod. 1995;22:227–232. doi: 10.1179/bjo.22.3.227. [DOI] [PubMed] [Google Scholar]
- 20.Tanne K, Hiraga J, Kakiuchi K, Yamagata Y, Sakuda M. Biomechanical effect of anteriorly directed extraoral forces on the craniofacial complex: a study using the finite element method. Am J Orthod Dentofacial Orthop. 1989;95:200–207. doi: 10.1016/0889-5406(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 21.Miyasaka-Hiraga J, Tanne K, Nakamura S. Finite element analysis for stresses in the craniofacial sutures produced by maxillary protraction forces applied at the upper canines. Br J Orthod. 1994;21:343–348. doi: 10.1179/bjo.21.4.343. [DOI] [PubMed] [Google Scholar]
- 22.Liou E. J, Tsai W. C. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005;42:121–127. doi: 10.1597/03-107.1. [DOI] [PubMed] [Google Scholar]
- 23.Vaughn G. A, Mason B, Moon H. B, Turley P. K. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005;128:299–309. doi: 10.1016/j.ajodo.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 24.Tindlund R. S. Orthopaedic protraction of the midface in the deciduous dentition. Results covering 3 years out of treatment. J Craniomaxillofac Surg. 1989;17(suppl 1):17–9. doi: 10.1016/s1010-5182(89)80032-0. [DOI] [PubMed] [Google Scholar]
- 25.So L. L. Effects of reverse headgear treatment on sagittal correction in girls born with unilateral complete cleft lip and cleft palate—skeletal and dental changes. Am J Orthod Dentofacial Orthop. 1996;109:140–147. doi: 10.1016/s0889-5406(96)70174-9. [DOI] [PubMed] [Google Scholar]
- 26.Saadia M, Torres E. Sagittal changes after maxillary protraction with expansion in Class III patients in the primary, mixed, and late mixed dentitions: a longitudinal retrospective study. Am J Orthod Dentofacial Orthop. 2000;117:669–680. [PubMed] [Google Scholar]
- 27.Suda N, Suzukl M. I, Hirose K, Hiyama S, Suzuki S, Kuroda T. Effective treatment plan for maxillary protraction: is the bone age useful to determine the treatment plan? Am J Orthod Dentofacial Orthop. 2000;118:56–62. doi: 10.1067/mod.2000.104491. [DOI] [PubMed] [Google Scholar]
- 28.Franchi L, Baccetti T, McNamara J. A., Jr Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 29.Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod. 1982;82:329–342. doi: 10.1016/0002-9416(82)90467-5. [DOI] [PubMed] [Google Scholar]
- 30.Cha K. S. Skeletal changes of maxillary protraction in patients exhibiting skeletal class III malocclusion: a comparison of three skeletal maturation groups. Angle Orthod. 2003;73:26–35. doi: 10.1043/0003-3219(2003)073<0026:SCOMPI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Sung S. J, Baik H. S. Assessment of skeletal and dental changes by maxillary protraction. Am J Orthod Dentofacial Orthop. 1998;114:492–502. doi: 10.1016/s0889-5406(98)70168-4. [DOI] [PubMed] [Google Scholar]
- 32.Shanker S, Ngan P, Wade D, Beck M, Yiu C, Hägg U, Wei S. H. Cephalometric A point changes during and after maxillary protraction and expansion. Am J Orthod Dentofacial Orthop. 1996;110:423–430. doi: 10.1016/s0889-5406(96)70046-x. [DOI] [PubMed] [Google Scholar]
- 33.Kim J. H, Viana M. A, Graber T. M, Omerza F. F, BeGole E. A. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115:675–685. doi: 10.1016/s0889-5406(99)70294-5. [DOI] [PubMed] [Google Scholar]
- 34.Singer S. L, Henry P. J, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Buschang P. H, Porter C, Genecov E, Genecov D, Sayler K. E. Facemask therapy of preadolescents with unilateral cleft lip and palate. Angle Orthod. 1994;64:145–150. doi: 10.1043/0003-3219(1994)064<0145:FMTOPW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Ngan P. W, Hagg U, Yiu C, Wei S. H. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod. 1997;3:255–264. doi: 10.1016/s1073-8746(97)80058-8. [DOI] [PubMed] [Google Scholar]
- 37.MacDonald K. E, Kapust A. J, Turley P. K. Cephalometric changes after the correction of Class III malocclusion with maxillary expansion/facemask therapy. Am J Orthod Dentofacial Orthop. 1999;116:13–24. doi: 10.1016/S0889-5406(99)70298-2. [DOI] [PubMed] [Google Scholar]
- 38.Baek S. H, Lee J. K, Lee J. H, Kim M. J, Kim J. R. Comparison of treatment outcome and stability between distraction osteogenesis and LeFort I osteotomy in cleft patients with maxillary hypoplasia. J Craniofac Surg. 2007;18:1209–1215. doi: 10.1097/scs.0b013e31814b2b8c. [DOI] [PubMed] [Google Scholar]
- 39.Ishikawa H, Kitazawa S, Iwasaki H, Nakamura S. Effects of maxillary protraction combined with chin-cap therapy in unilateral cleft lip and palate patients. Cleft Palate Craniofac J. 2000;37:92–97. doi: 10.1597/1545-1569_2000_037_0092_eompcw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 40.Van den Dungen G. M, Ongkosuwito E. M, Aartman I. H, Prahl-Andersen B. Craniofacial morphology of Dutch patients with bilateral cleft lip and palate and noncleft controls at the age of 15 years. Cleft Palate Craniofac J. 2008;45:661–666. doi: 10.1597/07-166.1. [DOI] [PubMed] [Google Scholar]