Abstract
The recently emerging coronavirus, severe acute respiratory syndrome coronavirus 2, (SARS-CoV-2) is the causative agent of the Coronavirus disease 2019 (COVID-19) pandemic. Since its discovery in the city of Wahan, China, SARS-CoV-2 has spread rapidly to invade all countries. In addition to its rapid transmission rate, it is characterized by high genetic mutation rates. The aim of this study is to provide an effective method for the isolation and propagation of SARS-CoV-2 in cell lines without any induction of genetic variations. In this study, we isolated SARS-CoV-2 from oro-nasopharyngeal swabs collected from Egyptian patients who were clinically diagnosed with COVID-19. Molecular identification of SARS-CoV-2 was performed by Real-Time Quantitative Reverse Transcription PCR (RT-qPCR). The isolated virus was propagated on Vero E6 cells without applying serial viral passages to avoid any variation of the viral genome. The replication and propagation were confirmed by the results of both RT-qPCR and the cytopathic effect (CPE). Moreover, SARS-CoV-2 was completely inactivated chemically using beta-propiolactone (βPL). Whole genome sequencing (WGS) of the propagated virus was performed in order to investigate mutational patterns. The genome sequences recovered in 2020 (n = 18) were similar to the reference strain, Wuhan-Hu-1, and were clustered as clade 20A. However, the genomic sequences recovered in 2021 (n = 2) were clustered as clade 21J. These two sequences are considered the first Delta (B.1.617.2) variants detected in Egypt. This study provides a reference for researchers in Egypt to isolate and propagate SARS-CoV-2 easily and efficiently. Furthermore, the prevalence of the SARS-CoV-2 delta variant in Egypt necessitates continuous monitoring of the efficacy of the applied treatment protocol and the effectiveness of current vaccines against such variants of concern (VOC).
Keywords: SARS-CoV-2, Isolation, Propagation, RT-qPCR, Delta variant, Variant of concern
1. Introduction
Coronaviruses are enveloped, spherical, positive-sense ssRNA viruses. They cause variable clinical features in the respiratory, digestive, and reproductive systems of a variety of hosts, such as birds and mammals (Cui et al., 2019; Monchatre-Leroy et al., 2017; Kim et al., 2020). Coronaviruses have a genome of 27–32 kb, which encodes non-structural proteins involved in replication, structural proteins, and viral transcription, which include nucleocapsids, membranes, envelopes, and spike proteins. In addition, the genome contains species-specific accessory genes. Coronaviruses are divided into four genera: the alpha-, beta-, gamma-, and deltacoronaviruses belonging to the family Coronaviridae which comprises two sub-families (Orthocoronavirinae and Letovirinae), 5 genera, 26 sub-genera, and 46 species (Cui et al., 2019; Wang et al., 2020; Brian and Baric, 2005). Of coronaviruses, seven members are known to cause human infection. Four of these seven coronaviruses, namely, NL63, HKU1, 229E, and OC43, cause mild symptoms. On the other hand, SARS-CoV, MERS-CoV, and SARS-CoV-2 may cause severe symptoms (Kim et al., 2020; Corman et al., 2018; De Wit et al., 2016; TaŞtan et al., 2020; Andersen et al., 2020). The etiologic agent of COVID-19 is SARS-CoV-2 which belongs to the betacoronaviruses and was first identified as the causative agent of the pneumonia outbreak in Wuhan, China, in 2019 that expanded worldwide to cause a pandemic (Wang et al., 2020; TaŞtan et al., 2020; Holshue et al., 2020; Zhu et al., 2020; Harcourt et al., 2020; Lai et al., 2020).
According to SARS-CoV-2 dissemination patterns, it can be transmitted from person to person, and it may be more transmissible than SARS-CoV and MERS-CoV (Harcourt et al., 2020; Li et al., 2020; Chan et al., 2020). The recently announced numbers of confirmed positive cases and deaths due to COVID-19 emphasize the global threat of the COVID-19 pandemic. As of March 22nd, 2022, the World Health Organization (WHO) declared that 470,839,745 confirmed cases, with 6,092,933 deaths, have been reported worldwide (World Health Organization, 2022a). In Egypt, the first COVID-19 case was reported in February 2020. In three months, the number of cases increased to 10,000 (Medhat and El Kassas, 2020). According to the WHO updates, 500,889 confirmed cases and 24,361 deaths have been reported in Egypt as of March 22nd, 2022 (World Health Organization, 2022b).
Several studies were conducted to study the characteristics of SARS-CoV-2 in order to determine the viral genome variants that play a crucial role in its transmission. Since its discovery, SARS-CoV-2 has shown massive variations in the genome overtime (van Dorp et al., 2020; Hamed et al., 2021; Garcia-Beltran et al., 2021). The phylogenetic analysis is necessary to understand the evolutionary picture of SARS-CoV-2. In 2020, 144 Egyptian SARS-CoV-2 isolates were found to have at least 99% identity to the reference strain Wuhan-Hu-1 and exhibited a distinct mutation pattern (D614G/Q57H/V5F/G823S) (Seadawy et al., 2022). During the second wave of the pandemic, the genomic sequences of SARS-CoV-2 were dramatically changed, resulting in several variants that were assigned as variants of concern (VOC) according to the WHO (Alotaibi et al., 2022).
Previous studies have shown that serial propagation of SARS-CoV-2 in Vero E6 cells results in rapid increases in genetic variants. Significant changes in the furin cleavage site (FCS) have a major impact on evolutionary studies, vaccine development, and antiviral drug discovery (Jureka et al., 2020; Funnell et al., 2021; Ogando et al., 2020). Due to the huge number of COVID-19 reported cases in Egypt and how COVID-19 affects the Egyptian public health and economy, it is crucial to effectively propagate and isolate SARS-CoV-2 from Egyptian patients for further molecular characterization studies.
The aim of our study was to establish a standardized protocol for working with the virus in order to isolate RNA from the virus and virus-infected cells without affecting the viral genome. Therefore, we collected oropharyngeal and nasopharyngeal specimens from Egyptian patients with COVID-19 symptoms. A specific RT-qPCR kit was used to identify SARS-CoV-2 positive specimens. We used Vero E6 cells to propagate and isolate SARS-CoV-2 from the positive specimens. Our results showed effective replication and propagation of the virus as indicated by the RT-qPCR technique. The full genome of the propagated virus from twenty samples recovered in 2020 and 2021 was sequenced and submitted to NCBI and GISAID database. Moreover, we performed phylogenetic analysis in order to follow the evolutionary pattern of SARS-CoV-2 in Egypt.
2. Materials and methods
2.1. Ethics statement
All patients gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by Princess Nourah Bint Abdul Rahman, PNU Institutional Review Board (IRB Registration Number with KACST, KSA: H-01-R-059 and IRB Log Number: 20–0457) and the Research Ethics Committee of Faculty of Pharmacy, Tanta University. After receiving authorization from Almaza Military Hospital's head, samples were collected.
2.2. Specimen collection and transportation
Patients with COVID-19 symptoms in Almaza Military Hospital had oropharyngeal and nasopharyngeal swabs collected. A transportation medium of DMEM supplemented with 2% FBS, ampicillin 100 IU/mL, and streptomycin 100 g/mL was utilized for specimen transportation. The specimens were transported in the transportation medium at 4 °C in a biosafety transporting device to the Egyptian Army's Biological Prevention department under strict biosafety conditions. For viral culture, Vero E6 cells were employed. The Vero E6 cell line was kept in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and incubated at 37 °C with 5% CO2.
2.3. Molecular identification by RT-qPCR
RNA was extracted from the samples using QIAamp Viral RNA mini kit (QIAGEN, Hilden, Germany) according to the guidelines. Molecular identification of SARS-CoV-2 was done using Viasure® SARS-CoV-2 Real Time PCR Detection Kit (ref. VS-NCO212H) targeting ORF1ab and N genes. According to the manufacturer's instructions, 15 μL of rehydration buffer was added to each well to rehydrate the master mix, followed by the addition of 5 μL of the extracted RNA. Positive and negative controls were included in the kit to validate the reaction. Cycle threshold (Ct) values were determined using AriaMx Real-time PCR System (Agilent). First, reverse transcription step was done by heating the final reaction mixture to 45 °C for 15 min, then initial denaturation at 95 °C for 120 s, followed by 45 cycles of denaturation at 95 °C for 10 s and annealing/extension at 60 °C for 50 s with the collection of fluorogenic data at the end of this step.
2.4. Virus isolation and propagation
Positive samples, identified by RT-qPCR, were propagated as follows: Vero E6 cells were cultured in T-25 cell culture flasks until cells reached 90% confluency, then the cells were inoculated with 100 ul sample diluted with 300 ul of the inoculation medium containing DMEM supplemented with 2% FBS. The Vero E6 cells were then incubated at 37 °C for 90 min for adsorption. After adsorption, 2.5 mL of the inoculation medium was added, followed by incubation at 37 °C. Virus isolation and propagation were confirmed by RT-qPCR and CPE. A Biosafety Level-3 facility was used for viral culture procedures.
2.5. SARS-CoV-2 inactivation
SARS-CoV2 was treated with beta-propiolactone (βPL) at a final concentration of 1:4000 (0.25% of 10% βPL stock solution) and inactivation was done by incubation at 2–8 °C for 20–24 h.
2.6. Next-generation sequencing and data analysis
Library preparation was done using the AviSeq COV19 NGS Library Prep kit (Ref. AVG202096) and Illumina machine (Iseq-100 instrument) according to manufacture instructions. Complementary DNA (cDNA) was synthesized by adding RT Primer Mix DP (BATCH No.020402C). A multiplex PCR reaction was performed to amplify the entire SARS-Co-V-2 whole genome. The quality of the library were visualized via gel electrophoresis using DNA HS 100 Assay Kit (Cat.No.Q32852).Simple data analysis was performed using Abiomix software for generation FASTA files. Nextclade Tool (version 1.5.2) was also used for viral genome alignment, quality checks and clade assignment.
2.7. TEM of inactivated SARS-CoV-2 delta variant
Inactivated, propagated SARS-CoV2 Delta variant was fixed with 2% Formaldehyde in phosphate buffered saline for 60 min before ultracentrifugation (24,000 rpm, 80 min).The sample was loaded on carbon coating grid stained with 2% Phospho-Tungestic Acid (PTA) for 40 s then examined at 50 nm and 100 nm.
2.8. Statistical analysis
Two-tailed paired t-test was used to compare the difference between the mean scores of the CT values before, and after inoculation. RT-qPCR data represent mean ± standard deviation from three independent experiments. The result is significant at P-value <0.05.
3. Results
3.1. Molecular identification by RT-qPCR
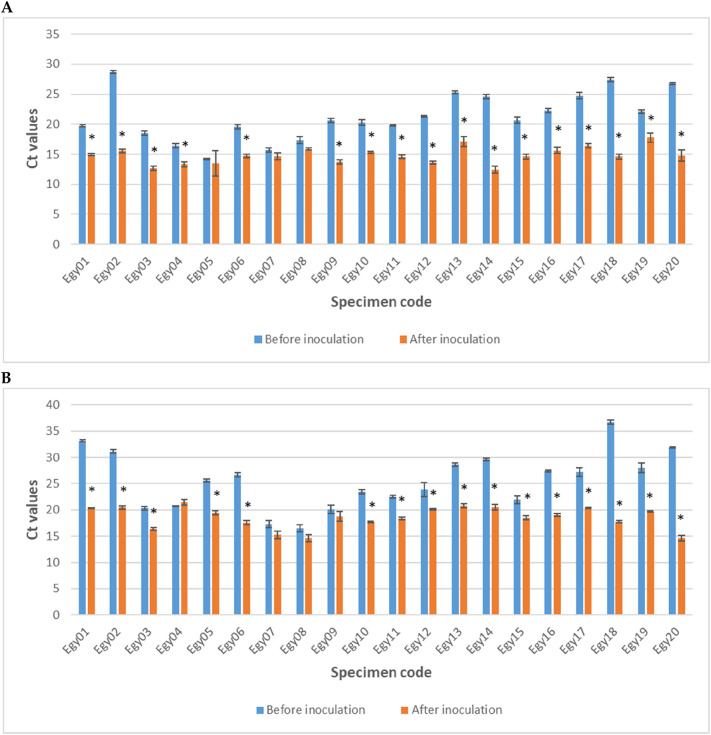
For molecular identification of positive samples, we used a specific RT-qPCR kit. Samples were collected from Egyptian patients suffering from symptoms of SARS-CoV-2 including fever, dyspnea, dry cough, and atypical pneumonia which was confirmed, by chest X-rays. Viasure® SARS-CoV-2 Real Time PCR Detection Kit was used to identify SARS-CoV-2 in the oropharyngeal and nasopharyngeal swabs taken from the patients. The Ct values of the pre and post cell line inoculation was presented in Table 1 . Samples gave positive Ct values ranging from 14.15 to 28.7 for ORF1ab gene ( Fig. 1A ), and from 16.48 to 36.67 for the N gene ( Fig. 1B). The results statistically showing significant difference (P-value <0.05) are labeled with (*) on the graph. The identity, genome sequence and accession code of each isolate was presented in Supplementary data A1.
Table 1.
Ct values for samples before and after inoculation.
| Specimen code | Ct value before inoculation |
Ct value after inoculation |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ORF1 gene | N gene | ORF1 gene | N gene | |||||||||
| EGY01 | 19.87 | 19.50 | 19.77 | 33.14 | 33.30 | 32.90 | 14.80 | 14.98 | 15.05 | 20.41 | 20.33 | 20.21 |
| EGY02 | 28.59 | 29.02 | 28.49 | 30.81 | 31.03 | 31.55 | 15.76 | 15.65 | 15.20 | 20.25 | 20.30 | 20.87 |
| EGY03 | 18.38 | 18.98 | 18.28 | 20.04 | 20.22 | 20.66 | 12.23 | 12.88 | 12.85 | 16.02 | 16.45 | 16.56 |
| EGY04 | 16.40 | 16.04 | 16.70 | 20.60 | 20.84 | 20.68 | 13.78 | 13.00 | 13.22 | 21.98 | 21.21 | 21.07 |
| EGY05 | 14.25 | 14.16 | 14.03 | 25.44 | 25.84 | 25.35 | 12.02 | 12.55 | 15.88 | 19.09 | 19.87 | 19.23 |
| EGY06 | 19.39 | 19.91 | 19.28 | 26.95 | 26.18 | 26.74 | 14.70 | 14.43 | 15.03 | 17.80 | 17.90 | 17.15 |
| EGY07 | 15.87 | 15.29 | 15.92 | 17.83 | 17.51 | 16.50 | 14.22 | 15.31 | 14.45 | 14.38 | 15.71 | 15.66 |
| EGY08 | 16.88 | 17.98 | 17.06 | 15.70 | 16.98 | 16.76 | 15.70 | 15.78 | 16.08 | 14.30 | 14.09 | 15.42 |
| EGY09 | 20.33 | 20.58 | 21.06 | 19.27 | 20.81 | 20.35 | 13.89 | 13.90 | 13.35 | 17.70 | 18.90 | 19.66 |
| EGY10 | 19.78 | 20.36 | 20.74 | 23.02 | 23.46 | 23.76 | 15.55 | 15.22 | 15.16 | 17.60 | 17.55 | 17.81 |
| EGY11 | 19.65 | 19.78 | 19.99 | 22.74 | 22.61 | 22.14 | 14.76 | 14.72 | 14.21 | 18.66 | 18.24 | 18.25 |
| EGY12 | 21.34 | 21.46 | 21.25 | 24.54 | 22.33 | 24.62 | 13.35 | 13.80 | 13.53 | 20.23 | 20.21 | 19.99 |
| EGY13 | 25.54 | 25.26 | 25.08 | 29.02 | 28.46 | 28.38 | 16.21 | 17.87 | 17.28 | 20.76 | 20.32 | 21.09 |
| EGY14 | 24.65 | 24.24 | 24.90 | 29.68 | 29.89 | 29.38 | 12.25 | 12.89 | 12.02 | 20.56 | 20.01 | 20.98 |
| EGY15 | 20.25 | 21.28 | 20.48 | 22.10 | 21.13 | 22.61 | 15.03 | 14.70 | 14.21 | 18.59 | 18.90 | 18.05 |
| EGY16 | 22.15 | 22.03 | 22.68 | 27.53 | 27.24 | 27.41 | 15.90 | 15.98 | 14.98 | 19.30 | 18.90 | 18.85 |
| EGY17 | 24.95 | 25.15 | 24.13 | 27.37 | 27.91 | 26.39 | 16.19 | 16.30 | 16.80 | 20.26 | 20.40 | 20.52 |
| EGY18 | 27.59 | 27.62 | 27.02 | 37.13 | 36.56 | 36.32 | 14.24 | 14.60 | 15.04 | 17.54 | 17.98 | 17.73 |
| EGY19 | 22.02 | 22.40 | 21.90 | 28.98 | 27.25 | 27.66 | 17.77 | 17.03 | 18.56 | 19.69 | 19.53 | 19.90 |
| EGY20 | 26.80 | 26.55 | 26.98 | 31.89 | 31.92 | 31.76 | 14.20 | 15.80 | 14.30 | 14.52 | 15.20 | 14.14 |
Fig. 1.
Molecular identification of SARS-CoV-2 in the specimens and virus propagation as indicated by RT-qPCR. Extracted RNA before inoculation (blue), and after inoculation (red). (A) Ct values of ORF1ab gene amplification. (B) Ct values of N gene amplification. Data represent mean ± standard deviation from three independent experiments. * The result is significant at P-value <0.05. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2. Virus propagation on VeroE6 cells
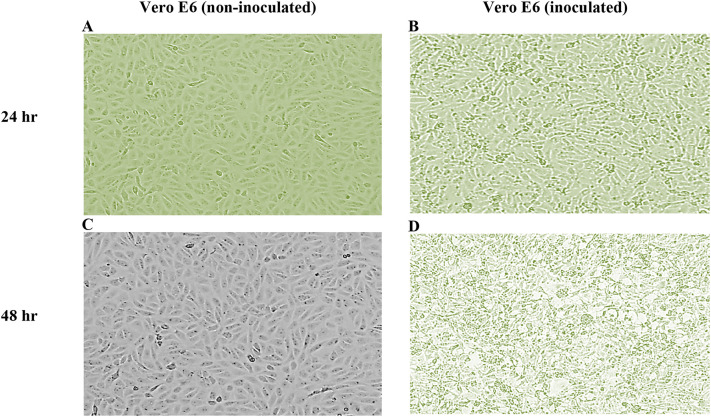
PCR positive samples were grown in Vero E6 cells. Virus replication was first investigated by daily monitoring of CPE in the inoculated Vero E6 cells for 2 days. We observed CPE in the inoculated cells beginning from day 1 post-inoculation and recorded after 48 h post-inoculation ( Fig. 2 ). To identify the propagation of the virus as SARS-CoV-2, RT-qPCR was used.
Fig. 2.
Virus propagation in Vero E6 cells. Positive samples were inoculated onto Vero E6 cells. The cells were monitored daily for 2 days and CPE in the inoculated cells with respect to the control (non-inoculated) cells was recorded. (A) Vero E6 (non-inoculated) after 24 h. (B) Vero E6 24 h post-inoculation. (C) Vero E6 (non-inoculated) after 48 h. (D) Vero E6 48 h post-inoculation.
The presence of SARS-CoV-2 in the propagated samples was confirmed, and Ct values for ORF1ab and N genes in the the propagated samples was confirmed, and Ct values for ORF1ab and N genes in the propagated samples markedly decreased compared to the corresponding values in the samples before inoculation, where Ct values ranged from 12.39 to 17.79 forORF1ab gene, and from 14.6 to 21.42 for the N gene, after inoculation RT-qPCR data show that, after inoculation, Ct values for ORF1ab and N genes amplification markedly decreased compared to the corresponding values in the samples before inoculation ( Table 1 and Fig. 1 A,B). This finding confirms the propagation of SARS-CoV-2.
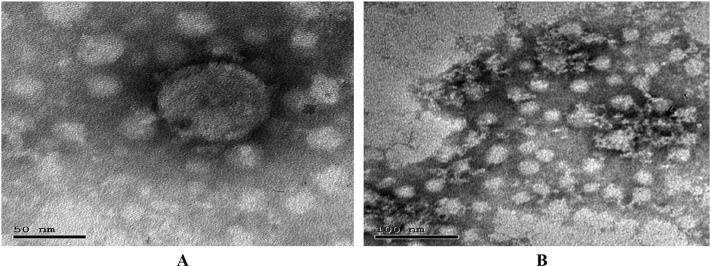
3.3. Viral Inactivation with β-propiolactone
The inactivation curves for viruses following exposure to β-Propiolactone (βPL) were not linear and showed “tailing” or a decrease in inactivation rate after βPL treatment. This was attributed to a drop in βPL concentration over time induced by the agent's contact with the virus, water, or medium components, which slowed the rate of inactivation. In a semi-logarithmic plot of virus titer vs inactivation time, chemical inactivation resulted in nonlinear tailing curves, indicating non-first-order kinetics with regard to virus titer, as shown in Fig. 3 .
Fig. 3.
Viral inactivation curve.
3.4. Test for effective inactivation
The virus was inoculated onto VeroE6 for three passages and there was no cytopathic effect (CPE) observed after 48 h post infection with propagated virus.
3.5. Next-generation sequencing and data analysis
After a complete molecular identification of the propagated SARS-CoV2 with RT-qPCR, the full genome of the propagated virus from all samples was sequenced. Whole Genome sequencing alignment was performed by BWA software and the output showed 20 successful high-quality genomes. These sequences were compared with the entire genome of reference SARS-CoV-2 (NC_045512.2). The validated sequences (n = 20) were submitted to NCBI Virus GenBank (Accession codes: MT776904, MT798592, MT897260, MT905421, MT905422, MT905430, MT947079, MT947084, MT947153, MT994951, MT994965, MT994970, MT994978, MT994981, MT994987, MT994988, MW010028 and MW010029) and to GISAID (Accession codes: EPI_ISL_4748272 and EPI_ISL_4748283). (See Supplementary data A1 for the identity, genome sequence and accession code of each isolate).
Further analysis was performed to detect the genetic mutation using Nextclade Tool (https://clades.nextstrain.org/). All isolates recovered in 2020 (n = 18) were clade 20A and showed nine substitutions, in a nucleotide sequences compared with the reference strain NC_045512.2, including C241T, C3037T, C14362T, G15907A, T17091C, A23403G, G25563T, G26257T and A29871G. While, the isolates recovered in 2021 (n = 2) were clade 21J (Delta) (Fig. 4 ) and showed 41 nucleotide substitutions. The isolates released in 2020 were similar and showed four viral genome mutations in ORF1b, ORF3a, S and E. However, the isolates released in 2021 showed 32 viral genome mutations in ORF1a, ORF1b, ORF3a, ORF6, ORF7a, ORF7b, ORF8, S, E, M, and N as shown in Table 2 .
Fig. 4.

Unrooted phylogenetic tree showing the distribution of Delta SARS-CoV-2 sequences. Constructed by open access tool (https://clades.nextstrain.org/).
Table 2.
Viral genome mutations in SARS-CoV-2 recovered isolates.
| Isolates recovered in 2020 (n = 18) | Isolates recovered in 2021 (n = 2) Delta (B.1.617.2) variant |
||||
|---|---|---|---|---|---|
| S:D614G ORF1b:G814S ORF3a:Q57H E:V5F |
ORF1a:A1306S ORF1a:L1507F ORF1a:P2046L ORF1a:P2287S ORF1a:T2836I ORF1a:V2930L ORF1a:T3255I |
ORF1a:T3646A ORF1a:V3660M ORF1a:D4190E ORF1a:T4175I S:T19R S:T95I S:L452R |
S:T478K S:D614G S:P681R S:D950N ORF1b:P314L ORF1b:A572 |
ORF1b:G662 ORF1b:P1000 ORF1b:A1918 ORF1b:S2312L N:D63G N:R203M |
N:G215C N:D377Y ORF3a:S26L ORF7a:T120I ORF7b:T40I ORF9b:T60A |
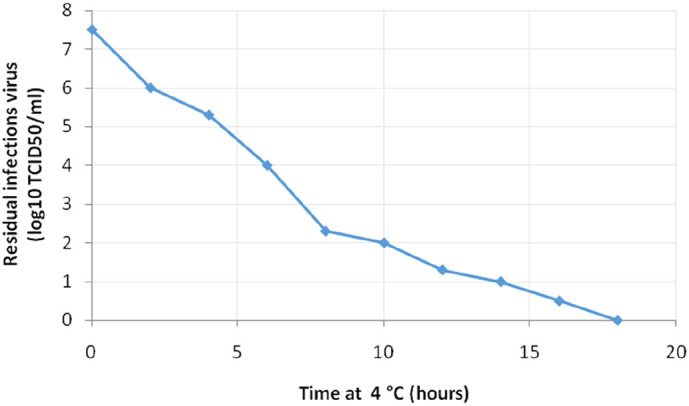
Characterization of isolates recovered in September 2021 revealed that EPI_ISL_4748272 and EPI_ISL_4748283 variants were AY.119.2 and AY.44 Pango Lineage, respectively. Both of them were Delta (B.1.617.2) variants. Further characterization of the isolated Delta variant was performed by transmission electron microscopy (TEM). Electron micrograph was revealed that there were oval viral particles with spikes measuring approximately 100 nm in diameter, as described in Fig. 5 .
Fig. 5.
Inactivated SARS-CoV-2 Delta variant particle observed by transmission electron microscopy (TEM). (A) Electron micrograph (50 nm). (B) Electron micrograph (100 nm).
4. Discussion
The coronavirus SARS-CoV-2 is an ssRNA virus that has spread worldwide (Ahmadi et al., 2020). The continuous emergence of coronaviruses and the recent pandemic of the novel coronavirus (SARS-CoV-2) threaten public health and the world economy. This necessitates a continuous follow-up of its evolution and the detection of the genomic variations that spread globally (Cascella et al., 2022). Moreover, there is an urgent need to check the efficacy of the applied treatment protocol as well as the effectiveness of the current vaccines against the novel SARS-CoV-2 variants (Garcia-Beltran et al., 2021). In order to achieve that we must establish a simple method for isolation and propagation of SARS-CoV-2 that achieve a high titer of virus with minimal or no effect on the viral genome.
In the current study, we set a simple method for the isolation and propagation of SARS-CoV-2 isolated from Egypt. After specimen collection from Egyptian patients, we used a simple transfer medium that essentially has the same composition as the inoculation medium used in the propagation process plus antibiotics, to avoid inactivation of the infectious SARS-CoV-2 particles during transportation. Different RT-PCR protocols were designed to amplify variable SARS-CoV-2 genes, such as RdRp, E, N, S, and ORF1a/b genes (Cui and Zhou, 2020; Bai et al., 2020). Of note, ORF1ab and N genes are commonly used for COVID-19 determination in China, while N1, N2 and N3 genes are targeted in US CDC (Bai et al., 2020; Sheikhzadeh et al., 2020). For molecular identification of SARS-CoV-2 in the collected specimens, we used Viasure® SARS-CoV-2 Real Time PCR Detection Kit which targets ORF1ab and N genes for amplification. Our findings revealed that the applied rRT-PCR protocol is effective as an accurate and precise molecular diagnostic test for confirming COVID-19 infection.
Propagation of SARS-CoV-2 in cell culture is crucial for various studies. In the current study, we used Vero E6 cells to propagate SARS-CoV-2 from the clinical specimens. Although DMEM supplemented with 10% FBS was used to maintain Vero E6 cells, the inoculation medium was supplemented with 2% FBS instead, which is preferred for virus propagation (TaŞtan et al., 2020; Saad et al., 2021). Our observations are consistent with previous studies which reported that the African Green Monkey cell lines, such as Vero E6 and Vero CCL-81, showed great effectiveness in growing SARS-CoV-2 (Harcourt et al., 2020; Case et al., 2020; Saad et al., 2021; Calderaro et al., 2020). Moreover, it has been reported that, in comparison with Vero CCL-81 cell line, Vero E6 cell line is better, not only in SARS-CoV-2 amplification but also in quantification by plaque assay (Harcourt et al., 2020).
Virus replication was investigated by monitoring CPE in the inoculated Vero E6 cells. We observed CPE beginning from day 1 post-inoculation, which became more prominent at 48 h post-inoculation. In agreement with our findings, a previous study reported that CPE was nearly complete in Vero E6 at 48 h post-infection with SARS-CoV-2 (Jureka et al., 2020), while Case et al. reported that the CPE appears in Vero cells by day 3 post-inoculation (Case et al., 2020). Furthermore, we used the same RT-qPCR kit employed to identify SARS-CoV-2 in the original swabs to identify the propagation of SARS-CoV-2 virus. We found that Ct values for ORF1ab and N genes in the propagated samples markedly decreased compared to the corresponding values in the original swabs before inoculation. Taken together, CPE and RT-qPCR findings confirm successful propagation of SARS-CoV-2. Of note, we did not conduct sequential propagation of virus in Vero E6, which has been demonstrated to cause rapid development of genetic variants (Funnell et al., 2021; Ogando et al., 2020).
In the present study, the full genome of the virus propagated in cell culture was sequenced and submitted to NCBI (n = 18) in 2020 and to GISAID (n = 2) in 2021. Our findings regarding the whole genome sequencing of SARS-CoV-2 recovered in 2020 showed that all strains belong to the 20A clade and were mutated and carried D614G, V5F, Q57H and G823S mutations. In agreement with this finding, several studies conducted to track the distribution of viral clades in Egypt reported the higher prevalence of all clades with D614G mutation in 2020 (Hamed et al., 2021; Alotaibi et al., 2022; Zekri et al., 2021; Kandeil et al., 2020). Two isolates were recovered from COVID-19 patients, in September 2021, (accession codes: EPI_ISL_4748272 and EPI_ISL_4748283) were AY.119.2 and AY.44 Pango Lineage, respectively. Both of them were delta (B.1.617.2) variants. They were related to variant of concern (VOC) Delta GK/478 K.V1 (B.1.617.2) first discovered in India. The first official case of the delta variant was recorded in Egypt in July 2021 (Enterprise, 2021). The recovered Delta variants carried several amino acid mutations in spike protein including D614G, D950N, L452R, P681R, T19, T95I and T478K. The spike protein mutations (T478K, P681R and L452R) have a significant impact on SARS-CoV-2 transmissibility and its neutralization by antibodies for earlier variants (Starr et al., 2021).
The delta variant (B.1.617.2) is characterized by easily and quickly spreading than other variants, resulting in increased number of COVID-19 cases (Ramesh et al., 2021; Singanayagam et al., 2022). The transmission rate of delta variants is 50% higher than the alpha variant (Dhar et al., 2021). The delta variant (B.1.617.2) also associated to high level of hospitalization as well as emergency care attendance (Butt et al., 2022; Twohig et al., 2022). Vaccination, on the other hand, is quite effective in lowering the severity of COVID-19 and preventing death, but it is less effective in preventing infection by the delta and alpha variants (Ramesh et al., 2021; Singanayagam et al., 2022; Lopez Bernal et al., 2021). Bates et al. also reported that the novel SARS-CoV-2 variants are resistant to serum antibody inactivation, implying lower protection against re-infection or a higher likelihood of vaccine failure (Bates et al., 2021).
5. Conclusion
In conclusion, the stability of the viral genome was our greatest concern to avoid any possible variations that could result from viral propagation. This study provides a reference for researchers in Egypt to isolate and propagate SARS-CoV-2 easily and efficiently. The established protocol of isolation, propagation, and inactivation was utilized in order to perform further molecular characterization studies such as whole genome sequencing (WGS) and morphological analysis of SARS-CoV-2 by transmission electron microscopy. The phylogenetic analysis of isolated SARS-CoV-2 in Egypt showed that the virus has exhibited a dramatic evolution since the first case registered in Egypt. The isolates recovered in 2020 were similar to the reference strain, Wuhan-Hu-1. The two recovered isolates in 2021 have been clustered into the 21J subclade. These variants are the first isolates with the Delta (B.1.617.2) variant ever recorded in Egypt. This study will help researchers with their ongoing SARS-CoV-2 vaccine research, evolutionary studies, and the development of antiviral drugs.
Data availability statement
Data are available upon request from the corresponding author.
Institutional review board statement
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the declaration of Helsinki, and the protocol was approved by Princess Nourah Bint Abdulrahman, PNU Institutional Review Board (IRB Registration Number with KACST, KSA: H-01-R-059 and IRB Log Number: 20-0457 in 2020) and the Research Ethics Committee of Faculty of Pharmacy, Tanta University. Samples collection was performed after permission from the head of the Army Hospital.
Informed consent statement
The purpose of the study was explained to the patients and informed consents were obtained according to the guidelines on human research adopted by the Research Ethics Committee at the Faculty of Pharmacy, Tanta University.
CRediT authorship contribution statement
Badriyah Alotaibi: Conceptualization, Funding acquisition, Project administration. Thanaa A. El-Masry: Conceptualization, Funding acquisition, Resources, Visualization, Writing – review & editing. Mohamed G. Seadawy: Data curation, Formal analysis, Methodology, Writing – original draft. Bassem E. El-Harty: Data curation, Formal analysis, Methodology. Asmaa Saleh: Investigation, Writing – original draft. Ahmed F. Gad: Data curation, Formal analysis, Methodology. Mostafa F. El-Hosseny: Data curation, Formal analysis, Methodology. Yasmen F. Mahran: Formal analysis, Writing – review & editing. Maisra M. El-Bouseary: Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
The authors extend their appreciation to the Deputyship for Research & Innovation, Ministry of Education in Saudi Arabia for funding this research work through the project number (PNU-DRI-Targeted-20-(032).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.meegid.2022.105278.
Appendix A. Supplementary data
Supplementary A1: List of the identity, genome sequence and accession code of each isolate (n = 20).
References
- Ahmadi E., Zabihi M.R., Hosseinzadeh R., Noorbakhsh F. SARS-CoV2 spike protein displays biologically significant similarities with paramyxovirus surface proteins; a bioinformatics study. bioRxiv. 2020 doi: 10.1101/2020.07.20.210534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alotaibi B., El-Masry T.A., Seadawy M.G., Farghali M.H., El-Harty B.E., Saleh A., et al. SARS-CoV-2 in Egypt: epidemiology, clinical characterization and bioinformatics analysis. Heliyon. 2022;8(2) doi: 10.1016/j.heliyon.2022.e08864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai H., Cai X., Zhang X. Landscape coronavirus disease 2019 test (COVID-19 test) in vitro- A comparison of PCR vs immunoassay vs CRISPR-based test.OSF. Preprints. 2020 doi: 10.31219/osf.io/6eagn. [DOI] [Google Scholar]
- Bates T.A., Leier H.C., Lyski Z.L., McBride S.K., Coulter F.J., Weinstein J.B., et al. Neutralization of SARS-CoV-2 variants by convalescent and BNT162b2 vaccinated serum. Nat. Commun. 2021;12(1):5135. doi: 10.1038/s41467-021-25479-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brian D.A., Baric R.S. Coronavirus genome structure and replication. Curr. Top. Microbiol. Immunol. 2005;287:1–30. doi: 10.1007/3-540-26765-4_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt A.A., Dargham S.R., Chemaitelly H., Al Khal A., Tang P., Hasan M.R., et al. Severity of illness in persons infected with the SARS-CoV-2 delta variant vs beta variant in Qatar. JAMA Intern. Med. 2022;182(2):197–205. doi: 10.1001/jamainternmed.2021.7949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderaro A., Arcangeletti M.C., De Conto F., Buttrini M., Montagna P., Montecchini S., et al. SARS-COV-2 infection diagnosed only by cell culture isolation before the local outbreak in an Italian seven-week-old suckling baby. Int. J. Inf. Dise. 2020;96:386–389. doi: 10.1016/j.ijid.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella M., Rajnik M., Aleem A., Dulebohn S.C., Di Napoli R. 2022. Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls [Internet]. Updated 2022 5 Jan. [PubMed] [Google Scholar]
- Case J.B., Bailey A.L., Kim A.S., Chen R.E., Diamond M.S. Growth, detection, quantification, and inactivation of SARS-CoV-2. Virology. 2020;548:39–48. doi: 10.1016/j.virol.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman V.M., Muth D., Niemeyer D., Drosten C. Hosts and sources of endemic human coronaviruses. Adv. Virus Res. 2018;100:163–188. doi: 10.1016/bs.aivir.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui F., Zhou H.S. Diagnostic methods, and potential portable biosensors for coronavirus disease 2019. Biosens. Bioelectron. 2020;165 doi: 10.1016/j.bios.2020.112349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J., Li F., Shi Z.L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wit E., Van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14(8):523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhar M.S., Marwal R., Vs R., Ponnusamy K., Jolly B., Bhoyar R.C., et al. Genomic characterization and epidemiology of an emerging SARS-CoV-2 variant in Delhi, India. Science. 2021;374(6570):995–999. doi: 10.1126/science.abj9932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enterprise Delta variant has landed + vaccine passes might become a thing in Egypt. Monday. https://enterprise.press/stories/2021/08/23/delta-variant-has-landed-vaccine-passes-might-become-a-thing-in-egypt-51303/
- Funnell S.G.P., Afrough B., Baczenas J.J., Berry N., Bewley K.R., Bradford R., et al. A cautionary perspective regarding the isolation and serial propagation of SARS-CoV-2 in Vero cells. npj Vaccines. 2021;6(1):83. doi: 10.1038/s41541-021-00346-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Beltran W.F., Lam E.C., St Denis K., Nitido A.D., Garcia Z.H., Hauser B.M., et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell. 2021;184(9):2372–2383.e9. doi: 10.1016/j.cell.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamed S.M., Elkhatib W.F., Khairalla A.S., Noreddin A.M. Global dynamics of SARS-CoV-2 clades and their relation to COVID-19 epidemiology [Sci rep] Sci. Rep. 2021;11(1):8435. doi: 10.1038/s41598-021-87713-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt J., Tamin A., Lu X., Kamili S., Sakthivel S.K., Murray J., et al. Isolation and characterization of SARS-CoV-2 from the first US COVID-19 patient [Preprint] bioRxiv. 2020 doi: 10.1101/2020.03.02.972935. [DOI] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., et al. First Case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jureka A.S., Silvas J.A., Basler C.F. Propagation, inactivation, and safety testing of SARS-CoV-2. Viruses. 2020;12(6):622. doi: 10.3390/v12060622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandeil A., Mostafa A., El-Shesheny R., Shehata M., Roshdy W.H., Ahmed S.S., et al. Coding-complete genome sequences of two SARS-CoV-2 isolates from Egypt. Microbiol Resour Announc. 2020;9(22) doi: 10.1128/MRA.00489-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.M., Chung Y.S., Jo H.J., Lee N.J., Kim M.S., Woo S.H., et al. Identification of coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect. 2020;11(1):3–7. doi: 10.24171/j.phrp.2020.11.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez Bernal J., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., et al. Effectiveness of COVID-19 vaccines against the B.1.617.2 (Delta) variant. N. Engl. J. Med. 2021;385(7):585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medhat M.A., El Kassas M. COVID-19 in Egypt: uncovered figures or a different situation? J. Glob. Health. 2020;10(1) doi: 10.7189/jogh.10.010368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monchatre-Leroy E., Boué F., Boucher J.M., Renault C., Moutou F., Ar Gouilh M., Umhang G. Identification of alpha and beta coronavirus in wildlife species in France: Bats, Rodents, Rabbits, and Hedgehogs. Viruses. 2017;9(12):9. doi: 10.3390/v9120364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogando N.S., Dalebout T.J., Zevenhoven-Dobbe J.C., Limpens R.W.A.L., van der Meer Y., Caly L., et al. SARS-coronavirus-2 replication in Vero E6 cells: replication kinetics, rapid adaptation and cytopathology. J. Gen. Virol. 2020;101(9):925–940. doi: 10.1099/jgv.0.001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramesh S., Govindarajulu M., Parise R.S., Neel L., Shankar T., Patel S., et al. Emerging SARS-CoV-2 variants: a review of its mutations, its implications and vaccine efficacy. Vaccines. 2021;9(10):1195. doi: 10.3390/vaccines9101195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saad M.A., Saleh A.A., Ryan I., Amin M., Saleh M.S., Abdulaal T., et al. Preliminary step towards COVID-19 inactivated vaccine development in Egypt. Arch. Clin. Trials. 2021;1(1):1–6. doi: 10.33425/2768-4598.1001. [DOI] [Google Scholar]
- Seadawy M.G., Gad A.F., Abo-Elmaaty S.A., Hassan M.G. Genome sequencing of SARS-CoV-2 reveals the prevalence of variant B.1.1.7 in Egypt. Infect. Genet. Evol. 2022;97:105191. doi: 10.1016/j.meegid.2021.105191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikhzadeh E., Eissa S., Ismail A., Zourob M. Diagnostic techniques for COVID-19 and new developments. Talanta. 2020;220 doi: 10.1016/j.talanta.2020.121392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singanayagam A., Hakki S., Dunning J., Madon K.J., Crone M.A., Koycheva A., et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect. Dis. 2022;22(2):183–195. doi: 10.1016/S1473-3099(21)00648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr T.N., Greaney A.J., Dingens A.S., Bloom J.D. Complete map of SARS-CoV-2 RBD mutations that escape the monoclonal antibody LY-CoV555 and its cocktail with LY-CoV016. Cell Rep. Med. 2021;2(4) doi: 10.1016/j.xcrm.2021.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TaŞtan C., Yurtsever B., Sir KarakuŞ G., Dİlek KanÇaĞi D., Demİr S., Abanuz S., et al. SARS-CoV-2 isolation and propagation from Turkish COVID-19 patients. Turk J. Biol. 2020;44(3):192–202. doi: 10.3906/biy-2004-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twohig K.A., Nyberg T., Zaidi A., Thelwall S., Sinnathamby M.A., Aliabadi S., et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect. Dis. 2022;22(1):35–42. doi: 10.1016/S1473-3099(21)00475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dorp L., Acman M., Richard D., Shaw L.P., Ford C.E., Ormond L., et al. Emergence of genomic diversity and recurrent mutations in SARS-CoV-2. Infect. Genet. Evol. 2020;83 doi: 10.1016/j.meegid.2020.104351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M.Y., Zhao R., Gao L.J., Gao X.F., Wang D.P., Cao J.M. SARS-CoV-2: structure, biology, and structure-based therapeutics development. Front. Cell. Infect. Microbiol. 2020;10 doi: 10.3389/fcimb.2020.587269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization WHO coronavirus [COVID-19] dashboard. 2022. https://covid19.who.int/ on March 23rd.
- World Health Organization Egypt: WHO. Coronavirus disease [COVID-19] dashboard. 2022. https://covid19.who.int/region/emro/country/eg on March 23rd.
- Zekri A.N., Easa Amer K.E., Hafez M.M., Hassan Z.K., Ahmed O.S., Soliman H.K., et al. Genomic characterization of SARS-CoV-2 in Egypt. J. Adv. Res. 2021;30:123–132. doi: 10.1016/j.jare.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary A1: List of the identity, genome sequence and accession code of each isolate (n = 20).
Data Availability Statement
Data are available upon request from the corresponding author.