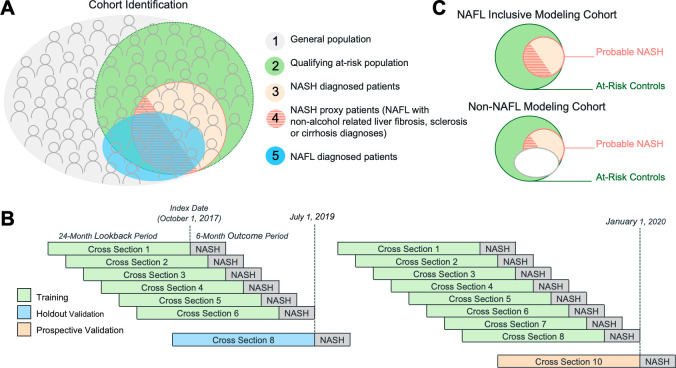
Figure 1.
Cohort selection and model development. (A) Patients were identified from the general population (1) who met study stratification criteria (2). A subset of eligible patients was classified as likely to have NASH as evidenced by either a NASH diagnosis within 6 months after model prediction (3) or a diagnosis for non-alcohol-related liver fibrosis, sclerosis or cirrhosis within 6 months after model prediction and in proximity to a NAFL diagnosis (4). Eligible patients with no evidence of NASH were used as adversarial training examples, that is, patients with an overlap in symptoms, treatments and timing of resource utilisation but who were not patients with NASH. Patients with an existing NAFL claim in the previous 24 months overlapped with the patients with probable NASH population (5). Multiple time-bound cross-section were derived from the at-risk patient population (B). Cross-section 8 was reserved as a holdout set for model validation since it was sufficiently offset to prevent temporal overlap with the training set outcome window. Simulated model deployment using a prospective validation (scoring) set was performed by training on cross-sections 1–6 or on cross-sections 1–8 and using cross-section 10 as the test set. The NAFL inclusive and non-NAFL modelling cohorts used for model development (C). NAFL, non-alcoholic fatty liver; NASH, non-alcoholic steatohepatitis.