Abstract
We report a case of localized malignant pleural mesothelioma (LMPM) of the interlobar fissure mimicking lung cancer. A 74-year-old woman presented with dyspnoea and a left pleural effusion. Chest computed tomography revealed a bulky mass, arising from the left lower lobe with intense uptake at the 18F-FDG PET. A left lower lobectomy was performed after thoracoscopic pleural biopsies. The final histology revealed an LMPM epithelioid like. We describe the diagnostic and curative path of the disease, speculating on the differential diagnosis and treatment of LMPM.
Keywords: Mesothelioma, Lung cancer, Epithelioid like
A 74-year-old woman without a history of asbestos exposure, presented with dyspnoea, left pleural effusion and a CA-125 level of 357 IU/ml (normal <35).
CASE
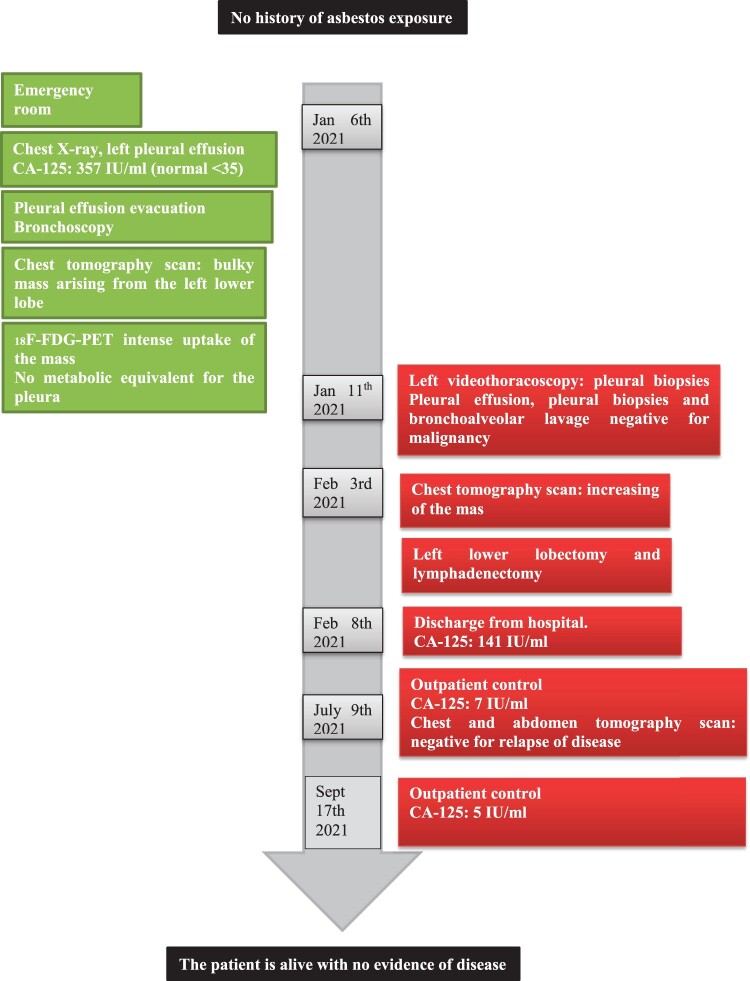
A 74-year-old woman without a history of asbestos exposure, presented with dyspnoea, left pleural effusion and a CA-125 level of 357 IU/ml (normal <35). After partial evacuation of the pleural effusion, the chest computed tomography showed a bulky mass, arising from the lower lobe (Fig. 1A). The 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) documented intense uptake of the mass with a residual layer of pleural effusion with no metabolic equivalent (Fig. 1B). We performed thoracoscopic biopsies of hyperaemic pleura and, in another session, a left lower lobectomy. Surgery revealed a sessile mass, arising from the lower lobe, firmly adherent to the interlobar fissure. The final diagnosis was localized malignant pleural mesothelioma (LMPM) epithelioid like. The postoperative course was uneventful. The CA-125 level dropped to 141 IU/ml before discharge and to 7 IU/ml at 6 months. At a 9-month follow-up, she is alive and well (Fig. 2).
Figure 1:
(A) Chest computed tomography (CT) scan image of the mass; (B) 18F-FDG PET, showing intense uptake of the mass; (C) sheets and tubular structures of epithelioid cells associated with marked lymphocytic and plasmacellular infiltrate; and (D) neoplastic cells immunoreactive for calretinin.
Figure 2:
Timeline.
Pleural effusion cytology and pleural biopsies were negative for malignancy. A frozen section on the mass biopsy showed the presence of malignant cells suggestive of epithelial origin. The greyish mass was 9 cm × 8 cm × 7 cm. Histology of formalin-fixed paraffin-embedded tissue sections showed polygonal epithelioid cells with prominent nucleoli and eosinophilic cytoplasm arranged in tubular-papillary structures and solid nests with prominent intra- and peritumoural inflammatory infiltrate. The neoplasm infiltrated the visceral pleura without evidence of lung invasion, separated from lung parenchyma by a fibrous capsule (Fig. 1C). Resection margins and lymph nodes were negative. Immunohistochemistry revealed, among the others, a strong reactivity of neoplastic cells for calretinin (Fig. 1D), high molecular weights cytokeratin 5 and 7 and focal positivity for Wilms tumour 1.
DISCUSSION
LMPM is a rare subtype of malignant pleural mesothelioma (MPM). It is diagnosed as a solitary serosal lesion without evidence of diffuse surface involvement and a microscopic pattern identical to that of diffuse malignant mesothelioma (DMM) [1–3]. Macroscopically, LMPM can be pulmonary, extrapulmonary, lobulated and/or a smooth mass with or without ribs infiltration. There are too few cases to determine if long-term survival in LMPM is better than DMM and if it correlates with the histologic subtype [2, 4]. The prognosis seems more favourable and it is potentially curable by radical surgical excision [2].
Compared to DMM, a history of asbestos exposure is less frequent [1, 2]. Differential diagnoses include primary pulmonary neoplasm, metastases and other mesenchymal pleural tumours such as synovial sarcoma and solitary fibrous tumours. Diagnosis is generally postoperative and based on radiological, surgical and pathological evaluation. Preoperative diagnosis by percutaneous CT-guided biopsy might not offer a reliable diagnosis [5]. We decided to perform thoracoscopic pleural biopsies first, waiting for the final pathology, considering the difficulties of differential diagnosis between metastatic lung cancer and pleural mesothelioma. Lobectomy was performed in another session following intraoperative frozen section on a biopsy of the mass. The TTF-1 negativity, strong reactivity for calretinin, and focally for WT-1, confirmed the mesothelial origin of the neoplasm. Morphology and immunohistochemistry ruled out mesenchymal tumours.
After radical surgery, the literature suggests a longer survival of LMPM compared to DDM; however, the disease progression is difficult to predict [1, 2, 4]. The epithelioid histological type is considered to be a positive prognostic indicator over the sarcomatoid or biphasic type in the DMM. Nevertheless, several studies do not confirm this hypothesis [3, 4].
There are no accepted tumour markers in routine clinical practice for mesothelioma [5]. The baseline level of serum CA-125 is considered as an independent prognostic factor for patients with DMM increasing with the progression of the disease. Its monitoring could suggest the advisability of adjuvant therapy [5]. Our patient showed a drastic decrease in the CA-125 level after surgery. Its dosage was included in the follow-up routine.
LMPM may resemble solitary lung cancer as this case shows. The diagnostic-therapeutic process, albeit articulated, proved to be correct for this complicated case. It would have been advisable, at the time of the pleural biopsies, to perform a biopsy of the primary tumour.
Conflict of interest: none declared.
Data Availability Statement
All relevant data are available without limitation from the authors.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Pietro Bertoglio, Giovanni Luca Carboni and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
REFERENCES
- 1. Allen TC, Cagle PT, Churg AM, Colby TV, Gibbs AR, Hammar SP. et al. Localized malignant mesothelioma. Am J Surg Pathol 2005;29:866–73. [DOI] [PubMed] [Google Scholar]
- 2. Marchevsky AM, Khoor A, Walts AE, Nicholson AG, Zhang YZ, Roggli V. et al. Localized malignant mesothelioma, an unusual and poorly characterized neoplasm of serosal origin: best current evidence from the literature and the International Mesothelioma Panel. Mod Pathol 2020;33:281–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brcic L, Kern I.. Clinical significance of histologic subtyping of malignant pleural mesothelioma. Transl Lung Cancer Res 2020;9:924–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guo X, Watanabe J, Takahashi K, Hayashi T, Kurose N, Sasaguri Y. et al. Localized malignant pleural mesothelioma arising in the interlobar fissure: a unique surgical case masquerading clinicopathologically as primary lung adenocarcinoma. SAGE Open Med Case Rep 2019;7:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cheng X, Gou H, Liu J, Luo D, Qiu M.. Clinical significance of serum CA125 in diffuse malignant mesothelioma. SpringerPlus 2016;5:368. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are available without limitation from the authors.