Abstract
Intraoperative injuries to the ureter can occur in complicated colorectal and gynaecologic procedures in minimal access surgery. The majority of these go unrecognised at the time of the operation, which can be disastrous to the patient. The routine use of ureteric stents is controversial, with some studies showing that stents only enable detection of ureteric injury but do not prevent it. Fluorescent image-guided surgery with indocyanine green (ICG) to visualise the ureter is a relatively new technique. We report our method of visualisation of the ureter in two patients undergoing laparoscopic anterior resection and Hartmann procedure, respectively. After induction of anaesthesia, retrograde catheterisation of both ureters was performed by the urologist. 2.5 mg ICG was injected into each catheter at the start of the procedure. Both ureters were visualised very well throughout the procedure with no post-operative complications. This technique using ICG adds visual cues to make up for the loss of tactile feedback, making it a safe strategy to prevent intraoperative ureteric injury.
Keywords: Colorectal surgery, fluorescent imaging, indocyanine green, laparoscopy, ureter, ureteric injury
INTRODUCTION
Laparoscopic colorectal procedures are advanced and require a high level of technical skill. The benefits of laparoscopic surgery are well known in terms of reduced post-operative pain, earlier recovery, decreased incisional hernias and cosmesis.[1] As there is a significant reduction of tactile feedback, intraoperative injuries to adjacent structures sometimes go unnoticed. Iatrogenic ureteric injuries are one such complication, which, if detected late, can be disastrous for the patient.[2,3,4] Prophylactic ureteral stents do help in detecting intraoperative ureteral injury but do not prevent it.[5] Furthermore, prophylactic stent insertion has its complications, which makes its routine use debatable. It would be desirable to visualise the ureters during the surgical procedure, which would make up for the lack of tactile feedback in laparoscopic surgery. Fluorescence ureterography has been studied only by a few investigators using methylene blue dye or indocyanine green (ICG).[6,7,8,9,10] This can provide real-time mapping of the ureter, which facilitates focussed dissection to prevent ureteral injury. We present here our method of fluorescent visualisation of ureters in colorectal surgery.
CASE REPORTS
Case 1
A 50-year-old female was referred to our hospital because of altered bowel habits and urgency to defecate for the past 2 months. Her magnetic resonance imaging of the pelvis showed a 4.7 cm × 1.4 cm growth in the distal third of the rectum 3.6 cm from the anal verge with multiple pararectal nodes suggestive of Stage 3c carcinoma rectum (cT3aN1M0). After receiving short-course radiotherapy of 25 Gy in 5 fractions to the pelvis, she was taken up for surgery. In the operating room, after induction of general anaesthesia, rigid cystoscopy and retrograde bilateral ureteric catheterisation were performed by the urologist. 2.5 mg (1 ml) of ICG dye was diluted with 4 ml distilled water and injected into each catheter before starting the surgery. A laparoscopic ultralow anterior resection with colo-anal stapled anastomosis and covering loop ileostomy was performed. Near-infrared (NIR) visualisation was performed with the Spies™ system (Karl-Storz®). Both ureters were visualised well throughout the surgery [Figures 1 and 2]. The ureteral catheters were removed at the end of the surgical procedure. Post-operatively, the patient had haematuria for 2 days which settled without the need for blood transfusion. Recovery was uneventful with ileostomy functioning well on day 2. The patient was discharged on day 6 with no fever or urinary disturbances.
Figure 1.
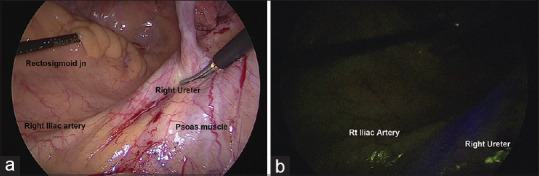
(a) Intraoperative view white light mode at the start of dissection showing right Iliac artery and right ureter, (b) near-infrared mode
Figure 2.
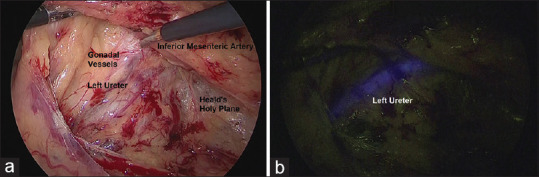
(a) Intraoperative view during medial to lateral dissection. The inferior mesenteric artery has been lifted with the left-handed grasper. The left ureter along with gonadal vessels is just visible, (b) same image near-infrared mode
Case 2
This patient, a 38-year-old male, presented with complaints of the passage of mucoid stools, increasing in frequency for the past 2 months. A digital rectal examination and proctoscopy were done at the outpatient clinic and were normal. Computed tomography of the abdomen and pelvis showed an ulceroproliferative growth of about 9.2 cm × 6 cm involving the upper rectum and rectosigmoid junction with suspicious infiltration of the sigmoid mesocolon. He was posted for surgery. After pre-operative retrograde ureteric catheterisation by the urologist, 2.5 mg of ICG was injected into each catheter. Laparoscopic Hartmann procedure was performed because of bulky growth causing difficulty in pelvic dissection. NIR visualisation was performed with the Spies™ system (Karl-Storz®). ICG was particularly useful in this patient as the sigmoid mesocolon was closely adherent to the ureter. This part of the dissection was done under NIR guidance [Figures 3 and 4]. The patient underwent laparotomy and refashioning of the stoma on the 3rd day due to necrosis of the stoma. 100 cc collection was also drained, but there was no ureteric injury at the operation. This patient recovered well and was discharged with no further complaints.
Figure 3.
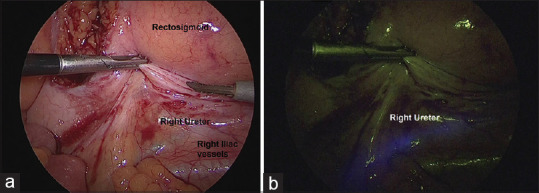
(a) The sigmoid colon is held up with umbilical cotton tape and retracted to the left by the assistant. Beginning of mediolateral dissection, (b) the ureter in near-infrared mode
Figure 4.
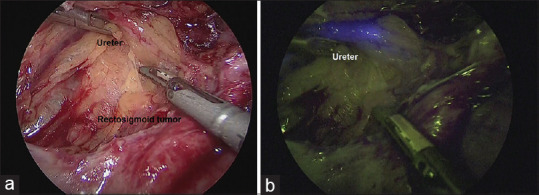
(a) The tumour is close to the left ureter, (b) dissection is being performed under near-infrared guidance
DISCUSSION
Iatrogenic ureteric injury is a rare but serious problem. Several studies estimate the incidence to be around 0.6%–1.5% for colorectal surgery.[11,12] The rate is even higher in gynaecological surgery at around 0.7%–3%.[4] The majority of these injuries go unrecognised at the time of operation resulting in pain, fever, urinary tract infection, peritonitis, urinoma formation or permanent renal damage necessitating nephrectomy.[2,3] The advantages offered by minimally invasive surgery are lost. Therefore, undoubtedly, the best way to manage a ureteral injury is to prevent it.
Surgeons and gynaecologists feel safe with a pre-operative ureteric stent, feeling that this will prevent ureteric injury. Proponents of routine stenting argue that prophylactic stents enable intraoperative detection of ureteral injury, thus facilitating earlier repair translating into significant cost savings.[13] These stents have a role in difficult situations, such as diverticulitis, rectal carcinoma, reversal of Hartmann's operation, pre-operative radiation and Crohn's disease. Opponents argue that complications resulting from the procedure such as haematuria and anuria can impair quality of life in patients who are routinely stented.[14,15]
Fluorescence imaging-guided surgery has recently found many new applications, such as assessing perfusion of bowel edges before anastomosis, visualisation of bile ducts in laparoscopic cholecystectomy, sentinel lymph node biopsy and many others.[16,17,18] There are only a few studies that have explored the use of fluorescent-guided imaging for the identification of ureters.[6,7,8,9,10,19] Methylene blue and ICG have been used. Siddighi et al. conducted their study in patients undergoing robot-assisted laparoscopic sacrocolpopexy.[6] They dissolved 25 mg of ICG in 10 ml sterile water and injected the same into each ureter with only the tip of the catheter into the ureteric orifice. The visualisation was good in all patients allowing safe dissection with no intraoperative ureteral injury. No adverse events were reported in any patient post-operatively. Yeung et al. studied eight patients with colorectal cancer, Hartmann's reversal, inflammatory bowel disease with intravenous methylene blue.[10] Ten of eleven cases were successfully visualised by fluorescence and the authors particularly found the procedure useful in four cases.
Al-Taher et al. studied fluorescence in 10 patients with varying doses of intravenous methylene blue. The ureter was visualised well when the dosage of methylene blue was 0.5 mg/kg or higher. Although no adverse reactions occurred in any patient, the risk of anaphylaxis with intravenous methylene blue is ever present.[9]
Lee et al. have reported excellent results in their cohort of 25 patients undergoing robot-assisted ureteral reconstructions.[7] In addition to visualising the ureter, they also could make out aberrant ureteral anatomy as well as identify non-viable segments of the ureter.
Since ICG is excreted exclusively in bile and is extremely safe, we attempted intraureteral catheter injection of ICG.[20] This technique allows for real-time mapping of the ureter during dissection. Furthermore, the dissection can be carried out under the NIR light, keeping the ureter out of harm's way. This seems to be a promising strategy to prevent iatrogenic ureteric injury.
CONCLUSION
Fluorescent-guided visualisation of ureters is the new ‘kid on the block’. The utility of this procedure has been described in only a few studies. As it adds visual cues to a technology lacking in tactile feedback, this makes it suitable for use in laparoscopic and robotic surgery. With the introduction of newer camera systems that can show NIR images superimposed on normal light images in real-time, ICG-NIR imaging is likely to be a game changer in surgeries involving difficult dissections.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;3 doi: 10.1002/14651858.CD003145.pub2. CD003145. doi: 10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghali AM, El Malik EM, Ibrahim AI, Ismail G, Rashid M. Ureteric injuries: Diagnosis, management, and outcome. J Trauma. 1999;46:150–8. doi: 10.1097/00005373-199901000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Visco AG, Taber KH, Weidner AC, Barber MD, Myers ER. Cost-effectiveness of universal cystoscopy to identify ureteral injury at hysterectomy. Obstet Gynecol. 2001;97:685–92. doi: 10.1016/s0029-7844(01)01193-0. [DOI] [PubMed] [Google Scholar]
- 4.Schimpf MO, Gottenger EE, Wagner JR. Universal ureteral stent placement at hysterectomy to identify ureteral injury: A decision analysis. BJOG. 2008;115:1151–8. doi: 10.1111/j.1471-0528.2008.01757.x. [DOI] [PubMed] [Google Scholar]
- 5.Chou MT, Wang CJ, Lien RC. Prophylactic ureteral catheterization in gynecologic surgery: A 12-year randomized trial in a community hospital. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:689–93. doi: 10.1007/s00192-008-0788-3. [DOI] [PubMed] [Google Scholar]
- 6.Siddighi S, Yune JJ, Hardesty J. Indocyanine green for intraoperative localization of ureter. Am J Obstet Gynecol. 2014;211:436.e1–2. doi: 10.1016/j.ajog.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 7.Lee Z, Moore B, Giusto L, Eun DD. Use of indocyanine green during robot-Assisted ureteral reconstructions. Eur Urol. 2015;67:291–8. doi: 10.1016/j.eururo.2014.08.057. [DOI] [PubMed] [Google Scholar]
- 8.Lee Z, Kaplan J, Giusto L, Eun D. Prevention of iatrogenic ureteral injuries during robotic gynecologic surgery: A review. Am J Obstet Gynecol. 2016;214:566–71. doi: 10.1016/j.ajog.2015.10.150. [DOI] [PubMed] [Google Scholar]
- 9.Al-Taher M, van den Bos J, Schols RM, Bouvy ND, Stassen LP. Fluorescence ureteral visualization in human laparoscopic colorectal surgery using methylene blue. J Laparoendosc Adv Surg Tech. 2016;26:870–5. doi: 10.1089/lap.2016.0264. [DOI] [PubMed] [Google Scholar]
- 10.Yeung TM, Volpi D, Tullis ID, Nicholson GA, Buchs N, Cunningham C, et al. Identifying ureters in situ under fluorescence during laparoscopic and open colorectal surgery. Ann Surg. 2016;263:e1–2. doi: 10.1097/SLA.0000000000001513. [DOI] [PubMed] [Google Scholar]
- 11.Liguori G, Dobrinja C, Pavan N, de Manzini N, Bucci S, Palmisano S, et al. Iatrogenic ureteral injury during laparoscopic colectomy: Incidence and prevention A current literature review. Ann Ital Chir. 2016;87:446–55. [PubMed] [Google Scholar]
- 12.Marcelissen TA, Den Hollander PP, Tuytten TR, Sosef MN. Incidence of iatrogenic ureteral injury during open and laparoscopic colorectal surgery: A single center experience and review of the literature. Surg Laparosc Endosc Percutan Tech. 2016;26:513–5. doi: 10.1097/SLE.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 13.da Silva G, Boutros M, Wexner SD. Role of prophylactic ureteric stents in colorectal surgery. Asian J Endosc Surg. 2012;5:105–10. doi: 10.1111/j.1758-5910.2012.00134.x. [DOI] [PubMed] [Google Scholar]
- 14.Bieniek JM, Meade PG. Reflux anuria after prophylactic ureteral catheter removal: A case description and review of the literature. J Endourol. 2012;26:294–6. doi: 10.1089/end.2011.0311. [DOI] [PubMed] [Google Scholar]
- 15.Wood EC, Maher P, Pelosi MA. Routine use of ureteric catheters at laparoscopic hysterectomy may cause unnecessary complications. J Am Assoc Gynecol Laparosc. 1996;3:393–7. doi: 10.1016/s1074-3804(96)80070-3. [DOI] [PubMed] [Google Scholar]
- 16.Keller DS, Ishizawa T, Cohen R, Chand M. Indocyanine green fluorescence imaging in colorectal surgery: Overview, applications, and future directions. Lancet Gastroenterol Hepatol. 2017;2:757–66. doi: 10.1016/S2468-1253(17)30216-9. [DOI] [PubMed] [Google Scholar]
- 17.Pesce A, Piccolo G, La Greca G, Puleo S. Utility of fluorescent cholangiography during laparoscopic cholecystectomy: A systematic review. World J Gastroenterol. 2015;21:7877–83. doi: 10.3748/wjg.v21.i25.7877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grischke EM, Röhm C, Hahn M, Helms G, Brucker S, Wallwiener D. ICG fluorescence technique for the detection of sentinel lymph nodes in breast cancer: Results of a prospective open-label clinical trial. Geburtshilfe Frauenheilkd. 2015;75:935–40. doi: 10.1055/s-0035-1557905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park H, Farnam R. Novel use of indocyanine green for intraoperative, real-time localization of ureter during robot-assisted excision of endometriosis. Minim Invasive Gynecol. 2015;22:S69. doi: 10.1016/j.jmig.2015.08.185. [DOI] [PubMed] [Google Scholar]
- 20.Hope-Ross M, Yannuzzi LA, Gragoudas ES, Guyer DR, Slakter JS, Sorenson JA, et al. Adverse reactions due to indocyanine green. Ophthalmology. 1994;101:529–33. doi: 10.1016/s0161-6420(94)31303-0. [DOI] [PubMed] [Google Scholar]


