Abstract
Purpose of Review
This provides up-to-date epidemiology of adolescent suicide and risk factors for suicide and highlights the overlap of risks for suicide and injury. It reviews signs and symptoms, and the up-to-date evidence on screening for depression, post-traumatic stress disorder (PTSD), suicide, substance abuse, and lethal means, and offers strategies of implementation in trauma centers.
Recent Findings
The incidence of adolescent suicide has continued to rise in the USA to 6.5 per 100,000, with notable racial disparities. The risk factors are complex, but many pre-existing risk factors and sequela after injury such as exposures to violence, suicidal behaviors, substance abuse, depression and post-traumatic stress disorder, and specific injuries including traumatic brain injury and spinal cord injury have further emerged as risks. Studies show rates of suicidality as high as 30% in the acute care setting. There are short screening instruments that can be used to universally screen for depression and suicidality in adolescent trauma patients. Step-up models of care for PTSD are promising to increase screening and services after injury. Lethal means counseling, secure firearm storage practices, and firearm safety policies can reduce the risk of suicide.
Summary
Suicide is the second leading cause of death in US adolescents, and trauma patients have significant risk factors for mental illness and suicidality before and after injury. Trauma centers should strongly consider screening adolescents, establish strategies for mental health support and referrals, and provide lethal means counseling to help prevent suicide.
Keywords: Adolescent suicide, Suicide prevention, Pediatric firearm injury, Pediatric trauma, Mental illness in traumatic injury, Post-traumatic stress disorder
Introduction
Suicide is the second leading cause of death for adolescents between the ages 10 and 19 in the USA, accounting for 2744 deaths in 2019 [1]. The incidence has been steadily rising in the USA, and 5.1% of male and 9.3% of female high school students in the USA report a suicide attempt in the past year [2]. Suicide attempts represent less than 5% of injuries treated at trauma centers in part because of the high lethality of self-inflicted firearm injuries and asphyxiation—the two leading mechanisms of suicide death in this age group, as many die prior to receiving medical care [1, 3]. In addition, many adolescents that present with self-inflicted injuries or suicidal behaviors are often treated in the emergency department (ED) and may not be encountered by the trauma team [4]. However, in a 2-year period, trauma centers participating in the National Trauma Data Bank [3] cared for 3783 adolescents with a suicide attempt, 13% of which died from their injuries [5]. Those that are admitted often have higher injury severity, healthcare utilization, and mortality compared to other intents of injury, and those that have previous attempts are at risk of future suicide attempts [6, 7••]. What we often encounter—far more than suicide attempts—are adolescents with mental illnesses and other risk factors for suicide at the time of and after injury. Given this, it is imperative that trauma centers and healthcare providers understand the epidemiology, risk factors, warning signs, and strategies to identify adolescents at risk, refer them to evidence-based mental health services, and support patients and their families.
Epidemiology
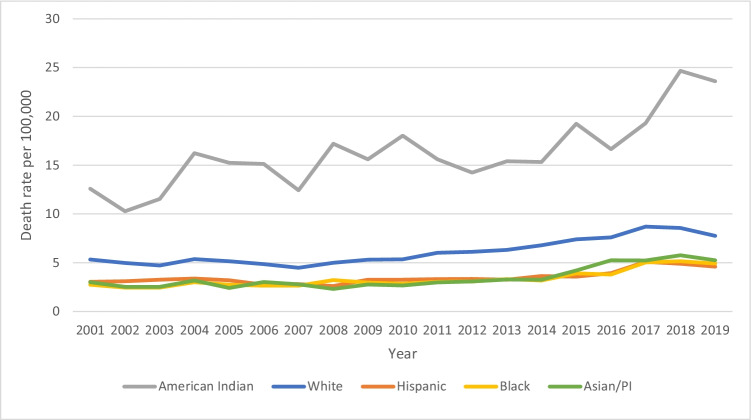
The incidence of adolescent suicide has increased from 4.57 per 100,000 in 2001 to 6.5 per 100,000 in 2019, and there are notable differences and trends among age, race, sex, and geographic region [1]. Older adolescents are more likely to die by suicide, as the incidence is 4 times higher among the ages of 15–19 compared to 10–14. Over the past 20 years, the incidence of suicide has increased for all races, with the most drastic increases in American Indian youth. American Indians have the highest incidence followed by non-Hispanic whites, reaching as high as 24 per 100,000 youths (Fig. 1). These data are alarming given the small population of American Indians in the USA, as it comprises the highest incidence of suicide mortality among all races. When comparing the rate of adolescent suicide between sexes, males have a significantly higher rate of deaths; however, female suicide rates have doubled since 2001, from 1.64 per 100,000 in 2001 to 3.48 per 100,000 in 2019. It is well established in the literature that females have significantly more suicide attempts than males, but males have higher fatalities, likely due to use of more lethal means in the form of firearms [5, 8•]. There are notable geographic differences in the incidence of adolescent suicide, with more rural, Rocky Mountain states representing the highest rates. Alaska, South Dakota, Wyoming, and Montana have the highest rates of suicides for youths aged 10–19, while the District of Columbia, New Jersey, New York, and Massachusetts report the lowest rates of suicides [1].
Fig. 1.
Incidence of suicide by race ages 10–19, 2001–2019. Data derived from Centers for Disease Control and Prevention, National Center for Health Statistics. Data are from the suicide causes of injury-related deaths by age 10–19 years old in all races from 2001 to 2019, as compiled by NCHS Vital Statistics System for numbers of deaths. Bureau of Census for population estimates. Accessed at https://www.cdc.gov/injury/wisqars/index.html
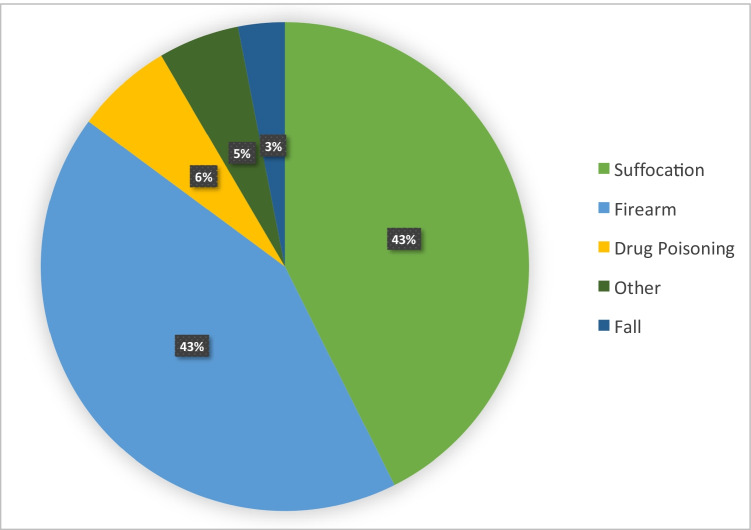
The leading mechanisms of suicide are suffocation (43%) and firearm injury (43%) (Fig. 2). Additional mechanisms include drug poisoning (6%) and falls (3%), and less than 1% each include cut/pierce, burns, drowning, and non-drug poisoning. Deaths from firearms and suffocation have been relatively stable in the past few years, although firearm deaths outnumbered other mechanisms 20 years ago; firearms accounted for 49% suicide deaths in 2001 compared to 38% which were due to suffocation/asphyxiation [1].
Fig. 2.
Mechanisms of suicide ages 10–19 (2019). Data derived from Centers for Disease Control and Prevention, National Center for Health Statistics. Data are from the suicide causes of injury-related deaths by age 10–19 years old in all races from 2001 to 2019, as compiled by NCHS Vital Statistics System for numbers of deaths. Bureau of Census for population estimates. Accessed at https://www.cdc.gov/injury/wisqars/index.html
Risk Factors and High-Risk Patient Populations
There are multiple risk factors for suicide attempts and completions at the individual, family, and community/environment levels that are important to recognize (Table 1). While there are many risk factors for suicide attempts, most individuals with these risks do not go on to attempt suicide; however, recognition of the risk factors is especially important when there are multiple risks, escalation of suicidal signs or behaviors, and when assessing adolescents and teens in acute care settings. This is critically important after experiencing a traumatic injury, as this patient population shares many overlapping risk factors for injury and adverse mental health outcomes.
Table 1.
High-risk populations and risk factors for adolescent suicide
| Individual | Interpersonal/family | Community |
|---|---|---|
| Male | Bullying | Social isolation |
| American Indian | Abuse, neglect | High economic distress |
| Non-Hispanic White | Experience/exposures to IPV, sexual abuse | Rural areas |
| LGBTQ, gender non-conforming | Social exposures to suicides in school, community | |
| Depression, PTSD, bipolar disorder | Parental mental illness, suicide attempts | High firearm ownership |
| Sleep disorders | Living in residential facility | Weak firearm safety laws |
| Past suicidal ideation, suicide attempts | Adoption, foster care | |
| Substance abuse disorders | Poor parental-child relationships | |
| Impulsivity, aggression | Low social support when identifying as LGBTQ | |
|
Pathologic computer use History of traumatic injury |
Firearm accessibility in the home |
As noted previously, there are fixed demographic groups including male sex, American Indians, and Hispanics who experience higher rates of suicide [1]. Adolescents that identify as lesbian, gay, bisexual, and non-gender conforming also have higher rates of suicidality and suicide [9, 10].
Certain mental health disorders and a history of suicide behaviors (ideation, attempts) and non-suicidal self-injury (NSSI) significantly increase risk [7••, 11]. Prior suicidal ideation, severity of ideation, and prior suicide attempts are among the highest predictors of future suicide attempts [7••]. Although most adolescents that have suicidal thoughts and behaviors do not progress to suicide attempts, they account for 26% of future suicide attempts by the age of 26 and they are strongly associated with suicide death [11]. However, it is important to note that about 68% of adolescents and young adults who attempt suicide have never had a prior suicidal thought or behavior [12]. Mental health disorders, notably depression, posttraumatic stress disorder (PTSD), sleep disturbances, bipolar disorder, substance abuse disorders and acute intoxication, psychotic symptoms, impulsivity, and aggression are risk factors for suicide, but what is especially notable is the presence of psychotic symptoms in the setting of such disorders, which can significantly increase the risk of suicide [8•, 13, 14, 15].
History of adoption, physical abuse and neglect, intimate partner violence (IPV), experience and perpetration of bullying, and pathologic Internet use are noted risk factors [8•, 16 ,17, 18, 19]. Experiencing a major life stressor or crisis such as a breakup with a dating partner or having a fight with a parent increases the risk of suicide as they increase impulsivity to act, even if never considering suicide previously [20]. Opioid misuse, which is reported in as many as 13% of high school students, increases the risk of suicidal risk behaviors, ideation, and attempts in adolescents [21, 22].
Additional risk factors pertinent to the family, the home environment, and social support systems are also noteworthy. These include having a parent with mental health problems or history of suicide, poor parental-child relationships, unsupportive parental and school beliefs when identifying as LGBTQ, social isolation resulting from not being in school or maintaining a job, housing insecurity, and living in a corrections facility or residential facility [8•, 23, 24, 25]. In addition, living in a home with a firearm increases the risk of suicide by firearm, which has a fatality rate of up to 85% [26]. Living in a home where a firearm is kept unsecured (loaded and unlocked) increases the risk of suicide compared to homes that store firearms separate from ammunition in firearm safety devices [27, 28•].
Factors related to communities, society, and policy also influence risk. The concept of suicide as a contagion among children has garnered significant interest, and some studies indicate increased risk of attempts and completion with media coverage of suicides in a community, and when adolescents learn of suicides of schoolmates [29–31]. Rural communities are known to have higher rates of adolescent suicide compared to urban ones, while other community risk factors may come into play such as poverty and unemployment, and higher firearm ownership and access [26, 32]. Lastly, adolescents’ suicide rates are higher in states with weak firearm safety laws [33].
Overlapping Burden of Risk for Injury and Suicide in the Trauma Population
Mental illness, substance abuse, and adverse childhood experiences (ACE) such as exposures to intimate partner and community violence, abuse and neglect, sexual abuse, and housing insecurity are all known risk factors for suicide and traumatic injuries and are much more common in the trauma patient population compared to the general population [34, 35]. By caring for the injured population, we are caring for a population at high risk of suicide even before their injury. This risk may only increase after injury, when the experience of trauma and its mental and physical sequela only compounds what risks one may have prior to injury.
While likely complex in association and causality, about 22% of traumatically injured patients develop a new psychiatric illness after traumatic injury, and 56% have an increased risk of developing a substance use disorder within 3 years of injury, both of which are significant risk factors for suicide [36, 37]. Suicide risk is well established for traumatic brain injury in children and adults, as suicide rates among individuals with a history of TBI are twice that of those who have not experienced TBI, and the risk is increased with TBI severity, long hospitalizations, and frequent medical encounters [38]. However, even concussion or mild TBI confers a higher risk of suicide [39•]. Spinal cord injury (SCI) is also associated with higher rates of suicidal ideation and death by suicide, with up to 11% of deaths after SCI being attributed to suicide, mostly from firearms [40].
Future risk of suicidal ideation and attempts after traumatic injuries outside of TBI and SCI are not well studied, and there are no known dedicated studies among adolescents. One of the first studies assessing suicide after traumatic injury included patients 15 and over and showed an increased risk of suicide completion after traumatic injury compared to the general population predominately among young adults, noting though that the high rates of alcohol abuse among trauma patients may attribute to this difference [41]. A more recent longitudinal study of patients aged 16 and over treated at trauma centers (without an index suicide attempt or moderate or severe TBI) demonstrated that 6% of patients experienced suicidal ideation during the follow-up period of 2 years. This risk was found to fluctuate, and notable risks included pre-existing depression, history of suicidality, recent stressful events, current level of pain, mild TBI, and current diagnoses of depression, PTSD, anxiety disorder, or substance use disorder [42]. Another study that included children and adults demonstrated that traumatic injury was associated with a 40% increase in the postinjury rate of mental health diagnoses, suicide rates were significantly higher than the general population, and patients younger than 18 years had the greatest increase in rate of postinjury mental health hospital admissions (IRR 3.3, 95% CI 1.5 to 7.2) compared to other age groups [43••].
The risk of developing PTSD post-injury is well established. A meta-analysis found that 19% of children and adolescents develop significant post-traumatic stress after injury [44]. Traumatically injured patients, especially due to violence, have a significantly increased risk of developing depression and PTSD after injury compared to those who do not experience injury, and this may lead to functional impairment and other poor outcomes [45–47]. In addition to PTSD and depression, which can independently increase the risk of suicide, there are other notable risks for suicide after injury. Surviving a violent injury, and exposure to violence from IPV and community firearm violence, increases the risk of suicidal ideation [48, 49]. Given the number of co-existing and future risks for adolescents exposed to violence, these patients are especially vulnerable to poor mental health outcomes and suicide risk.
Many trauma patients are prescribed opioids for the management of pain after traumatic injuries. Drastic increases in opioid misuse and overdoses in the past decade are associated with rising opioid prescriptions [50]. Further research as aforementioned has highlighted the increased risk of suicide behaviors and attempts with opioid misuse, placing traumatically increased trauma patients at additional risk. Of high school students reporting opioid misuse, 80% reported they were initially prescribed to them by a physician, and persistent opioid prescriptions and substance use disorders are high 4 years after traumatic injury [51, 52].
Signs and Symptoms of Major Depression and Suicide
It is imperative for clinicians to know the signs and symptoms of depression and suicide in order to refer them for further assessment and treatment and to provide early intervention when there are signs of suicidality. Outside of patients presenting with self-harm-related injuries or overtly expressing suicidal ideation, some of the signs may be subtle. Having a depressed mood most of the time, loss of interest or pleasure in usual activities, weight changes, sleep changes, restlessness or psychomotor slowing, loss of energy, feelings of worthlessness, hopelessness, purposelessness, concentration problems, irritability, and recurrent thoughts of death are all concerning signs of worsening depression in an adolescent that might be experiencing suicidal ideation [53]. It is also important to look for signs of mania or hypomania including mood changes such as depressed, elated, or irritable mood, inflated self-esteem, grandiosity, decreased need for sleep, hyper-verbal or pressured speech, racing thoughts, abrupt topic changes when talking, distractibility, agitation or restlessness, and erratic/impulsive behavior such as excessive spending, hypersexuality, or making uninhibited remarks [53]. Notably, some adolescents with depression may have difficulty in verbalizing their feelings or may deny that they are depressed or suicidal. They may instead present with mood lability, irritability, low frustration tolerance, temper tantrums or agitation, somatic complaints, and/or social withdrawal instead of verbalizing feelings of depression [54]. In addition to interviewing the adolescent, parents and caregivers should be interviewed to determine if the adolescent demonstrates warning signs associated with suicide. These warning signs include changes in eating or sleeping habits, frequent sadness, withdrawal from family, friends and regular activities, frequent physical complaints related to emotions (headaches, fatigue, stomach aches), decline in academic performance, and preoccupation with death and dying [55].
Adolescents who experience traumatic events may also have accompanying depressive symptoms as part of PTSD. Traumatic injuries and abuse are important risk factors for suicide due to alterations in mood and cognition that are part of PTSD symptomology. These include persistent exaggerated negative beliefs about oneself, blaming oneself for the traumatic event, persistent negative emotional state, loss of interest in activities, and persistent inability to experience positive emotions such as happiness, satisfaction, or loving feelings. It is important for clinicians working with injured adolescents to know that these patients may experience mood changes (sad or irritable mood) along with long periods of re-experiencing traumatic symptoms (intrusive memories, recurrent nightmares, or flashbacks) that alternate with long periods of avoidance (in talking about and avoiding/recalling the traumatic incident) and emotional numbing [56]. If avoidance and affective or emotional numbing are present, the adolescent may appear to be unaffected by the trauma, and re-experiencing symptoms may be masked [56]. This may lead to an adolescent who is at increased risk of suicide to not receive mental health screening. For this reason, it is recommended that clinicians be aware and screen adolescents for traumatic events and PTSD to help identify at-risk youth and provide appropriate referral services.
Evidence-Based Practices for Trauma Centers
Screening for Depression, PTSD, and Suicide Risk
Suicide prediction continues to pose many challenges for providers. Healthcare providers, especially those caring for high-risk populations such as trauma patients, need to be able to identify risk factors, signs of suicidal ideation, and know what screening and management strategies exist. There is not a formal recommendation for universal screening of adolescent trauma patients for depression or suicide, and many trauma centers do not have practices in place that are adequately meeting the mental health needs of their patients [57]. Less than 50% of all patients are screened for suicidality, 25% for depression, and 7% for PTSD symptoms at level I and II trauma centers across the USA [58]. This leaves up to 90% of those with post-injury PTSD or depression without assessment and care [57].
The American Academy of Pediatrics (AAP) recommends screening patients age 12 and over annually, and the United States Preventative Task Force (USPTF) recommend screening adolescent patients for depression when adequate systems exist for screening, treatment, and referrals [59, 60]. In addition, there are injury-specific recommendations to universally screen for depression and suicidal ideation among patients with spinal cord injury [61]. The American College of Surgeons Committee on Trauma (ACS COT) supports regular screening and referral for depression and PTSD in the older adolescent and adult population (over the age of 15); however, there is no firm recommendation or guidance of screening in younger patients [62]. A recent study found that 29% of patients between the ages of 10 and 12 screened positive for suicide risk when presenting to the emergency department (ED), suggesting that this age group should be included [63••]. Individuals that present to the ED with self-harm or suicidal ideation have a substantial increased risk of suicide and overall mortality in the following year, so recognition and intervention in the acute care setting are imperative [64]. Given the burden of pre-existing mental illness and other risk factors for suicide, in addition to the sequela after injury, trauma centers and caregivers for traumatically injured adolescents should strongly consider universally screening all patients ages 10 and above for depression and suicidality and developing a strategy for referrals and patient support.
There are multiple screening instruments that can be utilized for screening for depression, suicidality, and PTSD. The Patient Health Questionnaire-9 (PHQ-9), a 9-item screening instrument for depression, is validated in adults and adolescents and has a question specifically inquiring about suicidal thoughts. There is a PHQ-2 that can serve as a “rapid screen” with the remaining questions administered if positive, although the full PHQ-9 performs better in the adolescent population [65]. The Center for Epidemiological Studies Depression Scale for Children (CES-DC) was developed specifically for children [66]. The PHQ-9 is a good option for adult centers caring for patients ages 15 and over as it can be used in both teenagers and adults, while the CES-DC may be considered in pediatric trauma centers caring for younger patients. Suicide-specific instruments include the 4-item Ask Suicidal-Screening Questions (ASQ); it is easy to administer, validated among adults and adolescents, and has high sensitivity in the pediatric ED population [67]. Based on the diagnostic criteria for PTSD, formal PTSD assessment diagnosis cannot be performed until 30 days after exposure to a traumatic event, making the timing of assessment more appropriate at follow-up or via telehealth assessments. The Child PTSD Symptom Scale (CPSS) can be utilized to screen for PTSD in children and is validated in traumatized children over the age of 7 [68].
Referral and Treatment
If there is a clinical concern for severe depression and suicidal ideation, or if the patient screens positive, they should not be discharged without a psychiatric evaluation [53]. Patients and their families should be referred to mental healthcare for further evaluation and treatment which can take the form of a psychiatric consult or evaluation by a qualified mental health professional such as a mental health social worker or clinical psychologist. Discharge can be considered if the clinician is satisfied that adequate supervision and support will be available to the adolescent over the next few days and if the caregiver has agreed to perform suicide safety procedures, including removal/safe storage of lethal medications and firearms and ensuring outpatient follow-up [53]. If a patient presents with injuries from a suicide attempt or self-harm behaviors, this mandates psychiatric evaluation, and many patients may need inpatient psychiatric treatment after clearance from medical and surgical care.
Although beyond the scope of this review, there are multiple therapies that may be provided by mental health providers with varying levels of evidence including cognitive behavioral psychotherapy and pharmacologic therapy; however, some studies have shown there is a small increased risk of suicidal behaviors after initiation of some anti-depressant medications [60]. Thus, it is important to note that initiation of pharmacotherapy should only be done in conjunction with psychiatric support and plans for close outpatient follow-up and monitoring. Whether pharmacologic therapies are employed or not, early and frequent follow-up is associated with reduced suicide risk among adolescents with suicidal behavior [69].
Substance Abuse Screening and Intervention
As substance abuse and acute intoxication increase the risk of injury and injury recidivism, the ACS COT and Pediatric Trauma Society (PTS) recommend that adolescents over the age of 12 be provided Screening, Brief Intervention and Referral to Treatment (SBIRT) to help patients obtain substance abuse treatment services and reduce recidivism [70]. While the impact of SBIRT on adolescents and teens is less understood compared to adults, recognizing alcohol and substance abuse in conjunction with other mental health disorders and suicidal ideation is important, as substance abuse is not only an independent risk factor for suicide, alcohol and illicit substance use further potentiates the risk of suicide among youth with depression [11, 71]. A total of 18–30% of pediatric patients screen positive for substance use or risky substance use behaviors [72, 73]. Studies demonstrate relatively low adherence to screening recommendations in pediatric trauma centers, significant variation in who is screened based on age, injury severity, and mechanism of injury, and disparities in referrals for support services [72–74]. There are strategies demonstrated to improve screening and intervention. These include utilizing both biomarkers (blood alcohol content and urine drug screens) and validated instruments such as the CRAFFT or Alcohol Use and Disorders Identification Test (AUDIT) for screening, universal screening rather than selective screening at the time of presentation for patients ages 12 and over, integration of screening prompts in the electronic medical record (EMR), and multi-disciplinary protocols and training for all staff on SBIRT [72–76].
Lethal Means Counseling
Firearms are lethal 74–85% of the time when used for a suicide attempt and tied for the second leading mechanism of adolescent suicide [1, 26]. Over 13 million children in the USA live in homes with firearms and about 4.6 million of those reside in homes where guns are improperly stored (i.e., loaded and unlocked) [70]. These are pre-COVID estimates and the FBI has reported a significant rise in background checks during the ongoing COVID-19 pandemic, so the prevalence of unsecured firearms in homes with youth is likely much higher [77]. Adolescents identified as at risk of suicide (mental illness, suicidality) are just as likely to report living in a home with firearm access as adolescents without such risks with 1 in 3 reporting access, and 90% of guns used in youth suicide come from the child’s home or the home of a friend or relative [78, 79]. Children and adolescents, especially in the setting of trauma, are a high-risk demographic group for suicide and should be considered for routine firearm screening and secure storage counseling interventions [80]. The AAP recommends routine screening and counseling, and firearm safety storage and counseling is supported by multiple major medical societies including the ACS [81, 82••].
Responsible storage (storing guns locked, unloaded, and separate from ammunition) decreases risk for firearm suicide by up to 85% [83]. Up to a third of youth suicides and unintentional firearm deaths could be prevented through simple secure storage counseling interventions [84•]. Studies have demonstrated that brief physician counseling, combined with provision of a safe storage device, is effective at increasing safe storage of home firearms, and multiple studies have found similar findings [85].
The majority of healthcare providers agree that they should provide firearm counseling but report many barriers to doing so including lack of time, inadequate training, and low self-efficacy [86]. Educating providers and integration of secure storage screening and counseling into routine care can increase the efficacy of lethal means screening. We have done this at our institution with the implementation of the Be SMART for Kids program, which is an evidence-informed and AAP-aligned educational program for adults that aims to reduce unintentional shootings and youth suicide through the promotion of secure firearm storage in the home [87]. After providing education to pediatric residents and integrating prompts in the EMR, we significantly increased the frequency of firearm screening and secure storage counseling during well-child checks [88]. For further guidance, Wintemute et al. have outlined multiple resources on firearm access screening and counseling including specific questions, brief interventions, patient and family educational materials, and secure firearm storage options [89].
Although drug overdoses represent a smaller portion of suicides in adolescents, many patients are prescribed medications to treat pain after traumatic injuries, and it is important to integrate opioid misuse prevention strategies and counseling for patients and their caregivers since opioids increase the risk of misuse, overdose, and suicide [50]. There is also a valid concern that many opioid overdose deaths are misclassified as unintentional overdose; therefore, the burden of suicide is likely underappreciated [90]. There is more guidance and recommendations provided about pain management strategies to increase utilization of non-opioid analgesia and reduce doses of outpatient prescriptions [50, 91]. In addition to providing substance abuse screening and intervention, counseling should be provided to caregivers about providing oversight for adolescent opioid use, monitoring doses, storage, and safe disposal after no longer needing the medication to help reduce misuse.
Proposed Models of Implementation and Care
Depression, Suicidality, Substance Abuse, and Lethal Means Screening—“Bundling” Risk Assessments
Before initiating screening for depression and suicidality, there should be well-established protocols on the screening instrument, the target age group, the timing of screening, who is performing the screening, and referrals for further assessment, treatment, and follow-up. This will depend on the resources available and structure of the trauma team. Given adolescent patients are treated at both adult and pediatric trauma centers, it is important to have cross collaboration to standardize screening and referral pathways. It may also be helpful to select instruments such as the PHQ-9 and ASQ, which are easy to administer and can be used in both adolescent and adult populations [65, 66]. Teams should establish clinical partnerships with mental health experts at their facilities such as psychiatrists, clinical psychologists, and mental health clinical social workers, and should include clinical stakeholders in the development of processes and protocols in order to increase successful implementation of screening and referrals, and to achieve buy-in from team members.
All screening and inquiry should be performed alone with the adolescent patient and delivered with trauma-informed principles. It should be performed after the initial acute phase of care in the setting of a potentially distressing or life-threatening injury, and in the absence of severe pain or in the setting of altered mental status from medications, TBI, or cognitive impairment. If a self-inflicted injury is suspected, earlier inquiry should be performed to ensure the safety of the patient. The individual performing screening may vary between centers based on resources; however, they should be comfortable with the selected instruments and have a protocol to follow for immediate referrals if screening positive for depression or suicidality. Given the overlapping risk factors in the trauma population, it is prudent to consider screening for substance abuse, depression/suicide, and lethal means access collectively, in addition to other high-risk behaviors or exposures such as social determinants of health, exposures to violence, and other risks for injury in the home. Trauma center social workers may be in the ideal position to perform screening during their assessments, and clinical psychologists, if available, may also be key team members to perform screening and brief interventions. Other clinical team members can incorporate screening into the tertiary survey. Given what is known about low comfort levels and efficacy of clinician screening for depression and lethal means, it is important to provide guidance to trainees and there should be prompts in the EMR to both improve efficacy, adherence to the instrument, and documentation [88, 91]. Any positive screen should prompt referral to the appropriate mental health provider for further evaluation, safety planning, treatment, and follow-up, and the detection of a firearm in the home should be accompanied by education to the caregiver on lethal means access, counseling for secure storage and if available, provision of a firearm lock, or information on options for temporary relinquishment or safe storage. [80]
PTSD Screening, Monitoring and Step-up Care—a Promising Model for Trauma Centers
There are many barriers reported by trauma centers in providing mental health assessments and services, notably time, expertise, and resource constraints [92]. While many patients are “captured” while admitted for assessment at that time, monitoring for the development of adverse mental health outcomes such as PTSD is even more challenging after a patient is discharged. A promising model of assessing and providing treatment PTSD for patients after traumatic injury is the step-up model of care that provides universal screening for PTSD, but focuses time and resources for intervention on only those that screen positive. This model has demonstrated improved outcomes related to PTSD and improved quality of life and is utilized in our trauma center for patients and pediatric caregivers [93, 94•]. Our Trauma Resilience and Recovery Program (TRRP) utilizes mental health providers including clinical psychologists and supervised trainees provide early brief interventions on coping strategies for acute distress at the index hospitalization, and 30-day follow-up screening for depression and PTSD via telephone for those that agree to follow-up, including children and caregivers. Those that screen positive are provided with either in-person or telehealth interventions such as trauma-focused cognitive behavioral therapy (CBT), Parent–Child Interaction Therapy (PCIT), cognitive processing therapy, and brief behavioral activation for depression for caregivers if needed. Patients and families with more complex psychiatric or substance abuse needs are referred for other services including psychiatric care. Evaluation of the program that included teen and adult patients demonstrated 98% of patients accepted enrollment for PTSD screening and of the 36% that screened positive, and 75% either accepted referrals or were already receiving care [94•]. The high acceptance of telehealth services may improve access to care, especially to those in rural communities with fewer mental health providers. The TRRP program is now being propagated in trauma centers throughout South Carolina and North Carolina, with further plans for outcome evaluation. Other models of PTSD stepped care delivery including staffing and funding models are outlined by deRoon-Cassini et al. [95].
Advocating for Policies Demonstrated to Reduce Adolescent Teen Suicide
The complexity of risks and contributors for adolescent suicide make it difficult to identify specific policies or areas of advocacy that definitively reduce the risk of suicide. Addressing a combination of factors at the social-ecological level including reduction of adverse childhood experiences and childhood trauma, early identification of at risk youth, improving programs to promote community and peer connectedness, improved access to mental healthcare, and further research to develop efficacious intervention and treatment programs may all reduce theoretically reduce risk of adverse mental health outcomes and suicides [96]. However, some of the policies with a meaningful demonstration of reducing adolescent suicide are state policies that promote safe firearm ownership and reduce access to those at risk of suicide. Higher minimum ages for firearm ownership and concealed carry (> 21), permit-to-purchase laws, minimum waiting periods for purchase, and child access prevention laws are associated with lower rates of adolescent suicide [97–99]. Many professional medical, surgical, and trauma societies support the implementation of such policies that have the potential to meaningfully reduce suicide through policies promoting safe firearm ownership [100].
Conclusion
As a leading cause of death in adolescents, trauma centers are in unique positions to identify adolescents at risk of suicide. The co-occurring risk factors for suicide and injury including mental illness, exposures to violence, and substance abuse, in addition to the elevated risk after injury, especially in specific injuries such as TBI, SCI, and assault, all contribute to making the adolescent trauma patient population very high risk for suicide [8•, 38, 40, 41, 42, 43••]. This suggests that trauma providers should not only recognize the risks and signs of suicidality, but should strongly consider using validated instruments to universally screen for depression and suicide, and have plans for referral and treatment in conjunction with mental health partners [59, 60, 63••, 65, 66, 67, 68, 69]. Lethal means reduction via counseling and securing firearms with a safety device is a demonstrated, evidence-based strategy for suicide prevention [85]. Lethal means screening and education on secure storage should accompany suicidality assessments and should be considered with substance abuse SBIRT. Step-up models of care for PTSD screening and mental health care have the potential to improve mental health support for pediatric and adult trauma patients, be adapted to meet the needs of trauma centers with varying resources, and extend services via telehealth to address barriers to mental healthcare [93, 94•, 95]. Table 2 highlights these high-yield findings and suggestions for trauma providers. Future research efforts should focus on evaluating the outcomes of universal screening among the adolescent trauma population, including the prevalence of suicidality, services referred to and received, and long-term outcomes. Future investigation on implementation strategies can help inform successful screening and interventions, especially in centers with fewer resources and personnel. Lastly, trauma providers should advocate for research and implementation of evidence-based policies that are demonstrated to reduce adolescent suicide.
Table 2.
Key points for trauma providers
| Adolescent suicide epidemiology |
| • Suicide is the second leading cause of death for US adolescents with an increasing incidence of 6.5 per 100,000, and the leading mechanisms are firearms and suffocation |
| • 5.1% of male and 9.3% of female high school students in the USA report a suicide attempt in the past year, but the incidence is reported as high as 30% in the pediatric emergency medicine setting |
| • Males, American Indians, and non-Hispanic white adolescents have the highest rates, but it is increasing among all minorities and the incidence of female suicides has doubled in the past 20 years |
| Overlapping risks of traumatic injury and suicide |
| • Mental illness, substance abuse, prior self-harm, exposures to violence, and firearm access are risk factors for traumatic injury and suicide |
| • Traumatically injured adolescents are at high risk of post-injury PTSD, suicidality, and substance abuse, especially patients that sustain traumatic brain injuries, spinal cord injuries, and violent injuries |
| Strategies for identification, intervention, and prevention |
| • Given the high risks and rates of depression and suicidality in the adolescent trauma population, trauma centers should strongly consider universal screening of adolescents ages 10 and over utilizing validated instruments such as the PHQ-9, CES-DC, and ASQ |
| • Trauma centers should screen for access to lethal means and provide counseling on safe firearm storage and prescription drug storage |
| • Centers should establish protocols for screening and referrals to mental health providers, and incorporate team education and prompts in the electronic medical record for depression, suicidality, and lethal means screening and documentation to increase efficacy of implementation |
| • Centers should consider “bundling” substance abuse SBIRT with depression, suicidality, and lethal means access screening to comprehensively identify risks and provide interventions services |
| • Step-up models of care for PTSD screening and interventions are promising models in trauma centers to improve identification and treatment in a resource-sensitive manner |
| • Policies aimed at responsible firearm ownership such as permit-to-purchase, minimum age requirement of 21 for concealed carry, child access prevention laws, and mandatory waiting periods for firearm purchase are demonstrated to reduce firearm suicides |
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical collection on Intentional Violence
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Web-based Injury Statistics Query and Reporting System. Centers for Disease Control and Prevention. https://wisqars-viz.cdc.gov:8006/lcd/home. Accessed 15 Apr 2021.
- 2.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, et al. Youth Risk Behavior Surveillance - United States, 2017. MMWR Surveill Summ. 2018;67(8):1–114. doi: 10.15585/mmwr.ss6708a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Surgeons. National Trauma Databank 2016 Annual Report. https://www.facs.org/-/media/files/quality-programs/trauma/ntdb/ntdb-annual-report-2016.ashx. Accessed 10 April 2021.
- 4.Sawyer SM, Patton GC. Why are so many more adolescents presenting to our emergency departments with mental health problems? Med J Aust. 2018;208(8):339–340. doi: 10.5694/mja18.00213. [DOI] [PubMed] [Google Scholar]
- 5.Mathews EM, Woodward CJ, Musso MW, Jones GN. Suicide attempts presenting to trauma centers: trends across age groups using the National Trauma Data Bank. Am J Emerg Med. 2016;34(8):1620–1624. doi: 10.1016/j.ajem.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Deng H, Yue JK, Winkler EA, Dhall SS, Manley GT, Tarapore PE. Pediatric firearm-related traumatic brain injury in United States trauma centers. J Neurosurg Pediatr. 2019;6:1–11. doi: 10.3171/2019.5.PEDS19119. [DOI] [PubMed] [Google Scholar]
- 7.•• King CA, Grupp-Phelan J, Brent D, Dean JM, Webb M, Bridge JA, et al. Pediatric Emergency Care Applied Research Network. Predicting 3-month risk for adolescent suicide attempts among pediatric emergency department patients. J Child Psychol Psychiatry. 2019;60(10):1055–1064. 10.1111/jcpp.13087. This study found that after presenting to the ED for any complaint, 5% of adolescents between the ages of 12 and 17 reported a suicide attempt 3 months after the visit. Prior suicidal thoughts and suicidal ideation were predictive of attempt, and school connectedness was protective. This highlights the high risk of future suicide attempt if suicidality is present on presentation to ED visits in the adolescent population, and suggests the importance of screening all adolescents at these visits. [DOI] [PMC free article] [PubMed]
- 8.Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health. 2019;64(2):265–283. doi: 10.1007/s00038-018-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guz S, Kattari SK, Atteberry-Ash B, Klemmer CL, Call J, Kattari L. Depression and suicide risk at the cross-section of sexual orientation and gender identity for youth. J Adolesc Health. 2021;68(2):317–323. doi: 10.1016/j.jadohealth.2020.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Thoma BC, Salk RH, Choukas-Bradley S, Goldstein TR, Levine MD, Marshal MP. Suicidality disparities between transgender and cisgender adolescents. Pediatrics. 2019;144(5):e20191183. doi: 10.1542/peds.2019-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mars B, Heron J, Klonsky ED, Moran P, O'Connor RC, Tilling K, Wilkinson P, Gunnell D. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry. 2019;6(4):327–337. doi: 10.1016/S2215-0366(19)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castellví P, Lucas-Romero E, Miranda-Mendizábal A, Parés-Badell O, Almenara J, Alonso I, et al. Longitudinal association between self-injurious thoughts and behaviors and suicidal behavior in adolescents and young adults: a systematic review with meta-analysis. J Affect Disord. 2017;215:37–48. doi: 10.1016/j.jad.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 13.Kelleher I, Corcoran P, Keeley H, et al. Psychotic symptoms and population risk for suicide attempt: a prospective cohort study. JAMA Psychiat. 2013;70(9):940–948. doi: 10.1001/jamapsychiatry.2013.140. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76(1):84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 16.Slap G, Goodman E, Huang B. Adoption as a risk factor for attempted suicide during adolescence. Pediatrics. 2001;108(2):E30. doi: 10.1542/peds.108.2.e30. [DOI] [PubMed] [Google Scholar]
- 17.Messias E, Castro J, Saini A, Usman M, Peeples D. Sadness, suicide, and their association with video game and internet overuse among teens: results from the youth risk behavior survey 2007 and 2009. Suicide Life Threat Behav. 2011;41(3):307–315. doi: 10.1111/j.1943-278X.2011.00030.x. [DOI] [PubMed] [Google Scholar]
- 18.Stanley IH, Horowitz LM, Bridge JA, Wharff EA, Pao M, Teach SJ. Bullying and suicide risk among pediatric emergency department patients. Pediatr Emerg Care. 2016;32(6):347–351. doi: 10.1097/PEC.0000000000000537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Copeland WE, Wolke D, Angold A, Costello EJ. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiat. 2013;70(4):419–426. doi: 10.1001/jamapsychiatry.2013.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zygo M, Pawłowska B, Potembska E, Dreher P, Kapka-Skrzypczak L. Prevalence and selected risk factors of suicidal ideation, suicidal tendencies and suicide attempts in young people aged 13–19 years. Ann Agric Environ Med. 2019;26(2):329–336. doi: 10.26444/aaem/93817. [DOI] [PubMed] [Google Scholar]
- 21.Wilkins NJ, Clayton H, Jones CM, Brown M. Current prescription opioid misuse and suicide risk behaviors among high school students. Pediatrics. 2021;1:e2020030601. doi: 10.1542/peds.2020-030601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baiden P, Graaf G, Zaami M, Acolatse CK, Adeku Y. Examining the association between prescription opioid misuse and suicidal behaviors among adolescent high school students in the United States. J Psychiatr Res. 2019;112:44–51. doi: 10.1016/j.jpsychires.2019.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Geulayov G, Gunnell D, Holmen TL, Metcalfe C. The association of parental fatal and non-fatal suicidal behaviour with offspring suicidal behaviour and depression: a systematic review and meta-analysis. Psychol Med. 2012;42(8):1567–1580. doi: 10.1017/S0033291711002753. [DOI] [PubMed] [Google Scholar]
- 24.Rimes KA, Shivakumar S, Ussher G, Baker D, Rahman Q, West E. Psychosocial factors associated with suicide attempts, ideation, and future risk in lesbian, gay, and bisexual youth. crisis. 2019;40(2):83–92. 10.1027/0227-5910/a000527. [DOI] [PubMed]
- 25.Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics. 2011;127(5):896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5–14. doi: 10.1016/j.ypmed.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- 28.Swanson SA, Eyllon M, Sheu YH, Miller M. Firearm access and adolescent suicide risk: toward a clearer understanding of effect size. Inj Prev. 2020 doi: 10.1136/injuryprev-2019-043605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gould MS, Kleinman MH, Lake AM, Forman J, Midle JB. Newspaper coverage of suicide and initiation of suicide clusters in teenagers in the USA, 1988–96: a retrospective, population-based, case-control study. Lancet Psychiatry. 2014;1(1):34–43. doi: 10.1016/S2215-0366(14)70225-1. [DOI] [PubMed] [Google Scholar]
- 30.Hawton K, Hill NT, Gould M, John A, Lascelles K, Robinson J. Clustering of suicides in children and adolescents. Lancet Child Adolesc Health. 2020;4:58–67. doi: 10.1016/S2352-4642(19)30335-9. [DOI] [PubMed] [Google Scholar]
- 31.Swanson SA, Colman I. Association between exposure to suicide and suicidality outcomes in youth. CMAJ. 2013;185(10):870–877. doi: 10.1503/cmaj.121377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knopov A, Sherman RJ, Raifman JR, Larson E, Siegel MB. Household gun ownership and youth suicide rates at the state level, 2005–2015. Am J Prev Med. 2019;56(3):335–342. doi: 10.1016/j.amepre.2018.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goyal MK, Badolato GM, Patel SJ, Iqbal SF, Parikh K, McCarter R. State gun laws and pediatric firearm-related mortality. Pediatrics. 2019;144(2):e20183283. doi: 10.1542/peds.2018-3283. [DOI] [PubMed] [Google Scholar]
- 34.Dicker RA, Mah J, Lopez D, Tran C, Reidy R, Moore M, et al. Screening for mental illness in a trauma center: rooting out a risk factor for unintentional injury. J Trauma. 2011;70(6):1337–1344. doi: 10.1097/TA.0b013e318216f611. [DOI] [PubMed] [Google Scholar]
- 35.Guinn AS, Ports KA, Ford DC, Breiding M, Merrick MT. Associations between adverse childhood experiences and acquired brain injury, including traumatic brain injuries, among adults: 2014 BRFSS North Carolina. Inj Prev. 2019;25(6):514–520. doi: 10.1136/injuryprev-2018-042927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. Am J Psychiatry. 2010;167(3):312–320. doi: 10.1176/appi.ajp.2009.09050617. [DOI] [PubMed] [Google Scholar]
- 37.Zatzick DF, Grossman DC. Association between traumatic injury and psychiatric disorders and medication prescription to youths aged 10–19. Psychiatr Serv. 2011;62(3):264–271. doi: 10.1176/ps.62.3.pss6203_0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Madsen T, Erlangsen A, Orlovska S, Mofaddy R, Nordentoft M, Benros ME. Association between traumatic brain injury and risk of suicide. JAMA. 2018;320(6):580–588. doi: 10.1001/jama.2018.10211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fralick M, Sy E, Hassan A, Burke MJ, Mostofsky E, Karsies T. Association of concussion with the risk of suicide: a systematic review and meta-analysis. JAMA Neurol. 2019;76(2):144–151. doi: 10.1001/jamaneurol.2018.3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kennedy P, Garmon-Jones L. Self-harm and suicide before and after spinal cord injury: a systematic review. Spinal Cord. 2017;55(1):2–7. doi: 10.1038/sc.2016.135. [DOI] [PubMed] [Google Scholar]
- 41.Ryb GE, Soderstrom CA, Kufera JA, Dischinger P. Longitudinal study of suicide after traumatic injury. J Trauma. 2006;61(4):799–804. doi: 10.1097/01.ta.0000196763.14289.4e. [DOI] [PubMed] [Google Scholar]
- 42.Bryant RA, O'Donnell ML, Forbes D, McFarlane AC, Silove D, Creamer M. The course of suicide risk following traumatic injury. J Clin Psychiatry. 2016;77(5):648–653. doi: 10.4088/JCP.14m09661. [DOI] [PubMed] [Google Scholar]
- 43.•• Evans CCD, DeWit Y, Seitz D, Mason S, Nathens A, Hall S. Mental health outcomes after major trauma in Ontario: a population-based analysis. CMAJ. 2018.12;190(45):E1319-E1327. 10.1503/cmaj.180368. This study found that trauma patients experienced a 40% increase in post-injury mental health diagnosis, suicide rates were significantly higher than the general population at 70 per 100,000, and adolescents experienced the highest increase rate of mental health–related hospital admissions out of all trauma patients. This is one of the few studies demonstrating the heightened risk of suicide after experiencing traumatic injuries outside of TBI and SCI. [DOI] [PMC free article] [PubMed]
- 44.Kahana SY, Feeny NC, Youngstrom EA, Drotar D. Posttraumatic stress in youth experiencing illnesses and injuries: an exploratory meta-analysis. Traumatology. 2006;12(2):148–161. doi: 10.1177/1534765606294562. [DOI] [Google Scholar]
- 45.Vibhakar V, Allen LR, Gee B, Meiser-Stedman R. A systematic review and meta-analysis on the prevalence of depression in children and adolescents after exposure to trauma. J Affect Disord. 2019;255:77–89. doi: 10.1016/j.jad.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 46.Zatzick DF, Jurkovich GJ, Fan MY, Grossman D, Russo J, Katon W, Rivara FP. Association between posttraumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Arch Pediatr Adolesc Med. 2008;162(7):642–648. doi: 10.1001/archpedi.162.7.642. [DOI] [PubMed] [Google Scholar]
- 47.Rivara F, Adhia A, Lyons V, Massey A, Mills B, Morgan E, Simckes M, Rowhani-Rahbar A. The effects of violence on health. Health Aff (Millwood) 2019;38(10):1622–1629. doi: 10.1377/hlthaff.2019.00480. [DOI] [PubMed] [Google Scholar]
- 48.Hsu HT, Fulginiti A, Petering R, Barman-Adhikari A, Maria DS, Shelton J, Bender K, Narendorf S, Ferguson K. Firearm violence exposure and suicidal ideation among young adults experiencing homelessness. J Adolesc Health. 2020;67(2):286–289. doi: 10.1016/j.jadohealth.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith ME, Sharpe TL, Richardson J, Pahwa R, Smith D, DeVylder J. The impact of exposure to gun violence fatality on mental health outcomes in four urban US settings. Soc Sci Med. 2020;246:112587. doi: 10.1016/j.socscimed.2019.112587. [DOI] [PubMed] [Google Scholar]
- 50.Oquendo MA, Volkow ND. Suicide: a silent contributor to opioid-overdose deaths. N Engl J Med. 2018;26;378(17):1567–1569. 10.1056/NEJMp1801417. [DOI] [PubMed]
- 51.McCabe SE, West BT, Teter CJ, Boyd CJ. Medical and nonmedical use of prescription opioids among high school seniors in the United States. Arch Pediatr Adolesc Med. 2012;166(9):797–802. doi: 10.1001/archpediatrics.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bell TM, Raymond J, Vetor A, Mongalo A, Adams Z, Rouse T, Carroll A. Long-term prescription opioid utilization, substance use disorders, and opioid overdoses after adolescent trauma. J Trauma Acute Care Surg. 2019;87(4):836–840. doi: 10.1097/TA.0000000000002261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 2001;40(7 Suppl):24S-51S. 10.1097/00004583-200107001-00003. [DOI] [PubMed]
- 54.Birmaher B, Brent D. AACAP Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503–1526. doi: 10.1097/chi.0b013e318145ae1c. [DOI] [PubMed] [Google Scholar]
- 55.AACAP. Frequently Asked Questions. Retrieved April 24, 2021, from Aacap.org website: https://www.aacap.org/AACAP/Families_and_Youth/Resource_Centers/Suicide_Resource_Center/FAQ.aspx. Accessed 20 Apr 2021.
- 56.Cohen JA, Bukstein O, Walter H, Benson SR, Chrisman A, Farchione TR, et al. AACAP Work Group On Quality Issues Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(4):414–430. [PubMed] [Google Scholar]
- 57.Fakhry SM, Ferguson PL, Olsen JL, Haughney JJ, Resnick HS, Ruggiero KJ. Continuing trauma: the unmet needs of trauma patients in the post-acute care setting. Am Surg. 2017;83:1308–1314. doi: 10.1177/000313481708301137. [DOI] [PubMed] [Google Scholar]
- 58.Love J, Zatzick D. A survey of screening & intervention for comorbid alcohol, drugs, suicidality, depression & PTSD at trauma centers. Psychiatr Serv. 2014;65:918–923. doi: 10.1176/appi.ps.201300399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.USPTF Final Recommendation Statement: Depression in Children and Adolescents. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/depression-in-children-and-adolescents-screening. Published Feb 8 2016. Accessed 12 Apr 2021.
- 60.Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D; GLAD-PC STEERING GROUP. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141(3):e20174081. 10.1542/peds.2017-4081. [DOI] [PubMed]
- 61.Management of mental health disorders substance use disorders, and suicide in adults with spinal cord injury. J Spinal Cord Med. 2021;44(1):102–162. doi: 10.1080/10790268.2021.1863738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.American College of Surgeons Committee on Trauma Statement on Post-Traumatic Stress Disorder in Adults. Published online Feb 1, 2018. https://www.facs.org/about-acs/statements/109-adult-ptsd. Accessed 12 Apr 2021.
- 63.Lanzillo EC, Horowitz LM, Wharff EA, Sheftall AH, Pao M, Bridge JA. The importance of screening preteens for suicide risk in the emergency department. Hosp Pediatr. 2019;9(4):305–307. doi: 10.1542/hpeds.2018-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goldman-Mellor S, Olfson M, Lidon-Moyano C, Schoenbaum M. Association of suicide and other mortality with emergency department presentation. JAMA Netw Open. 2019;2(12):e1917571. doi: 10.1001/jamanetworkopen.2019.17571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Allgaier AK, Pietsch K, Frühe B, SiglGlöckner J, Schulte-Körne G. Screening for depression in adolescents: validity of the patient health questionnaire in pediatric care. Depress Anxiety. 2012;29(10):906–913 47. [DOI] [PubMed]
- 66.Center for Epidemiological Studies Depression Scale for Children (CES-DC): instructions for use. https://www.brightfutures.org/mentalhealth/pdf/professionals/bridges/ces_dc.pdf. Accessed 20 Apr 2021.
- 67.Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, Wharff EA, Ginnis K, Cannon E, Joshi P, Pao M. Ask Suicide-Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–1176. doi: 10.1001/archpediatrics.2012.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Foa EB, Asnaani A, Zang Y, Capaldi S, Yeh R. Psychometrics of the Child PTSD Symptom scale for DSM-5 for trauma-exposed children and adolescents. J Clin Child Adolesc Psychol. 2018;47(1):38–46. doi: 10.1080/15374416.2017.1350962. [DOI] [PubMed] [Google Scholar]
- 69.Inagaki M, Kawashima Y, Yonemoto N, Yamada M. Active contact and follow-up interventions to prevent repeat suicide attempts during high-risk periods among patients admitted to emergency departments for suicidal behavior: a systematic review and meta-analysis. BMC Psychiatry. 2019;25;19(1):44. 10.1186/s12888-019-2017-7. [DOI] [PMC free article] [PubMed]
- 70.Kelleher DC, Renaud EJ, Ehrlich PF, Burd RS. Pediatric Trauma Society Guidelines Committee. Guidelines for alcohol screening in adolescent trauma patients: a report from the Pediatric Trauma Society Guidelines Committee. J Trauma Acute Care Surg. 2013 74(2):671–82. 10.1097/TA.0b013e31827d5f80. [DOI] [PubMed]
- 71.Yuma-Guerrero PJ, Lawson KA, Velasquez MM, von Sternberg K, Maxson T, Garcia N. Screening, brief intervention, and referral for alcohol use in adolescents: a systematic review. Pediatrics. 2012;130(1):115–122. doi: 10.1542/peds.2011-1589. [DOI] [PubMed] [Google Scholar]
- 72.Maung AA, Becher RD, Schuster KM, Davis KA. When should screening of pediatric trauma patients for adult behaviors start? J Trauma Surg Acute Open. 2018;3:e000181. doi: 10.1136/tsaco-2018-000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Johnson KN, Raetz A, Harte M, McMahon LE, Grandsoult V, Garcia-Filion P, Notrica DM. Pediatric trauma patient alcohol screening: a 3 year review of screening at a level I pediatric trauma center using the CRAFFT tool. J Pediatr Surg. 2014;49(2):330–332. doi: 10.1016/j.jpedsurg.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 74.Robinson T, Tarzi C, Zhou XG, Bailey K. Screening for alcohol and substance use in pediatric trauma patients: a retrospective review. J Pediatr Surg. 2020;55(5):921–925. doi: 10.1016/j.jpedsurg.2020.01.042. [DOI] [PubMed] [Google Scholar]
- 75.Roubil JG, Hazeltine MD, Bludevich BM, Aidlen JT, Pustis N, Ferrante C, Hirsh MP, Cleary MA. Assessing screening, brief intervention, and referral to treatment (SBIRT) compliance and disparities for pediatric inpatients at a tertiary care facility. J Pediatr Surg. 2021;S0022–3468(21):00666–667. doi: 10.1016/j.jpedsurg.2021.09.048. [DOI] [PubMed] [Google Scholar]
- 76.Zimmermann E, Sample JM, Zimmermann ME, Sullivan F, Stankiewicz S, Saldinger P. Successful implementation of an alcohol screening, brief intervention, and referral to treatment program. J Trauma Nurs. 2018;25(3):196–200. doi: 10.1097/JTN.0000000000000368. [DOI] [PubMed] [Google Scholar]
- 77.Azrael D, Cohen J, Salhi C, Miller M. Firearm storage in gun-owning households with children: results of a 2015 national survey. J Urban Health. 2018;95(3):295–304. 2. [DOI] [PMC free article] [PubMed]
- 78.Grossman DC, Reay DT, Baker SA. Self-inflicted and unintentional firearm injuries among children and adolescents: the source of the firearm. Arch Pediatr Adolesc Med. 1999;153(8):875–878. doi: 10.1001/archpedi.153.8.875. [DOI] [PubMed] [Google Scholar]
- 79.Simonetti JA, Mackelprang JL, Rowhani-Rahbar A, Zatzick D, Rivara FP. Psychiatric comorbidity, suicidality, and in-home firearm access among a nationally representative sample of adolescents. JAMA Psychiat. 2015;72(2):152–159. doi: 10.1001/jamapsychiatry.2014.1760. [DOI] [PubMed] [Google Scholar]
- 80.Wintemute GJ, Betz ME, Ranney ML. Yes, you can: physicians, patients, and firearms. Ann Intern Med. 2016;165(3):205–213. doi: 10.7326/M15-2905. [DOI] [PubMed] [Google Scholar]
- 81.Dowd MD, Sege RD. Council on Injury, Violence, and Poison Prevention Executive Committee; American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2012;130(5):e1416–23. doi: 10.1542/peds.2012-2481. [DOI] [PubMed] [Google Scholar]
- 82.Bulger EM, Kuhls DA, Campbell BT, Bonne S, Cunningham RM, Betz M, et al. Proceedings from the medical summit on firearm injury prevention: a public health approach to reduce death and disability in the US. J Am Coll Surg. 2019;229(4):415–430.e12. doi: 10.1016/j.jamcollsurg.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 83.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- 84.Monuteaux MC, Azrael D, Miller M. Association of increased safe household firearm storage with firearm suicide and unintentional death among US youths. JAMA Pediatr. 2019;173(7):657–662. doi: 10.1001/jamapediatrics.2019.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rowhani-Rahbar A, Simonetti JA, Rivara FP. Effectiveness of interventions to promote safe firearm storage. Epidemiol Rev. 2016;38(1):111–124. doi: 10.1093/epirev/mxv006. [DOI] [PubMed] [Google Scholar]
- 86.Webster DW, Wilson ME, Duggan AK, Pakula LC. Firearm injury prevention counseling: a study of pediatricians’ beliefs and practices. Pediatrics. 1992;89(5 Pt 1):902–907. doi: 10.1542/peds.89.5.902. [DOI] [PubMed] [Google Scholar]
- 87.Be SMART for Kids. https://besmartforkids.org/. Accessed 12 Apr 2021.
- 88.Gastineau KAB, Stegall CL, Lowrey LK, Giourgas BK, Andrews AL. Improving the frequency and documentation of gun safety counseling in a resident primary care clinic. Acad Pediatr. 2021;21(1):117–123. doi: 10.1016/j.acap.2020.07.013. [DOI] [PubMed] [Google Scholar]
- 89.Hyland SJ, Brockhaus KK, Vincent WR, Spence NZ, Lucki MM, Howkins MJ, Cleary RK. Perioperative pain management and opioid stewardship: a practical guide. Healthcare (Basel) 2021;9(3):333. doi: 10.3390/healthcare9030333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yaster M, McNaull PP, Davis PJ. The opioid epidemic in pediatrics: a 2020 update. Curr Opin Anaesthesiol. 2020;33(3):327–334. doi: 10.1097/ACO.0000000000000865. [DOI] [PubMed] [Google Scholar]
- 91.Sudhanthar S, Thakur K, Sigal Y, Turner J. Improving validated depression screen among adolescent population in primary care practice using electronic health records (EHR). BMJ Qual Improv Rep. 2015;4(1):u209517.w3913. 10.1136/bmjquality.u209517.w3913. [DOI] [PMC free article] [PubMed]
- 92.Powers MB, Warren AM, Rosenfield D, Roden-Foreman K, Bennett M, Reynolds MC, Davis ML, Foreman ML, Petrey LB, Smits JA. Predictors of PTSD symptoms in adults admitted to a level I trauma center: a prospective analysis. J Anxiety Disord. 2014;28(3):301–309. doi: 10.1016/j.janxdis.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Dunn C, Lord SP, Petrie M, Oʼconnor SS, Katon W. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013 257(3):390–9. 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed]
- 94.Ruggiero KJ, Davidson TM, Anton MT, Bunnell B, Winkelmann J, Ridings LE, et al. Patient engagement in a technology-enhanced, stepped-care intervention to address the mental health needs of trauma center patients. J Am Coll Surg. 2020;231(2):223–230. doi: 10.1016/j.jamcollsurg.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.deRoon-Cassini TA, Hunt JC, Geier TJ, Warren AM, Ruggiero KJ, Scott K, et al. Screening and treating hospitalized trauma survivors for posttraumatic stress disorder and depression. J Trauma Acute Care Surg. 2019;87(2):440–450. doi: 10.1097/TA.0000000000002370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stone DM, Holland KM, Bartholow B, Crosby AE, Davis S, Wilkins N. Preventing suicide: a technical package of policies, programs, and practices. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2021. Accessed 20 Apr 2021.
- 97.Bhatt A, Wang X, Cheng AL, Morris KL, Beyer L, Chestnut A, et al. Association of changes in Missouri firearm laws with adolescent and young adult suicides by firearms. JAMA Netw Open. 2020;3(11):e2024303. doi: 10.1001/jamanetworkopen.2020.24303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kalesan B, Mobily ME, Keiser O, Fagan JA, Galea S. Firearm legislation and firearm mortality in the USA: a cross-sectional, state-level study. Lancet. 2016;387:1847–1855. doi: 10.1016/S0140-6736(15)01026-0. [DOI] [PubMed] [Google Scholar]
- 99.Raifman J, Larson E, Barry CL, Siegel M, Ulrich M, Knopov A, Galea S. State handgun purchase age minimums in the US and adolescent suicide rates: regression discontinuity and difference-in-differences analyses. BMJ. 2020;22(370):m2436. doi: 10.1136/bmj.m2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McLean RM, Harris P, Cullen J, Maier RV, Yasuda KE, Schwartz BJ, Benjamin GC. Firearm-related injury and death in the United States: a call to action from the nation's leading physician and public health professional organizations. Ann Intern Med. 2019;171(8):573–577. doi: 10.7326/M19-2441. [DOI] [PubMed] [Google Scholar]