Abstract
Background
Respiratory infections among children, particularly community-acquired pneumonia (CAP), is a major disease with a high frequency among outpatient and inpatient visits. The causes of CAP vary depending on individual susceptibility, the epidemiological characteristics of the community, and the season. We performed this study to establish a nationwide surveillance network system and identify the causative agents for CAP and antibiotic resistance in Korean children with CAP.
Methods
The monitoring network was composed of 28 secondary and tertiary medical institutions. Upper and lower respiratory samples were assayed using a culture or polymerase chain reaction (PCR) from August 2018 to May 2020.
Results
A total of 1023 cases were registered in patients with CAP, and PCR of atypical pneumonia pathogens revealed 422 cases of M. pneumoniae (41.3%). Respiratory viruses showed a positivity rate of 65.7% by multiplex PCR test, and human rhinovirus was the most common virus, with 312 cases (30.5%). Two hundred sixty four cases (25.8%) were isolated by culture, including 131 cases of S. aureus (12.8%), 92 cases of S. pneumoniae (9%), and 20 cases of H. influenzae (2%). The cultured, isolated bacteria may be colonized pathogen. The proportion of co-detection was 49.2%. The rate of antibiotic resistance showed similar results as previous reports.
Conclusions
This study will identify the pathogens that cause respiratory infections and analyze the current status of antibiotic resistance to provide scientific evidence for management policies of domestic respiratory infections. Additionally, in preparation for new epidemics, including COVID-19, monitoring respiratory infections in children and adolescents has become more important, and research on this topic should be continuously conducted in the future.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12879-022-07263-z.
Keywords: Pneumonia, Child, Surveillance, Epidemiology
Background
Pneumonia is an infection of the lower airways, and community-acquired pneumonia (CAP) specifically refers to clinical signs and symptoms of pneumonia acquired outside a hospital setting [1]. In the United States, CAP is the most common cause of hospitalization among children, with an annual incidence of 15.7–22.5 hospitalizations per 100,000 children [2, 3]. According to statistics from the Health Insurance Review and Assessment Service, nearly half (44.6%) of the 1.59 million pneumonia patients in 2015 were reported to be children under the age of 10, and in 2018, children under the age of 10 often have respiratory system diseases, which are the most common diseases for outpatient and inpatient visits, with pneumonia ranking second among the causes of inpatient visits [4]. These respiratory diseases are mainly caused by bacterial or viral infections, and treatments should be selected depending on the pathogen that causes them. However, clinical symptoms alone cannot distinguish the pathogens, so they should be assessed via laboratory tests. In most CAPs, empirical treatment is provided in that the causes of pneumonia vary widely depending on individual sensitivity, the dynamics of the community, and seasons. It is difficult to obtain samples for microbiological diagnosis. Thus, epidemiological data on clinical patterns and causes of childhood pneumonia will help care, including determining the direction of treatment [5].
The development of the Haemophilus influenzae type b (Hib) vaccine and protein binding pneumococcal conjugate vaccine (PCV) has rapidly decreased the incidence of Hib pneumonia and pneumococcal pneumonia [6]. Data on changes in the serologic type of S. pneumoniae and antimicrobial susceptibility following the introduction of the pneumococcal vaccine are insufficient. Additionally, the data on pneumonia caused by other bacterial pathogens are insufficient.
Pneumonia by Mycoplasma pneumoniae is also a major infectious illness for children in kindergarten and school age, and it continues to be prevalent every 3 to 4 years [7–9]. The incidence of mycoplasma infection increased in 2007, and the incidence rate soared from 2010 to 2011 [7]. M. pneumoniae is often accompanied by pleural fluid and shows lobar pneumonia, which is difficult to differentiate from bacterial pneumonia by referring to clinical patterns and chest radiologic findings [8]. Recently, macrolide-resistant M. pneumoniae in Korea has been reported, and it is necessary to determine the nationwide status of the disease, the effectiveness of antibiotic treatment, and the degree of resistance.
There have been reports of the distribution of pathogens, epidemic trends, and antibiotic resistance of bacterial pathogens to respiratory infections in adults, but there have been no nationwide reports in children and adolescents in Korea. In particular, CAP in children and adolescents accounts for more than 50% of all cases, the pathogen of pneumonia is different from that of adults, and recent vaccination has resulted in changes in pathogens. For this reason, a nationalized study is needed to analyze the prevalence, epidemic characteristics, and pathogens of pneumonia in children and adolescents. Therefore, the purpose of this study is to establish a monitoring network for CAP among children in connection with community-based cooperative hospitals and the Korea Disease Control and Prevention Agency (KDCA). In addition, we studied the distribution of pathogens, epidemic trends of CAP, and antibiotic usage and resistance of bacterial pathogens.
Methods
Patients and study design
A prospective study was conducted in patients under 18 years old who attended a hospital with a diagnosis of CAP. Patients who fulfilled the selection criteria were studied from August 2018 to May 2019 (first research period) and from August 2019 to June 2020 (second research period). The cooperative hospital monitoring network was established for the second and tertiary hospitals in six metropolitan areas (Seoul, Gyeonggi Province, Chungcheong Province, Gangwon Province, Jeolla Province, Gyeongsang Province). From August 2018 to May 2019, 27 hospitals participated, and from August 2019 to June 2020, 28 hospitals participated. The Korean Childhood Community-Acquired Pneumonia Study Group (KoC-CAPS) was established, and this network represented laboratory monitoring networks where pneumonia data could be collected, managed, and analyzed and information could be shared among participating hospitals (Additional file 1: Fig. S1).
Inclusion criteria
The inclusion criteria were as follows: patients who had a cough or a severe fever as a major symptom, patients diagnosed with pneumonia with a chest X-ray, and patients under 18 years of age who had no history of using antibiotics within 5 days of the visit period.
Exclusion criteria
The exclusion criteria were as follows: patients with an upper respiratory tract infection that was accompanied by rhinitis symptoms such as a runny nose or stuffy nose, patients who had chronic underlying diseases or immune suppressive disease, and patients with a history of antibiotic use within 5 days.
Study participants
For each patient, a questionnaire with clinical and epidemiological features was completed. The questionnaire included the following information: patient information (age, birth date, sex, name of the hospital, specimen type, history of hospitalization, underlying disease, vaccination status, siblings), clinical information (fever, cough, sputum, rhinorrhea, vomiting, sore throat, etc., radiologic findings, vital signs, breathing sound, O2 saturation), and treatment (prescribed antibiotics, hospitalization period, sequelae) (Additional file 2: Table S1).
Collection of samples
Samples were obtained from sputum, nasopharyngeal aspiration, nasopharyngeal swab or bronchoalveolar lavage (BAL). Nasopharyngeal aspirates were obtained within 24 h after enrollment. A suction catheter was used to pass through the nose into the lower part of the pharynx. A total of 2 ml nasopharyngeal aspirates were obtained and sent to a laboratory for analysis within 48 h. A nasopharyngeal swab was obtained by inserting a swab into both nostrils parallel to the palate. A throat swab was obtained from the posterior pharyngeal and tonsillar areas. Sputum or BAL specimens were also collected if possible. Viruses [respiratory syncytial virus (RSV) A and B, influenza virus (IFV) A and B, parainfluenza virus (PIV) 1, 2, 3, and 4, adenovirus (ADV), human rhinovirus (HRV), human metapneumovirus (HMPV), coronavirus (CoV) 229E, NL63, OC43, bocavirus (BoV), and human enterovirus (HEV)] were assessed using the multiplex PCR method. Atypical pneumonia pathogens (M. pneumoniae, Chlamydophila pneumoniae, Legionella pneumophilia, Bordetella pertussis) were identified using polymerase chain reaction (PCR) tests and cultures. Cultures for bacterial pathogens (S. pneumoniae, H. influenzae, Staphylococcus aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa) and antimicrobial susceptibility tests were performed.
The detection of pathogen
A viral pathogen
For multiplex RT-PCR, viral genomic RNA and DNA were extracted from a total volume of 1 µl of the sample by the guanidinium thiocyanate extraction method. The lysis buffer included 500 molecules of the cloned amplified product used as an internal control in each reaction tube and then excluded false-negative results. Three independent multiplex reverse transcription nested RT-PCT assays, able to detect from 1 to 10 copies of viral genomes, were performed. One nested RT-PCR was performed using a specific primer for PIV (1, 2, 3, 4), ADV, HEV, and HMPV, another nested RT-PCR was prepared with specific primers for HRV (A, B, C), CoV (229E, NL63, OC43), and BoV (1, 2, 3, 4), and a third nested RT-PCR was performed using specific primers for RSV (A, B) and IFV (A, B, subtype H1, H3, H1pdm09) by using the Allplex™ Respiratory Panel (Seegene, Seoul, South Korea).
Atypical pneumonia pathogen
Atypical pneumonia pathogens were detected by PCR. Nucleic acid was extracted from a total volume of 1 ml of the sample and purified. The cyclic temperature settings were 94 ℃ 20 s, 58 ℃ 20 s, and 72 ℃ 20 s amplified by 35 cycles, with the last 72 ℃ 7 min. M. pneumoniae, C. pneumoniae, L. pneumophilia and B. pertussis were confirmed by using the Allplex™ PneumoBacter Assay (Seegene, Seoul, South Korea).
A bacterial pathogen
Bacterial pathogens were detected by culture, and cultured pathogens were subjected to antimicrobial susceptibility tests. If the final identification of the bacteria was ambiguous or required accurate identification, we confirmed the results by using VITEK 2 (bioMerieux, Hazelwood, USA) to verify the infection, and additional PCR tests were performed for S. pneumoniae and H. influenzae by using the Allplex™ PneumoBacter Assay (Seegene, Seoul, South Korea).
The susceptibility test of antibiotics
In this study, the antibiotic susceptibility test of isolated bacteria measured the minimum inhibitory concentration (MIC) using a MicroScan® Microbiology System (Dade Behring, Tokyo, Japan). The criteria for judging antibiotic resistance followed the criteria of the Clinical Laboratory Standard Institute (CLSI).
Results
Demographic results
A total of 1023 patients under 18 years old with a diagnosis of CAP were studied. The mean age was 5.0 ± 4.1 years (mean ± standard deviation, range: 1 month–18 years). Most patients were between 1 and 3 years old (310, 30.3%), followed by children between 7 and 11 years old (281, 27.5%), between 4 and 6 years old (210, 20.5%), under 12 months (146, 14.3%), and over 12 years old (75, 7.3%). There was a case in which age entry was omitted. There were 537 males (52.5%) and 486 females (47.5%). Regionally, 360 were reported in Gyeongsang Province, 219 in Chungcheong, 215 in Gyeonggi, 114 in Seoul, 101 in Jeolla, and 14 in Gangwon.
Of the 1023 people, 976 (95.4%) were hospitalized, and 45 (4.4%) were treated in outpatient clinics. There were 2 cases in which hospitalization was unknown. The mean length of hospital stay for the 932 people whose hospitalization period was specified was 6.8 days (range 1–47 days). Specimens were collected from 727 (71.1%) nasopharyngeal aspirate samples, 195 (19.1%) sputum samples, 73 (7.1%) nasopharyngeal swab samples, 12 (0.2%) BAL samples, 8 (0.8%) throat swab samples, and 2 (0.2%) transtracheal aspirate samples. The most frequent symptoms were cough (93.3%), fever (86.1%), sputum (78%), and rhinorrhea (51.1%). The most frequent physical examinations were rale (65%), wheezing (19.5%), decreased aeration (10.5%), and hypoxia (5.2%).
Among the radiological findings of pneumonia, peribronchial infiltration was the most common (44.4%), followed by lobar infiltration (42.8%), interstitial infiltration (11.1%), and pleural effusion (3.8%). There were 212 patients with underlying disease; among them, 79 had an allergic disease, 14 had congenital heart disease, 4 had kidney disease, 4 had endocrine disease, and 2 had cerebrovascular disease. Other accompanying diseases included neurological disorders, Down syndrome, developmental delays, etc. The antibiotic prescription rate was 91.8% (939), and of them, the macrolide prescription rate was the highest (69.6%), followed by cephalosporin (40.8%), and penicillin series (33.2%). All of the penicillin series used were semisynthetic penicillin. There were 84 cases in which antibiotics were not prescribed. The characteristics of the study population are depicted in Table 1.
Table 1.
Demographic and clinical features of the study population
| Mean Age ± SD | 5.0 ± 4.1 yrs | Clinical findings | N (%) | Physical examinations | N (%) |
| Age range (min–max) | 1 mo–18 yrs | Cough | 992 (93.8) | Rale | 688 (65) |
| Age | N (%) | Fever | 911 (86.1) | Wheezing | 206 (19.5) |
| < 12 month | 146 (14.3) | Sputum | 825 (78) | Decreased aeration | 111 (10.5) |
| 1–3 yrs | 310 (30.3) | Rhinorrhea | 541 (51.1) | Hypoxia < 95% | 55 (5.2) |
| 4–6 yrs | 210 (20.5) | Poor oral intake | 137 (12.9) | Chest retraction | 50 (4.7) |
| 7–11 yrs | 281 (27.5) | Chill | 86 (8.1) | Prescribed antibiotics | N (%) |
| ≧ 12 yrs | 75 (7.3) | Sore throat | 86 (8.1) | Macrolide | 654 (69.6) |
| Unknown | 1 (0.1) | Dyspnea | 58 (5.5) | Cephalosporin | 383 (40.8) |
| Total | 1,023 | GI symptom | Penicillin series | 312 (33.2) | |
| Gender | N (%) | Vomiting | 70 (6.6) | Tetracyclin | 59 (6.3) |
| Male | 537 (52.5) | Diarrhea | 37 (3.5) | Quinolone | 39 (4.2) |
| Female | 486 (47.5) | Abdominal pain | 34 (3.2) | Aminoglycoside | 5 (0.5) |
| Place of treatment | N (%) | Myalgia | 36 (3.4) | Vancomycin | 3 (0.3) |
| Hospitalized | 976 (95.4) | Chest pain | 21 (2) | Lincomycin | 3 (0.3) |
| Outpatient clinic | 45 (4.4) | Hoarseness | 17 (1.6) | Total | 939 |
| Species of sample | N (%) | Rash | 11 (1) | ||
| Nasopharyngeal aspirates | 727 (71.1) | Hemoptysis | 5 (0.5) | ||
| Sputum | 195 (19.1) | Chest X-ray finding | N (%) | ||
| Nasopharyngeal swab | 73 (7.1) | Peribronchial infiltration | 470 (44.4) | ||
| Bronchoalveolar lavage | 12 (1.2) | Lobar infiltration | 453 (42.8) | ||
| Throat swab | 8 (0.8) | Interstitial infiltration | 117 (11.1) | ||
| Transtracheal aspirate | 2 (0.2) | Pleural effusion | 40 (3.8) | ||
N number, SD standard deviation, mo months, yrs years, GI gastrointestinal
Respiratory pathogens
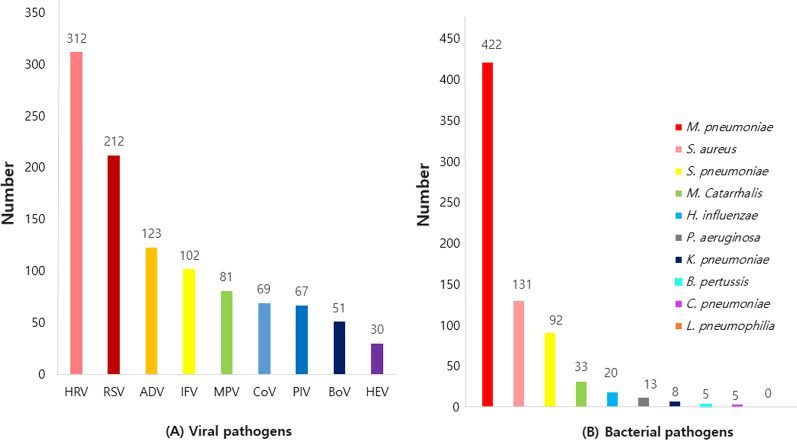
A total of 1023 samples of CAP were tested by virus PCR, and the rate of positivity for respiratory viruses was 65.7%. HRV was highest, with 312 (29.8%), followed by RSV (A + B) 212 (20.3%), ADV 123 (11.8%), IFV (A + B) 102 (9.8%), HMPV 81 (7.7%), CoV (OC43 + NL63 + 2229E) 69 (6.6%), PIV (1 + 2 + 3 + 4) 67 (6.4%), BoV 51 (4.6%), and HEV 30 (2.9%) (Fig. 1A). The frequency order of viruses was slightly different when comparing the results of the first and second research periods. The frequency of virus detection changed in the second period; it was ADV, IFV, CoV, HEV, PIV, HMPV, and BoV in the second period, and it was HMPV, ADV, PIV, BoV, IFV, CoV, and HEV in the first period. The number of detection for each virus detected in the sputum are found in Additional file 2: Table S2. Of the 1023 cases, the atypical pneumonia pathogen was identifiable in 432 cases (42.2%) by PCR and the bacterial pathogen was identifiable in 264 cases (25.8%) by culture. Of the atypical bacterial pathogens, there were 422 cases (97.7%) of M. pneumoniae, five cases (1.2%) of C. pneumoniae, five cases (1.2%) of B. pertussis, and L. pneumophilia was not found. The bacterial pathogens isolated by culture were as follows. There were 131 cases (12.8%) of S. aureus, 92 cases (9%) of S. pneumoniae, 33 cases (3.2%) of Moraxella catarrhalis, 20 cases (2%) of H. influenzae, 13 cases (1.3%) of P. aeruginosa, and 8 cases (0.8%) of K. pneumoniae (Fig. 1B). In particular, the number of detection for each pathogen found in the sputum are in Additional file 2: Tables S3, S4. The number of bacterial pathogens identified by culture in sputum, nasopharyngeal aspirate and nasal swab, etc., respectively are found in Additional file 2: Table S5.
Fig. 1.
The number of detected respiratory pathogens. A Respiratory viral pathogens. B Respiratory bacterial pathogens. HRV Human rhinovirus, RSV Respiratory syncytial virus, IFV Influenza virus, PIV Parainfluenza virus, ADV Adenovirus, HMPV Human metapneumovirus, CoV Coronavirus, BoV Bocavirus, HEV human enterovirus
Annual and seasonal patterns of respiratory pathogens of CAP
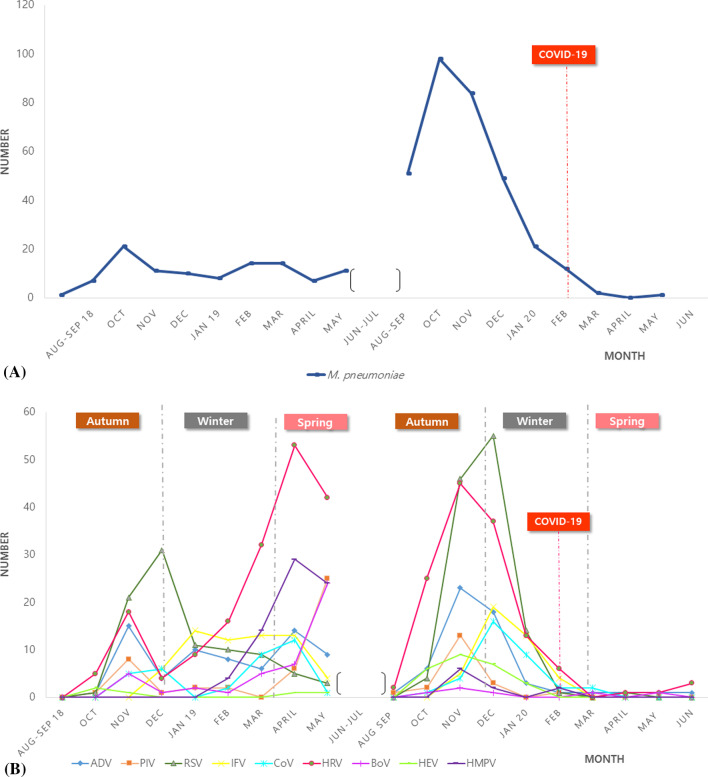
Mycoplasma pneumoniae was the most common bacterial pathogen that showed a surge infection from August 2019 to December 2019. But M. pneumoniae was rarely detected after the COVID-19 outbreak (Fig. 2A). Respiratory viruses showed a seasonal pattern, RSV was detected mostly from November to January, ADV showed a biphasic peak in November and April, HMPV in April and May, HRV a dual peak in the spring and autumn seasons, and BoV in April. Respiratory viruses were rarely detected after the COVID-19 outbreak. Less HRV, ADV, and BoV were detected, but RSV, IFV, PIV, and HMPV were not detected after the COVID-19 outbreak (Fig. 2B).
Fig. 2.
The annual and seasonal patterns of the respiratory pathogen in CAP. A M. pneumoniae, B Respiratory viral pathogens. CAP community-acquired pneumonia, HRV human rhinovirus, RSV Respiratory syncytial virus, IFV Influenza virus, PIV Parainfluenza virus, ADV Adenovirus, HMPV human metapneumovirus, CoV Coronavirus, BoV Bocavirus, HEV human enterovirus
Results of respiratory pathogens according to age
Respiratory viruses were the most common pathogen of CAP under the age of 3 years. The rates of viruses and M. pneumoniae were similar at the ages of 4–6 years. From 7 years of age, bacteria were predominant for CAP; M. pneumoniae was the most common bacterial pathogen. According to the positive rate of M. pneumoniae by age, the positive rate was highest at ages 7 to 11 (179 cases), followed by ages 4 to 6 (121 cases), ages 1 to 3 (56 cases), ages 12 years and older (48 cases), and at less than 12 months (14 cases). Five cases of C. pneumoniae were detected at 7–11 years of age. Five cases of B. pertussis were detected at the ages of 1–3 in three cases and 7–11 in two cases. When comparing the virus detection rate by age, the positive rate was the highest among those under 12 months, followed by those aged 1–3, 4–6, 7–11, and 12 or older (Table 2).
Table 2.
Results of isolated respiratory pathogen according to age
| < 12 mo | 1–3 yrs | 4–6 yrs | 7–11 yrs | ≧ 12 yrs | UK | Total | |
|---|---|---|---|---|---|---|---|
| N of sample | 147 | 309 | 215 | 270 | 73 | 5 | 1023 |
| Viruses | 127 (86.4) | 262 (84.8) | 136 (63.3) | 111 (41.1) | 24 (30.8) | 1 | 661 (64.5) |
| M. pneumoniae | 14 (9.5) | 56 (18.1) | 121 (56.3) | 179 (66.3) | 48 (65.8) | 3 | 422 (41.3) |
| S. aureus | 26 (17.7) | 24 (7.8) | 24 (11.1) | 42 (15.6) | 14 (19.2) | 1 | 131 (12.8) |
| S. pneumoniae | 24 (16.3) | 45 (14.6) | 12 (5.6) | 7 (2.6) | 4 (5.5) | 92 (9) | |
| H. influenzae | 1 (0.7) | 11 (3.6) | 4 (1.9) | 4 (1.5) | 20 (2) | ||
| P. aeruginosa | 3 (2) | 3 (1) | 3 (1.4) | 3 (1.1) | 1 (1.4) | 13 (1.3) | |
| K. pneumoniae | 3 (2) | 1 (0.3) | 2 (0.9) | 2 (0.7) | 8 (0.8) | ||
| C. pneumoniae | 5 (1.9) | 5 (0.5) | |||||
| B. pertussis | 2 (1.4) | 1 (0.3) | 1 (0.5) | 1 (0.4) | 5 (0.5) |
N number, mo months, yrs years, UK unknown
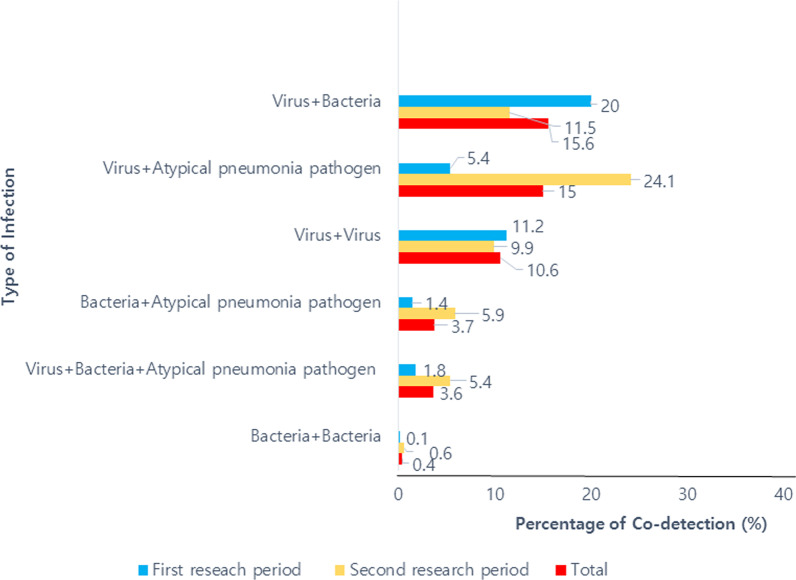
Results of co-detection
The proportion of co-detection was 49.2%, and the overall rate of co-detection was highest in the virus/bacteria (15.6%), followed by virus/atypical pneumonia pathogens (15%) and virus/virus (10.6%). We analyzed the rate of co-detection in each study period. In the first study period, the co-detection of virus/bacteria (20%) was the highest; however, in the second study period, when mycoplasma pneumonia epidemics occurred, the co-detection of virus/atypical pneumonia pathogens was highest (24.1%) (Fig. 3).
Fig. 3.
The percentage of co-detection in CAP. CAP community-acquired pneumonia
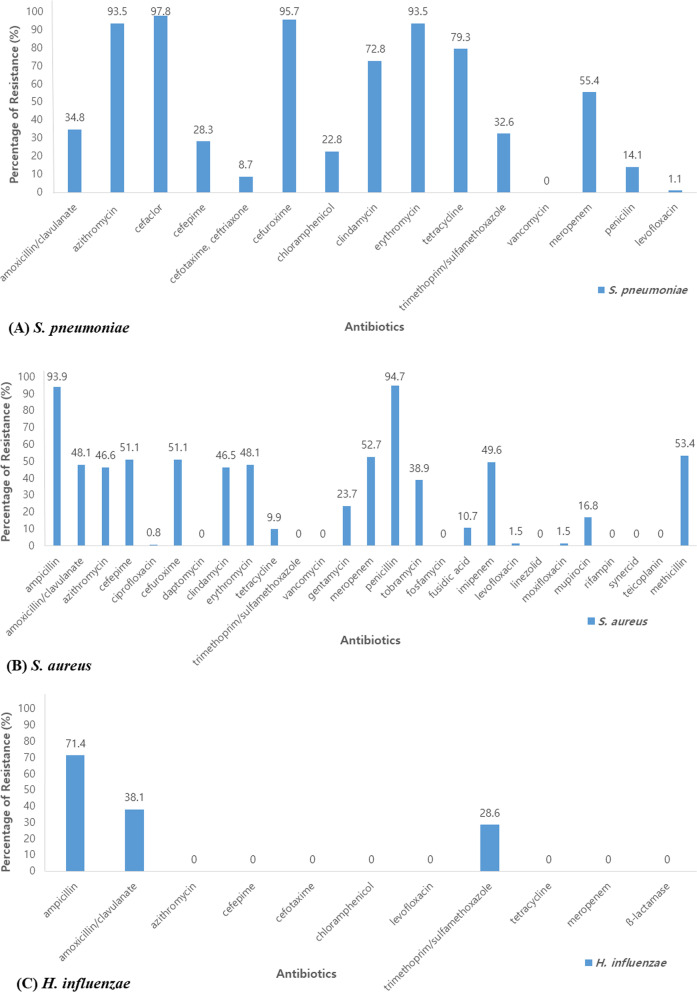
Resistance to antibiotics
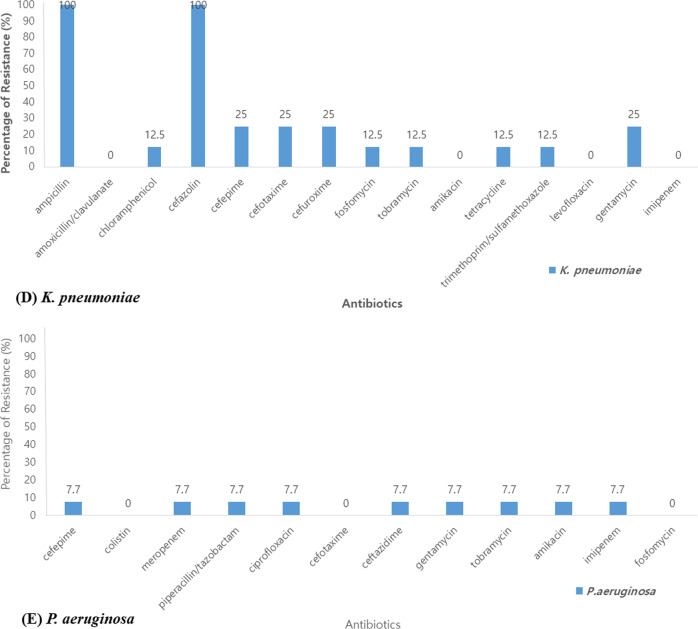
We assessed the antibiotic resistance rate of bacteria. Among a total of 92 cases of S. pneumoniae, 14.1% were resistant to penicillin, 8.7% to cefotaxime, 93.5% to erythromycin and azithromycin, 79.3% to tetracycline, and 1.1% to levofloxacin. Of 21 cases of H. influenzae, 71.4% were resistant to ampicillin, 38.1% to amoxicillin/clavulanate, and no strains were resistant to cefotaxime and tetracycline. Of the 131 cases of S. aureus, 94.7% and 53.4% were resistant to penicillin and methicillin, respectively, 48.1% to amoxicillin/clavulanate, 46.6% to azithromycin, 1.5% to levofloxacin, 9.9% to tetracycline, and 46.5% to clindamycin. No strains were resistant to trimethoprim/sulfamethoxazole and rifampin. Of the 8 cases of K. pneumoniae, 25% were resistant to cefotaxime, gentamycin and cefepime. No strains were resistant to amoxicillin/clavulanate, levofloxacin and imipenem. Of 13 cases of P. aeruginosa, 7.7% were resistant to cefepime, piperacillin/tazobactam, ciprofloxacin, ceftazidime and amikacin. No strains were resistant to colistin (Fig. 4).
Fig. 4.
The percentage of resistance in antibiotics. A S. pneumoniae, B S. aureus, C H. influenzae, D K. pneumoniae, E P. aeruginosa
Discussion
Most studies about the causative agents of CAP in children are limited by the difficulty of obtaining adequate specimens. This study is meaningful because it was the first prospective extensive study investigating respiratory pathogens in children with CAP in Korea. In this study, the rate of pathogen detection in children with CAP was 70.5%. However, it could not be confirmed whether the bacterial culture results were the causative pathogen of CAP, and it is highly likely that they were colonized. There are studies about the causative agents of CAP in many countries. In the Taiwanese study, at least one pathogen was identified in 68.3% of children with CAP [10], and in the Chinese study, the causative pathogen was identified in 70.1% of the hospitalized children with CAP at one hospital [11]. In a 3-year US-based study, the causative pathogen was identified in 81% of patients under the age of 18 hospitalized with CAP [2]. In a study conducted in Finland, the causative pathogen was detected in 85% of hospitalized children with pneumonia [12]. The difference in detection rate in each country seems to be due to the difference in sample types and methods. The sample types collected in this study were nasopharyngeal swabs/aspirates and sputum, and the causative pathogens were identified through PCR and cultures. To detect viruses, the same method (PCR test) is used through nasopharyngeal swabs/aspirates in other countries. However, unlike in this study, most tests for bacterial detection were conducted through blood and pleural fluid cultures or blood PCR tests. As a result, it is thought that the detection rate of the pathogen in each study is different.
There are few studies about the causative agent of children with CAP in Korea. In 2009, respiratory viruses were identified in 49.6% of severe lower respiratory tract infections in children [13]. However, unlike in our study, there were no data for bacterial infections. Recently, there was also a study on the seasonal pattern in etiologic viruses and M. pneumoniae in children hospitalized with CAP in Korea; it showed that M. pneumoniae was the most commonly identified pathogen [14]. It was noticeable that bacterial pathogens as well as viruses were also tested. In general, the common bacterial pathogens of CAP in children are S. pneumoniae, H. influenzae type b, and S. aureus. To differentiate true pathogens from colonization in CAP, cultures from blood/pleural fluid samples or urinary S. pneumoniae antigen tests using immunochromatography are better than nasopharyngeal samples [1, 12]. In the current study, we did not use this method; we used bacterial cultures or PCR from nasopharyngeal swabs/aspirates. The detection rate of bacteria from blood cultures in CAP is very low, and pleural cultures are limited to only children with parapneumonic effusion. Urinary S. pneumoniae antigen tests can be positive in children if S. pneumoniae is colonized in the nasopharynx. S. pneumoniae and H. influenzae are common flora in the upper respiratory tract, and up to two-thirds of children younger than 5 years are colonized with common bacterial pathogens in the upper respiratory tract. The identification of bacteria from the upper respiratory tract does not always determine the pathogen of CAP; therefore, physicians should consider clinical relevance for ascertaining the bacterial etiologies of pneumonia [15]. It is difficult to identify bacteria that cause bacterial pneumonia, because the introduction of the National Immunization Program (NIP) vaccine has reduced bacterial pneumonia and invasive bacterial infection. Although the results of bacterial culture in the upper respiratory tract sample in children are highly likely to be colonized, there are studies that suggest the association between bacteria colonizing the upper respiratory tract and lower respiratory tract infection in young children [16]. Also, analysis of antibiotic resistance and serotype of bacteria detected in the upper respiratory tract can obtain important information that can be used clinically. Therefore, the present study that reported these results is meaningful.
Over the past 20 years, more than 20 cases of B. pertussis have been reported every year in Korea. During 2001–2007, there was an average of 11.3 cases of B. pertussis per year [17], and a gradual increase from 2009 to 2012 was reported [18]. In particular, 24.5% of Korean adolescents and adults with chronic cough were positive for B. pertussis in 2015 [19]. Due to the lack of data on B. pertussis in pediatric patients in Korea, it was important to obtain epidemiological data on B. pertussis through the results of the surveillance network study. In this study, B. pertussis was isolated from five children, which was less than we expected. All cases were observed between January and April, and two of the patients were younger than 3 months old, while the other three were aged 1, 6 and 9 years old. Due to the NIP by the Korean government, the incidence of B. pertussis is low in children, but a gradual increase in adolescents and adults requires the need for a booster injection. Based on these data, it will be necessary to accumulate various epidemiological data on pertussis through the construction of a continuous monitoring network in children and adolescents in Korea.
The common pathogen of CAP in adults was S. pneumoniae in a prospective multicenter study in Korea, and in other study, S. pneumoniae was most frequent pathogen, atypical pathogens such as M. pneumoniae, and C. pneumoniae were the second most common pathogens [20, 21]. Unlike with adults, the most common cause of CAP in children varies according to age. Several studies have previously reported that respiratory viruses are the leading cause of CAP, which can be detected in more than 50% of the cases [22, 23]. However, these results may vary by study and age group. Similar to our research, in a study of Peru patients under the age of 18 who were hospitalized for pneumonia, M. pneumoniae was more frequently detected than respiratory viruses [24]. Additionally, in the Taiwanese study, S. pneumoniae was the most common pathogen, and the detection rate of pneumococcus was much higher than that in our study [10]. This may be attributed to relatively lower vaccination rates in Taiwan. Vaccination programs for causative pathogens of pneumonia in Korea are as follows. In 2003, a 7-valent pneumococcal protein-binding vaccine (PCV) was first introduced in Korea, and in June 2010, a 10-valent and a 13-valent PCV were introduced. Currently, Korean government has started pneumococcal vaccination for every infants at 2, 4, 6, and 15 months of age as NIP since 2014, which may rapidly decrease the frequency of S. pneumoniae pneumonia. H. influenzae type b vaccine is also provided as a NIP since 2013. The Hib vaccine is also given at 2, 4, and 6 months of age as a primary vaccinations and at 12–15 months of age as a booster shot. Pertussis vaccination is also included in a NIP as Diphtheria–tetanus–acellular pertussis vaccine (DTaP) or booster tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap). After three primary vaccinations at 2, 4, and 6 months of age, booster vaccinations are performed at 15–18 months old and 4–6 years old, respectively. In our study, 39 (3.8%) patients were not vaccinated, 86 (8.4%) were unsure whether they were vaccinated. And the rest of subjects (87.8%) were all vaccinated.
The rate of M. pneumoniae surged from the fall of 2019, which abruptly ended after the COVID-19 outbreak in 2020. M. pneumoniae is a major pathogen of CAP in children and adolescents [9]. Recent studies showed that mycoplasma was responsible for approximately 20–30% of CAP at the age of 3 to 4 years, and during the epidemic M. pneumoniae infected even children at 2 years old [5, 9, 25]. M. pneumoniae pneumonia epidemics occur every 3 to 5 years [9, 26, 27]. It was reported that epidemics of M. pneumoniae pneumonia occurred in 2007, 2011, and 2015 [28, 29]. According to the trend cycle, the results of this study confirmed that the mycoplasma epidemic had been refloating in 2019. Interestingly, the rate of M. pneumoniae decreased abruptly after COVID-19. This may be attributed to social distancing, mask-wearing, hand washing, and online schooling.
The seasonal difference in detection rates for viruses is consistent with the existing data. We found that the respiratory viruses were composed of major pathogens for CAP in young children under the age of 3 years. It is known that viruses may cause pneumonia, either directly or by rendering the host more susceptible to bacterial infection [11]. In studies of CAP in children, mixed infections were identified in 34–41% of the children with CAP, and mixed viral-bacterial infection showed the highest rate [11, 30–32]. On the other hand, two US studies reported a lower rate (23–26%) of mixed infection [2, 31]. In this study, the proportion of co-detection was 49.2%, which was higher than in previous studies. The co-detection rate of viruses, bacteria, and atypical bacterial pathogens was 3.6%. It is assumed that the differences in co-detection rate and pattern of co-detection may be related to seasonal, geographical, and racial factors. It may also vary depending on the type of sample or laboratory testing method.
Although viruses are major cause of childhood CAP, a majority of children with pneumonia receive antibiotics. Empiric use of antibiotics remains a cornerstone of treatment in the absence of results in the causative agents of pneumonia. In the U.S. guidelines, amoxicillin is used in previously healthy outpatients who have been properly vaccinated if they suspect mild or moderate bacterial pneumonia. It is recommended to use macrolides if CAP caused by an atypical pneumonia pathogen is suspected [33]. In our study, the empiric antibiotic prescription rate was high, and of them, the macrolide prescription rate was the highest. The high macrolide prescription rate may be attributable to the epidemic of M. pneumoniae in 2019.
The rate of antibiotic resistance in this study showed similar results as previous reports. Penicillin sensitivity of pneumococcus in the study of adult pneumonia was 42.9% in 2001 but 100% in 2010 [20, 21]. According to the treatment guidelines of CAP, S. pneumoniae has a low resistance rate for penicillin and quinolone and a relatively high resistance rate for some cephalosporin and macrolide [34]. Our results also showed high resistance rates for second-generation cephalosporin and macrolide, while low resistance rates for the third-generation cephalosporin, penicillin, and quinolone, which is similar to what was previously reported. In addition, the results of the antibiotic resistance of H. influenzae, P. aeruginosa, K. pneumoniae, and S. aureus were also confirmed to be similar to the 2017 National Antibacterial Resistance Survey Report [35]. These data can be helpful in forming the basis of empiric antibiotic therapy in a child with CAP.
Study limitations
There were some limitations of this study. First, we could not differentiate true pathogens from normal flora, because we mostly collected samples from the upper respiratory tract. Due to the difficulty in collecting sputum from the lower respiratory tract in young children, this may remain a limitation in children. Second, even though this was a nationwide multicenter study, the number of samples was relatively lower than expected, especially in the outpatient clinic. The number of samples decreased from February 2000. This was the beginning of the COVID-19 epidemic, which led to a decrease in respiratory infections, including in children and adolescents, as well as adults, and the disappearance of respiratory pathogens. In particular, since February 2020, the number of pneumonia patients has decreased sharply, due to restrictions on group activities, as well as high-intensity social distancing, the use of masks, and hand washing. Additionally, the indefinite postponement of openings at kindergarten and schools and the prevalence of homeschooling has also been an important factor in the decrease in infection. Third, laboratory results such as white blood cell count or C-reactive protein were not investigated. In the future, it is necessary to match pathogens with clinical symptoms.
Conclusions
This study established a surveillance network for monitoring respiratory infections in Korean children. This research provided scientific evidence of policies for managing pneumonia in children and adolescents in Korea by identifying trends in the prevalence of pathogens in children and adolescents with CAP. It will also contribute to the analysis of antibiotic resistance status for bacteria and proper treatment guidelines for children’s respiratory infections in Korea. In addition, this nationwide network system can help to search for a novel pathogen and monitor new respiratory infections such as COVID-19 and provide early national strategies in preparation for a new epidemic.
Supplementary Information
Additional file 1: Figure S1. The Korean Childhood Community-Acquired Pneumonia Study Group; KoC-CAPS.
Additional file 2: Table S1. Community acquired pneumonia—Clinical information records. Table S2. The PCR results of identified viral pathogen in the sputum. Table S3. The PCR results of identified bacterial pathogen in the sputum. Table S4. The culture results of identified bacterial pathogen in the sputum. Table S5. The number of bacterial pathogens identified by culture in NPA, sputum, nasopharyngeal swab, etc.
Acknowledgements
The authors would like to thank the members of the Pneumonia and Respiratory Disease Study Group of the Korean Academy of Pediatric Allergy and Respiratory Disease for carrying out the review.
Abbreviations
- CAP
Community-acquired pneumonia
- KDCA
Korea Disease Control and Prevention Agency
- PCR
Polymerase chain reaction
- MIC
Minimum inhibitory concentration
- BAL
Bronchoalveolar lavage
- HRV
Human rhinovirus
- RSV
Respiratory syncytial virus
- IFV
Influenza virus
- PIV
Parainfluenza virus
- ADV
Adenovirus
- HMPV
Human metapneumovirus
- CoV
Coronavirus
- BoV
Bocavirus
- HEV
Human enterovirus
- Hib
Hemophilus influenzae Type b
- PCV
Pneumococcal conjugate vaccine
- N
Number
- SD
Standard deviation
- mo
Months
- yrs
Years
- DTaP
Diphtheria–tetanus–acellular pertussis vaccine
- Td
Adult type diphtheria and tetanus toxoid vaccine
- Tdap
Booster tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine
- NIP
National immunization program
Authors’ contributions
JYS and EHC designed the conceptualization and experiments. EJR, MHL, JYL, HBK, YMA, JKK, HYK, SSJ, MJK, EKK, EAY, SJL, YP, JHS, EL, ESY, KSP, MYS, HLC, YYJ, BSC, JAJ, STY, MSS, JTK, BSK, YHH, SII, HJY, MYH, HYY, HMC, HYK, YHA, SJY and EHC carried out the investigation. EJR, MHL and ESL performed data curation. EJR wrote the main manuscript text. EJR, MHL, and ESL analyzed and interpreted the patient data. KJH, DHK, and SUJ performed analysis and microbiologic detection. EJR, EHC, MHL, and JYS approved the final manuscript. All authors read and approved the final manuscript.
Funding
This research was supported by a grant from the Korea Disease Control and Prevention Agency, Republic of Korea (Grant Number: 4800-4821-304).
This fund provides financial support in the investigation, design of the study, data collection, data analysis, and interpretation of data.
Availability of data and materials
The data were collected through the surveillance system of the Korean Childhood Community Acquired Pneumonia Study Group of the Korean Academy of Pediatric Allergy and Respiratory Disease. Data are available from the corresponding authors upon reasonable request and with permission of the Korean Academy of Pediatric Allergy and Respiratory Disease.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board and Ethics Committee of Chungnam National University Hospital. (IRB No 2019-07-037) The parents of all study participants gave written informed consent before study enrollment. All methods were performed in accordance with the relevant guidelines and regulations.
Consent of publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Eui Jeong Roh and Mi-Hee Lee contributed equally to this work and should be considered co-first authors
Jung Yeon Shim and Eun Hee Chung contributed equally to this work and should be considered co-corresponding authors
Contributor Information
Jung Yeon Shim, Email: jy7.shim@samsung.com.
Eun Hee Chung, Email: ehchung@cnu.ac.kr.
References
- 1.Katz SE, Williams DJ. Pediatric community-acquired pneumonia in the United States: changing epidemiology, diagnostic and therapeutic challenges, and areas for future research. Infect Dis Clin N Am. 2018;32:47–63. doi: 10.1016/j.idc.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee GE, Lorch SA, Sheffler-Collins S, Kronman MP, Shah SS. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126:204–213. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Insurance Review and Assessment Service in Korea. https://opendata.hira.or.kr/op/opc/olapJdgeChargeInfo.do. Accessed 28 Dec 2021.
- 5.Lee CH, Won YK, Roh EJ, Suh DI, Chung EH. A nationwide study of children and adolescents with pneumonia who visited emergency department in South Korea in 2012. Korean J Pediatr. 2016;59:132–138. doi: 10.3345/kjp.2016.59.3.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black SB, Shinefield HR, Ling S, Hansen J, Fireman B, Spring D, et al. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J. 2002;21:810–815. doi: 10.1097/00006454-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Kim J, Seo H, Yoo E, Park S, Yoon S, Jung H, et al. Mycoplasma pneumoniae pneumonia in Korean children, from 1979 to 2006-a meta-analysis. Korean J Pediatr. 2009;52:315–323. doi: 10.3345/kjp.2009.52.3.315. [DOI] [Google Scholar]
- 8.Youn YS, Lee KY. Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2012;55:42–47. doi: 10.3345/kjp.2012.55.2.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eun BW, Kim NH, Choi EH, Lee HJ. Mycoplasma pneumoniae in Korean children: the epidemiology of pneumonia over an 18-year period. J Infect. 2008;56:326–331. doi: 10.1016/j.jinf.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Chi H, Huang YC, Liu CC, Chang KY, Huang YC, Lin HC, et al. Characteristics and etiology of hospitalized pediatric community-acquired pneumonia in Taiwan. J Formos Med Assoc. 2020;119:1490–1499. doi: 10.1016/j.jfma.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang W, Wu M, Zhou J, Wang Y, Hao C, Ji W, et al. Etiologic spectrum and occurrence of coinfections in children hospitalized with community-acquired pneumonia. BMC Infect Dis. 2017;17:787. doi: 10.1186/s12879-017-2891-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Juvén T, Mertsola J, Waris M, Leinonen M, Meurman O, Roivainen M, et al. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19:293–298. doi: 10.1097/00006454-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Chun JK, Lee JH, Kim HS, Cheong HM, Kim KS, Kang C, et al. Establishing a surveillance network for severe lower respiratory tract infections in Korean infants and young children. Eur J Clin Microbiol Infect Dis. 2009;28:841–844. doi: 10.1007/s10096-009-0701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee E, Kim CH, Lee YJ, Kim HB, Kim BS, Kim HY, et al. Annual and seasonal patterns in etiologies of pediatric community-acquired pneumonia due to respiratory viruses and mycoplasma pneumoniae requiring hospitalization in South Korea. BMC Infect Dis. 2020;20:132. doi: 10.1186/s12879-020-4810-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdullahi O, Nyiro J, Lewa P, Slack M, Scott JA. The descriptive epidemiology of streptococcus pneumoniae and haemophilus influenzae nasopharyngeal carriage in children and adults in Kilifi district, Kenya. Pediatr Infect Dis J. 2008;27:59–64. doi: 10.1097/INF.0b013e31814da70c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Claassen-Weitz S, Lim KY, Mullally C, Zar HJ, Nicol MP. The association between bacteria colonizing the upper respiratory tract and lower respiratory tract infection in young children: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27:1262–1270. doi: 10.1016/j.cmi.2021.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The 5th edition of the epidemiology and management of infectious diseases subject to vaccination in April 2017. Korea Centers for Disease Control and Prevention. http://nip.kdca.go.kr/irgd/reference.do?service=getGuideView&strNum=1248&GUISEQNUM=124. Accessed 28 Dec 2021.
- 18.Han YI, Choi JY, Lee H, Lee T-J. Active surveillance of pertussis in infants under 6 months of age: a single center experience from 2011 to 2013. Korean J Pediatr Infect Dis. 2014;21:114–120. doi: 10.14776/kjpid.2014.21.2.114. [DOI] [Google Scholar]
- 19.Lee SY, Han SB, Kang JH, Kim JS. Pertussis prevalence in Korean adolescents and adults with persistent cough. J Korean Med Sci. 2015;30:988–990. doi: 10.3346/jkms.2015.30.7.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woo JH, Kang JM, Kim Y, Shin WS, Ryu JH, Choi J. A prospective multicenter study of community-acquired pneumonia in adults with emphasis on bacterial etiology. Korean J Infect Dis. 2001;33:1–7. [Google Scholar]
- 21.Chong YP, Jung K-S, Lee KH, Kim M-N, Moon SM, Park S, et al. The bacterial etiology of community-acquired pneumonia in Korea: a nationwide prospective multicenter study. Infect Chemother. 2010;42:397–403. doi: 10.3947/ic.2010.42.6.397. [DOI] [Google Scholar]
- 22.Ygreda JP, Pérez FL, Galarza RR, Da Fieno JT, Moreno VS, Sánchez CC, et al. Etiology of community acquired pneumonia in children 2–59 months old in two ecologically different communities from Peru. Arch Argent Pediatr. 2010;108:516–523. doi: 10.1590/S0325-00752010000600007. [DOI] [PubMed] [Google Scholar]
- 23.Stuckey Schrock K, Hayes BL, Gerog C. Community-acquired pneumonia in children. Am Farm Phys. 2012;86:661–667. [PubMed] [Google Scholar]
- 24.Del Valle-Mendoza J, Silva-Caso W, Cornejo-Tapia A, Orellana-Peralta F, Verne E, Ugarte C, et al. Molecular etiological profile of atypical bacterial pathogens, viruses and coinfections among infants and children with community acquired pneumonia admitted to a national hospital in Lima, Peru. BMC Res Notes. 2017;10:688. doi: 10.1186/s13104-017-3000-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim EK, Youn YS, Rhim JW, Shin MS, Kang JH, Lee KY. Epidemiological comparison of three mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J Pediatr. 2015;58:172–177. doi: 10.3345/kjp.2015.58.5.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guđrún S, Hauksdóttir TJ. Seroepidemiology of mycoplasma pneumoniae infections in Iceland 1987–96. Scand J Infect Dis. 1998;30:177–180. doi: 10.1080/003655498750003591. [DOI] [PubMed] [Google Scholar]
- 27.Foy HM. Infections caused by mycoplasma pneumoniae and possible carrier state in different populations of patients. Clin Infect Dis. 1993;17:S37–46. doi: 10.1093/clinids/17.Supplement_1.S37. [DOI] [PubMed] [Google Scholar]
- 28.Kim JH, Kim JY, Yoo CH, Seo WH, Yoo Y, Song DJ, et al. Macrolide resistance and its impacts on M. pneumoniae pneumonia in children: comparison of two recent epidemics in Korea. Allergy Asthma Immunol Res. 2017;9:340–346. doi: 10.4168/aair.2017.9.4.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wy HH, Min DH, Kim DS, Park MS, Shim JW, Jung HL, et al. Clinical characteristics of mycoplasma pneumoniae pneumonia in Korean children during the recent 3 epidemics. Allergy Asthma Respir Dis. 2017;5:8–14. doi: 10.4168/aard.2017.5.1.8. [DOI] [Google Scholar]
- 30.Chen CJ, Lin PY, Tsai MH, Huang CG, Tsao KC, Wong KS, et al. Etiology of community-acquired pneumonia in hospitalized children in northern Taiwan. Pediatr Infect Dis J. 2012;31:e196–201. doi: 10.1097/INF.0b013e31826eb5a7. [DOI] [PubMed] [Google Scholar]
- 31.Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy LB, Ziegler T, et al. Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics. 2004;113:701–707. doi: 10.1542/peds.113.4.701. [DOI] [PubMed] [Google Scholar]
- 32.Tsolia MN, Psarras S, Bossios A, Audi H, Paldanius M, Gourgiotis D, et al. Etiology of community-acquired pneumonia in hospitalized school-age children: evidence for high prevalence of viral infections. Clin Infect Dis. 2004;39:681–686. doi: 10.1086/422996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the pediatric infectious diseases society and the infectious diseases society of America. Clin Infect Dis. 2011;53:e25–76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song JH, Jung KS. Treatment guideline for community-acquired pneumonia in Korea: an evidence-based approach to appropriate antimicrobial therapy. J Korean Med Assoc. 2010;53:20–42. doi: 10.5124/jkma.2010.53.1.20. [DOI] [Google Scholar]
- 35.Kim JW, Bae SM, Lee SY, Yoo JS. Trends of antimicrobial resistance rates of major clinical pathogens isolated from general hospitals in Korea in 2016–2019: results from Kor-GLASS. Korea Disease Control and Prevention Agency. http://www.kdca.go.kr/board/board.es?mid=a20602010000&bid=0034&list_no=713902&act=view. Accessed 28 Dec 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. The Korean Childhood Community-Acquired Pneumonia Study Group; KoC-CAPS.
Additional file 2: Table S1. Community acquired pneumonia—Clinical information records. Table S2. The PCR results of identified viral pathogen in the sputum. Table S3. The PCR results of identified bacterial pathogen in the sputum. Table S4. The culture results of identified bacterial pathogen in the sputum. Table S5. The number of bacterial pathogens identified by culture in NPA, sputum, nasopharyngeal swab, etc.
Data Availability Statement
The data were collected through the surveillance system of the Korean Childhood Community Acquired Pneumonia Study Group of the Korean Academy of Pediatric Allergy and Respiratory Disease. Data are available from the corresponding authors upon reasonable request and with permission of the Korean Academy of Pediatric Allergy and Respiratory Disease.