Abstract
Background
School districts across the world have been grappling with how to keep their schools open, students healthy, and prevent the spread of viruses in their communities.
Objective
The aims of this study included assessing both (1) the effectiveness of enhanced classroom cleaning and disinfecting protocol on surface biocontamination and (2) the associations between surface biocontamination and student absence due to illnesses.
Methods
Cleaning effectiveness was assessed using quantitative adenosine triphosphate (ATP) measurements during a 10-week study period in a sample of 34 public schools (15,814 students), of a district located in the Western US. The schools were randomly assigned to 17 intervention schools implementing enhanced cleaning and disinfecting protocol and 17 control schools cleaning as usual. General estimating equations (GEEs) were used for modeling associations between ATP levels and weekly aggregates of student absences due to respiratory and gastrointestinal illnesses, which were recorded by the schools according to district wide protocol.
Results
The weekly average ATP levels on logarithmic scale were 5.02 (SD 0.53) and 5.26 (SD 0.48) in the intervention and control schools, respectively, where the difference is statistically significant (p < 0.001). The probability of weekly absence due to gastrointestinal illness was significantly associated with ATP levels (parameter estimate 1.16, 95% CI 1.01–1.34, per unit (log) increase of weekly average ATP), where the model accounts for student level, gender, ethnic group, and socioeconomic status as well as for school level attendance, total absence ratio, and ventilation adequacy in classrooms. Associations were not found between ATP levels and weekly probability of any absence, or absence due to respiratory illness.
Significance
Enhanced cleaning resulted in a significantly lower level of biocontamination on desktops in the intervention group. In addition, a statistically significant association was established between ATP levels on classroom desks and probability of absence due to gastrointestinal illness.
Impact
We found that enhanced cleaning protocol, including bi-weekly cleaning of classroom desks, as well as training of custodians and teachers, monitoring of effectiveness, and feedback, yielded a moderate but statistically significantly lower level of biocontamination on desktops, indicated by quantitative ATP monitoring. Within the range of weekly average desktop ATP levels observed, the probability of reported absence due to gastrointestinal illness is estimated to increase from 0.021 to 0.026. Based on the results, enhanced surface cleaning and monitoring its effectiveness is a possible district, state, or even national level policy to support healthy school environments.
Keywords: Adenosine triphosphate, Disease transmission, Disinfection, Hygiene, Infectious, Schools
Introduction
Exposures to pollutants in schools can have considerable effects on millions of children. However, most previous studies in this arena have cross-sectional designs or have been case studies utilizing school-level data on absenteeism and/or performance. In particular, there are limited prospective studies designed to evaluate the role of IEQ on student health.
One study conducted in the Southwestern United States indicated that inadequate ventilation was associated with visits to school nurses due to respiratory symptoms, and viable bacteria measured from high contact surfaces was associated with nurse visits due to gastrointestinal symptoms [1]. Also, other studies have indicated that enhanced student health and performance can be realized through improved classroom conditions such as adequate ventilation, thermal comfort, and hygiene [2, 3]. Yet, to our knowledge there are no large-scale intervention studies with longitudinal illness absence data juxtaposed to quantitative classroom environmental monitoring.
In the current scientific literature, also information about illness absence from schools is sparse. Many studies on IEQ factors have looked at illness absence in general and absence caused by respiratory infections, but incidence of different types of illnesses causing absence from schools are not well known [4, 5]. There appears to be significant seasonal variation in illness absences, leading to the assumption that a large part of illness absence is caused by influenza and other communicable diseases. In fact, one hypothesis for influenza seasonality focuses on behavior, either through more time spent indoors where contacts are closer or aggregation of susceptible children in schools [6]. Thus, it is important to study whether improving IEQ in schools, for example by enhanced hygiene, could reduce disproportionate health burdens across school communities.
Surface associated fungi, allergens, bacteria, and viruses are components of the indoor microbiome that commonly impact humans in the built environment. Important sources of microbes on surfaces include tracked in dust, shed from humans, settled airborne microbes and microbial growth on building materials [7–9]. Inadequate cleaning leads to accumulation of dust and non-visible ecological niches, which can promote the persistence of biological contaminants, and the resuspension of microbes from flooring and other surfaces is a significant source of exposure to these microbes [10–12]. Therefore, it is advised that schools should encourage routine surface cleaning [13]. However, large scale studies investigating school level differences in this context, as well as standardized methodologies to do so are lacking.
Adenosine triphosphate (ATP) is a measure of biological activity used as a marker for the pollutant loads of biological origin and overall cleanliness. After cleaning and a drop in active biomass, there is a corresponding decrease in ATP, where the amount of ATP measured is expressed in relative light units. Therefore, ATP testing may have a role in providing reassurance that cleaning regimes are being carried out satisfactorily [14]. Correlations have also been noted in recent studies, finding ATP readings indicative of surface associated bacterial, fungal, and human cell levels on desktops [7].
A survey conducted by Shaughnessy et al. established typical ranges for ATP readings in school environments both before and after cleaning [15]. It is important to note that the baseline ATP metric developed for residual surface contamination in schools coming from the study is the foundation for the Worldwide Cleaning Industry Association ISSA Clean Standard for K-12 [16]. The standard provides schools with a tool that will help them measure and monitor the effectiveness of the cleaning processes at their facilities. The significance being that ATP is the first research-based, easy to use indicator of cleaning effectiveness in school settings. However, further studies are needed when it comes to discerning to the effects of cleanliness on students’ health.
To be more effective, school communities need research-based recommendations based on clear endpoints, such as reduced illness absence. Some fundamental questions leading to this study included: (1) Can a concerted school custodial effort, providing twice-a-week desktop cleaning, be reasonably sustained? (2) Will such an effort reveal a significant reduction in desktop contamination based on ATP monitoring? 3) Is cleaning effectiveness associated with illness absence? The specific objectives of this study were: (1) to implement and assess the effectiveness of enhanced desktop cleaning and disinfecting by custodians (with teacher support), and (2) to assess the impact of surface biocontamination on students’ health using desktop ATP level as the exposure indicator, and the district data on illness absence as the outcome variables.
Material and methods
The study included a sample of 34 K-8 schools selected from a 57-school district located in the Western US. For the first study objective, the schools were randomly divided into two groups: (1) 17 intervention schools implemented enhanced cleaning and disinfecting in classrooms, and (2) 17 controls continued cleaning as usual. The sample size was determined using pilot data to achieve a minimum of 80% power to detect a difference in absence rates between the intervention and control groups of schools, using simple sample size calculation method for cluster-randomized trials [17]. At the time of the study, there were a total of 29,498 students in the district; there were 15,814 students in the 34 schools included in the study. Preparations, including training of the custodians and teachers in the intervention schools, were done in the fall of 2019 and the actual study was conducted between January 7 to March 14, 2020.
District data compiled from the study period included student level information on absence and socio-demographic variables, including grade level, gender, ethnic group, and eligibility to free or reduced lunch. Each student’s absences were recorded by the district using a unique student ID, date of absence, and reason for absence (if known). The reporting was based on parent reporting of student illness; there was no requirement for associated medical documentation. Full definitions related to absences are shown in Table 1. The main outcome variables were probability of absence per week due to respiratory or gastrointestinal illnesses.
Table 1.
Absenteeism data definitions and frequency reported in the spring 2020.
| Reason for absence | Explanation | N | % |
|---|---|---|---|
| Documented absence | Student is not attending school or individual class. A document has been presented to excuse the absence. i.e., doctor’s note or legal issue documented. | 8033 | 8.9 |
| Excused absence | Student is not attending school or individual class. Parent excused absence for reason other than illness. | 34,863 | 38.8 |
| Illness | Student is not attending school or individual class. Parent has stated the student is ill and has not given specific detail. There is no doctor’s document provided. | 33,259 | 37.0 |
| Illness gastrointestinal | Student is not attending school or an individual class for gastrointestinal related illness, such as nausea, vomiting or diarrhea. Parent has stated the student is ill. There is no doctor’s document provided. | 5882 | 6.5 |
| Illness respiratory | Student is not attending school or an individual class for respiratory related illness, but not asthma, such as runny nose, sore throat, congestion, or cough. Parent has stated the student is ill. There is no doctor’s document provided. | 7604 | 8.5 |
| Illness asthma | Student is not attending school or an individual class for asthma related illness. Parent has stated the student is ill. There is no doctor’s document provided. | 168 | 0.2 |
| Total | 89,809 | 100.0 |
Weekly absences correspond with total counts of students absent each week over the study period, and the percentage of weekly absences corresponds with total counts of students absent divided by total number of students * weeks. The binary student level absence data were used to calculate the probability of absence per week (based on any absence, and absence due to respiratory or gastrointestinal illnesses). It means that for every week of monitoring, each student is rated absent, if they missed 1–5 days of school for the given reason(s). As an example, a school level mean probability of 0.22 means that 22 out of 100 students each week are likely to be reported absent for any reason. Similarly, about two students are likely to be reported absent due to respiratory and gastrointestinal illnesses.
The enhanced cleaning protocol in the intervention group of schools was implemented in all classrooms thorough the school and included the following main components:
Training of custodians and teachers, including importance of cleaning, consistency of cleaning, effective cleaning techniques, safe product use, and deterring use of unapproved agents.
Use of specific cleaning and disinfecting methods and materials, as well as increased cleaning frequency of desktop surfaces.
External monitoring (by the research group) of cleaning effectiveness using ATP as a marker and providing regular feedback to school principals and custodians based on the monitoring results.
In addition to the main components, custodians and teachers could, at their voluntary discretion, invest in cleaning of high touch surfaces w/ disposable disinfecting wipes in the classrooms (ad hoc and/or as perceived to be needed) such as doorknobs, water fountain handles, or other similar surfaces.
Five focus rooms from each of 34 schools were selected for the assessment of the cleaning effectiveness. These rooms were carefully chosen to be representative of different building zones, e.g., in terms of year of construction, HVAC, and occupancy characteristics, with adjacent rooms thoroughly investigated (using spot check measurements) prior to selection. In addition, as a part of an ongoing district wide renovation program, the schools had been thoroughly investigated and the ventilation adequacy assessed based on long-term CO2 monitoring in 3–6 classrooms. The information about ventilation adequacy was collected and analyzed based on the following classification: (1) schools with all monitored classrooms inadequately ventilated, (2) schools with at least part of the classrooms adequately ventilated. The classrooms were considered adequately ventilated if the maximum (steady-state) CO2 levels were no greater than 700 ppm above outdoor air levels, as informed by ANSI/ASHRAE Standard 62.1.
In each focus room, a minimum of five desks were randomly selected for sampling by trained field technicians at designated times of the week. The time of sampling aligned with post-cleaning by custodial staff. However, the custodians did not know which classrooms or desks were being monitored. The sampling was done according to the same protocols as described in previous studies [15, 18]. The samples were immediately analyzed for area-normalized ATP levels using commercially available, handheld fluorescence monitors (Charm Sciences, NovaLum). A total of 7040 ATP samples were collected during the study period. With the goal of enforcing more consistent and effective cleaning, the principals and custodians of the intervention schools received regular feedback and were promptly alerted if the results were not indicating reduction of ATP levels.
Statistical analyses included descriptive statistics and the independent samples t-test for testing statistical significance between normally distributed continuous variables, and the chi-square test between categorical variables. Further, associations between log10-transformed ATP levels (LgATP) and absence were analyzed using general estimating equations (GEEs), which estimates population-averaged model parameters and their standard errors, using binomial distribution with logit link. School and student IDs were used as (repeated) subjects and week number as a within subject variable. Weekly mean LgATP was used as the independent variable.
In addition to the basic models, an additional model was fitted by stepwise selection of covariates or possible confounding factors or covariates including:
school and student level socio-demographic variables and the number of students (average head count),
weekly absence ratio, which could reflect between school differences in absence data recording, and
ventilation adequacy, which could be related to surface contamination as well as absence due illness.
Goodness of fit in selecting model variables in the final models was based on Corrected Quasi Likelihood under Independence Model Criterion (QICC) in smaller-is-better form, and variables that are not improving the model fit are excluded. The same principle was applied for selection of the working correlation structure, AR(1), where correlation decreases as a power of how many time points apart two observations are. (Repeated measurements commonly have a first-order autoregressive relationship).
Results
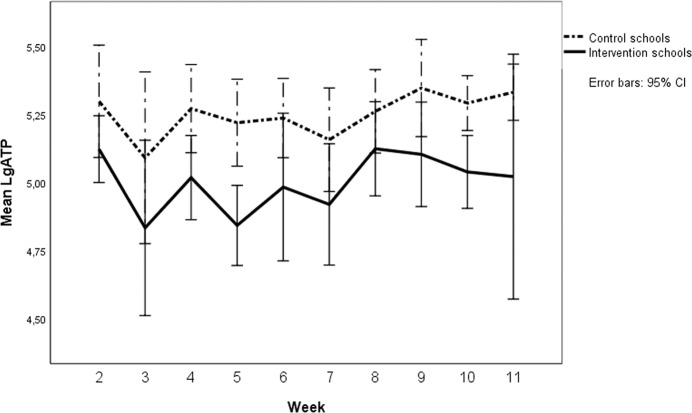
The overall average LgATP is 5.14 (SD 0.52): 5.26 (SD 0.48) for control schools and 5.02 (SD 0.53) for intervention schools. Weekly mean LgATP levels were significantly lower in the intervention group (p < 0.001) as shown in Fig. 1.
Fig. 1. Weekly averages for LgATP values in the intervention and control groups of schools.
Week 2 corresponds with the week of January 6, 2020, when the schools resumed after winter break, and the study began.
Reported frequencies of absence during the study period are shown in Table 1. Descriptive statistics related to student level data are shown in Table 2. In the sample of 34 schools, the average number of absences per student from the beginning of the school year was 7.2 (SD 6.4) and it was 3.0 (SD 3.2) during the 10-week study period. Statistically significant (p < 0.05) differences between intervention and control schools were seen in the age (based on grade level), socioeconomic status (based on eligibility for free or reduced lunch), and ethnic background.
Table 2.
Descriptive statistics related to illness absence and socio-demographic variables.
| Control schools | Intervention schools | |||
|---|---|---|---|---|
| N | % | N | % | |
| Grade levela | ||||
| Elementary school | 4528 | 47.3 | 5040 | 52.7 |
| Middle school | 3515 | 56.3 | 2731 | 43.7 |
| Gender | ||||
| Female | 3851 | 50.1 | 3837 | 49.9 |
| Male | 4192 | 51.6 | 3934 | 48.4 |
| Free or reduced luncha | 2092 | 59.7 | 1412 | 40.3 |
| Ethnic groupa | ||||
| Caucasian | 4957 | 47.2 | 5552 | 52.8 |
| Hispanic | 2170 | 63.5 | 1250 | 36.5 |
| Asian | 313 | 44.0 | 398 | 56.0 |
| Multi | 484 | 50.7 | 470 | 49.3 |
| Other | 119 | 54.1 | 101 | 45.9 |
| Ventilation assessment in the school | ||||
| Adequate in at least part of the classrooms | 9 | 42.9 | 12 | 57.1 |
| Inadequate in all classrooms | 8 | 61.5 | 5 | 38.5 |
aSignificant difference between intervention and control schools based on chi-square test (p < 0.05).
Summary of the weekly absence data are presented in Table 3. The binary student level absence data were used to the model the associations between the probability of absence per week (based on any absence, and absence due to respiratory or gastrointestinal illnesses) and weekly mean LgATP levels. First, we found a significant (crude) positive association (p < 0.05) between LgATP and reported absence due to gastrointestinal illness, with probability of 1.15 (1.00–1.33). The estimates for total absence and absence due to respiratory illness were 0.99 (0.94–1.05) and 0.88 (0.77–1.02), respectively, and not statistically significant. We also tested if the association would be stronger between weekly LgATP and the following week’s absence (possible lag period between exposure and illness onset), but no associations were found (data not shown).
Table 3.
Summary of weekly absence data used in the analyses.
| Control schools | Intervention schools | |||
|---|---|---|---|---|
| Na | %b | Na | %b | |
| Weekly absences | 12,629 | 22.0 | 11,532 | 21.6 |
| Weekly absences due to respiratory illness | 1055 | 1.8 | 1109 | 2.1 |
| Weekly absences due to gastrointestinal illness | 1409 | 2.5 | 1205 | 2.3 |
| Mean | SD | Mean | SD | |
| Probability of absence | ||||
| Any absence | 0.22 | 0.41 | 0.22 | 0.41 |
| Absence due to respiratory illness | 0.02 | 0.13 | 0.02 | 0.14 |
| Absence due to gastrointestinal illness | 0.02 | 0.16 | 0.02 | 0.15 |
| Head count | 546.49 | 186.01 | 496.85 | 115.36 |
| School level weekly absence ratioc | 21.83 | 5.94 | 21.01 | 5.88 |
aSum of students’ absence each week.
bPercent of absences over total number of students by week.
cNumber of students absent/total number of students.
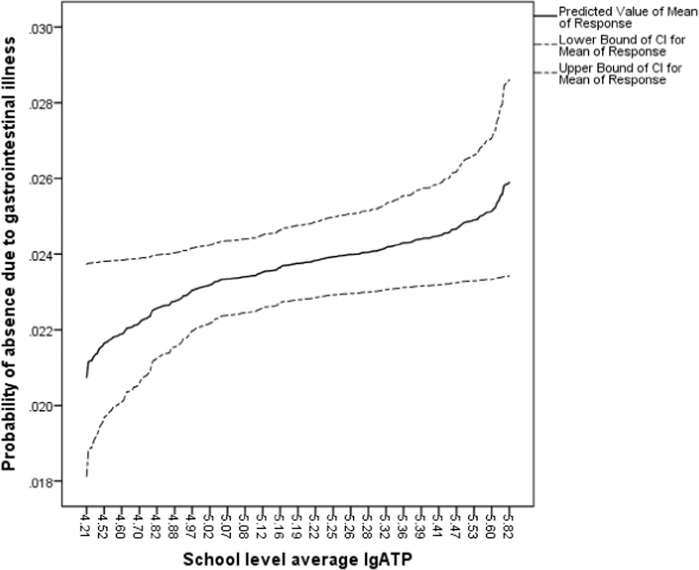
Stepwise fitting of variables resulted in selection of eligibility for free or reduced lunch, ethnic group, school headcount, school level weekly absence ratio, ventilation adequacy, and LgATP in the model. The final (best fit) model (A) for probability of absence due to gastrointestinal illness is presented in Table 4. The model results in increased probability of 1.16 (1.01–1.34), p = 0.037, for weekly average LgATP per unit (log) increase of ATP, where the multivariate GEE model accounts for student level gender, ethnic group, and socioeconomic status as well as for school level head count, total absence ratio, and ventilation adequacy in classrooms. Figure 2 illustrates the association between absence due to gastrointestinal illness based on the final model (A) and LgATP. Similar associations were not found between total absence and absence due to respiratory illness.
Table 4.
Final multivariate models for illness due to gastrointestinal illness.
| Model A | Model B | |
|---|---|---|
| Parameter | Exp(B) (95% CI), p | Exp(B) (95% CI), p |
| (Intercept) | 0.006 (0.003–0.012), <0.001 | 0.013 (0.011–0.016), <0.001 |
| Eligible for free or reduced lunch | ||
| Yes | 1.204 (1.074–1.350), 0.001 | 1.203 (1.073–1.349), 0.002 |
| No | 1 | 1 |
| Ethnic group | ||
| Other | 0.763 (0.661–0.882), <0.001 | 0.764 (0.661–0.882), <0.001 |
| Hispanic | 0.847 (0.751–0.956), 0.007 | 0.840 (0.744–0.949), 0.005 |
| Caucasian | 1 | 1 |
| School headcounta | 0.947 (0.920–0.974), <0.001 | 0.941 (0.915–0.968), <0.001 |
| School level weekly absence ratio | 1.046 (1.040–1.053), <0.001 | 1.046 (1.039–1.053), <0.0010 |
| Ventilation adequacy | ||
| Inadequate in all classrooms | 0.930 (0.846–1.024), 0.140 | 0.942 (0.859–1.034), 0.208 |
| Adequate in at least part of the classrooms | 1 | 1 |
| LgATP | 1.164 (1.009–1.344), 0.037 | – |
| Study group | – | |
| Intervention school | 0.914 (0.837–0.997, 0.042) | |
| Control school | 1 | |
aPer 100 students increase.
Fig. 2. Predicted propability of absence due to gastrointestinal illness plotted against weekly average LgATP.
Association between weekly probability of absence due to gastrointestinal illness and school level average LgATP.
Replacing LgATP with binary school classification (BIN = 0 control, 1 intervention school) in the multivariate model (A) yields parameter estimate 0.91 (0.84–1.00), p = 0.042, for the intervention group (model B, Table 4), indicating significantly decreased risk for absence due to GI illness as compared to the control group.
Discussion
As compared to a previous study presenting normal distributions for ATP levels on school desks, the reasonable range for post-cleaning (LgATP ≤4.72 as defined by Shaughnessy et al. [15]) was achieved by 10% of the control schools and 24% of the intervention schools. These results indicate that the cleaning was more effective in the intervention schools, however, even more rigorous cleaning efforts are needed to achieve the reasonable ATP range suggested in the previous study.
In the current study, ATP sampling occurred after the custodians had finished their cleaning routine. It often resulted in the study teams remaining onsite taking measurements deep into the evening, and no further occupancies occurred after that time until reentry in the morning. However, a window of a few hours was experienced between cleaning and sampling, during which time particles could have (re)settled on the desks and partially explain higher than expected ATP levels. Moreover, in some spaces (e.g., those with poor ventilation), the recontamination of desktops overnight, i.e., before students use the desks, may be substantial. Further studies should carefully consider the time of the sampling and how it may impact the results, as well as the optimal time of cleaning of the high contact surfaces in order to minimize the exposure. The results also show high within school variability, indicating challenges to maintain the same level of cleanliness across the school and over a long period of time.
Based on the results, within the range of LgATP observed, the probability of reported weekly absence due to gastrointestinal illness is estimated to increase from 0.021 to 0.026, which translates to one additional gastrointestinal illness case per 200 students per week. It should be noted that the actual number is likely to be larger due to underreporting of gastrointestinal illness, since majority of the illness absence was reported with non-specified reason. However, the relative increase is quite large (about 24%), and it appears that the extra effort invested in cleaning should pay off; also considering that the number of days the students, who become ill, are absent can vary considerably. In these data, the mean and median number of days the students are absent due to gastrointestinal illness is 1.0 and 1.5 (SD 0.95), and the range is 11. Many factors could impact on the severity of illness and how quickly each student recovers [19]. In addition to the cost related to student missing school are costs related to parents staying home from work, as well as the potential for spreading the infectious disease outside the school system.
Week was selected as the time unit, partially because it corresponds with the cleaning regimen, but also because students are exposed to infectious agents in schools during the week. For example, a review on viral gastroenteritis found median incubation periods from 1.2 days to 2 days for norovirus, sapovirus and rotavirus, and 4.5 days for astrovirus [20]. A recent study with the COVID-19 human coronavirus showed survival up to 2–3 days on plastic and stainless steel, 4 h on copper, and up to 24 h on cardboard [21]. Relatively little is known about the length of time such agents remain infectious, or the effectiveness of disinfection procedures to inactivate the virus [22].
We did not find an association between students’ absence due to respiratory illness and LgATP. A possible reason may be that viruses responsible for respiratory infections have multiple routes of transmission, including close personal contact, aerosol, and droplet nuclei, as well as multiple ports of entry including nose, mouth, and eyes. Also, other type of microbial exposures, such as mold and aeroallergens, that could increase the risk of respiratory or allergic illnesses among school children, may require more in-depth identification than what can be obtained from ATP measurements [18, 23]. On the other hand, gastrointestinal viruses and bacteria are transmitted primarily by the fecal-oral route and can persist on fomites for long periods of time. Therefore, this route of exposure maybe more likely and the impact of surface hygiene greater.
The results concur with Sandora et al. (2008), reporting results from an 8-week study in a single elementary school system [24]. The authors used clustered randomization to assign classrooms to intervention or control group, and the teachers of the study group were given a container of disinfecting wipes, while the students were given alcohol-based hand sanitizer. Illness absences, including respiratory and gastrointestinal illnesses, were recorded by school employee. After adjusting for race, health status, family size, and current hand-sanitizer use in the home, the absenteeism rate for gastrointestinal illness remained significantly lower in the intervention group than the control group (rate ratio: 0.91, p < 0.01). The adjusted absenteeism rate for respiratory illness was not different between the groups; the rate ratio was 1.10 (p = 0.12). However, any direct comparison of these two studies is challenging, for example, Sandora et al. studied the combined effect of using hand and surface sanitizing, whereas the current study was only considering surface sanitizing.
Hand hygiene is known to be very important in terms of protecting individuals from communicable disease, however, apart from education, it may not be easily enforced in schools [25]. On the other hand, enhanced surface sanitizing and monitoring its effectiveness could be developed into a possible district, state, or even national level policy to support heathy school environment. Moreover, improving the effectiveness of the cleaning would not necessarily result in additional costs: it could be achieved by a research-based approach, which emphasizes cleaning tradeoffs for health outcomes. Critical points to consider include frequency of cleaning of different surfaces (e.g., high touch surfaces), training the custodians and school personnel, as well as monitoring and feedback, the latter of which could be incorporated in the quality control/quality assurance procedures and perhaps commissioned.
From the exposure point of view, this study does not provide direct information on whether the microorganisms on the desks come from prior occupants of the desk or by settling from the classroom air. Further examination revealed that mean LgATP is slightly higher (5.25) in the group of schools where all investigated classrooms had inadequate ventilation, as compared to the group of schools that had adequate ventilation in at least part of the classrooms (5.05). The difference is statistically significant (p < 0.05) based on Kruskal–Wallis test. A possible explanation is that lower ventilation leads to slower removal of airborne particles, which can settle on desktops and other surfaces [18]. The ventilation assessment was based on separate investigations pertaining to this school district’s efforts in improving ventilation to meet the recommended standards. Therefore, we could not match the ventilation rates in the focus classrooms monitored for ATP but had to use a simplified school level classification. Based on previous studies, ventilation rates are quite representative of a long-term situation, providing the occupant density, systems or settings have not been changed [26]. Nevertheless, further studies are recommended to study possible interactions between ventilation rate in classrooms and surface cleanliness.
We measured ATP levels on desktops based a previous study that indicated lower absence rates in schools, which desktops ATP levels were rated “reasonable” both in the fall and winter. In addition to desktops, high ATP levels on bathroom stall doors appeared to reflect higher absence rates, but the differences were not statistically significant [18]. Surprisingly, the previous studies have found higher biocontamination levels on desktops than bathroom surfaces, which could be attributed to desktops not being cleaned as frequently [15]. On the other hand, ATP levels on cafeteria tables may be influenced by food residue [18]. In the light of these considerations, we decided to focus on monitoring desktops, not because they would be more important than other frequently touched surfaces, but rather because ATP readings seem to provide a more consistent indication of the surface cleanliness on desktops. In any case, ATP cannot be used as an indicator for pathogenic microbes [14].
There is a wide array of variables, which might confound a prospective study such as this one seeking to make the epidemiological linkage between surface biocontamination and health outcomes. Whereas the district data provided student level socio-demographic variables, there are numerous unknown variables related to students’ susceptibility to illness and even more so, being absent from school. In elementary schools the students are more likely to occupy the same classroom most part of the day, where desk cleaning could only provide limited protection from student-to-student transfer. On the other hand, middle school students often change classrooms and/or desks, resulting that desk cleaning might provide direct protection. However, based on the modeling results, grade level did not improve the model fit and it was therefore excluded from the final model. Whether or not the student change desks throughout the day or week, they share toilets, cafeterias, gyms, and other common areas, where the transmission could occur. While desktop ATP could be considered as an indicator of the level of biocontamination in schools, hygiene of the other types of surface areas is also significant as potential vector for disease transmission among school aged children and should be considered in the school or district level cleaning and assessment protocol.
The important contribution of this research is that a linkage is established between surface cleanliness and the risk of disease in a school population. Further studies are needed to fully understand the spread of various infectious diseases in school environments and the critical points of intervention.
Acknowledgements
The authors wish to thank Ms. Jana Black for assistance, as well as the personnel of the schools and the district for their dedicated efforts. In addition, the authors would like to recognize Charm, Inc. for loaning ATP monitors.
Author contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
Funding
The collection of ATP data and data analyses were funded by Reckitt Benckiser, who also supported the district by providing cleaning products for the intervention schools.
Data availability
The restrictions prohibiting the authors from making the data set publicly available are due to part of the data being obtained from a school district. The readers may contact the corresponding author for data requests.
Competing interests
The authors declare no competing interests.
Ethical approval
The research did not involve direct interaction with living individuals, or identifiable private information. The school district is collecting data on absence according to their own protocols. The data provided to the research group were de-identified. A data security plan was developed and approved by the district prior to obtaining data from the district. The plan details the issues related to handling the district data, including appropriate administrative, physical, and technical safeguards, and the way district data are collected, accessed, used, stored, processed, disposed of, and disclosed.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haverinen-Shaughnessy U, Shaughnessy R, Cole E, Toyinbo O, Moschandreas D. An assessment of indoor environmental quality in schools and its association with health and performance. Build Environ. 2015;93:35–40. doi: 10.1016/j.buildenv.2015.03.006. [DOI] [Google Scholar]
- 2.Mendell M, Heath H. Do indoor pollutants and thermal conditions in schools influence student performance? A critical review of the literature. Indoor Air. 2005;15:27–52. doi: 10.1111/j.1600-0668.2004.00320.x. [DOI] [PubMed] [Google Scholar]
- 3.Daisey JM, Angell WJ, Apte MG. Indoor air quality, ventilation and health symptoms in schools: an analysis of existing information. Indoor Air. 2003;13:53–64. doi: 10.1034/j.1600-0668.2003.00153.x. [DOI] [PubMed] [Google Scholar]
- 4.Willmott M, Nicholson A, Busse H, MacArthur GJ, Brookes S, Campbell R. Effectiveness of hand hygiene interventions in reducing illness absence among children in educational settings: a systematic review and meta-analysis. Arch Dis Child. 2016;101:42–50. doi: 10.1136/archdischild-2015-308875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toyinbo O, Matilainen M, Turunen M, Putus T, Shaughnessy R, Haverinen-Shaughnessy U. Modeling associations between principals’ reported indoor environmental quality and students’ self-reported respiratory health outcomes using GLMM and ZIP models. Int J Environ Res Public Health. 2016;13:385. doi: 10.3390/ijerph13040385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipsitch M, Viboud C. Influenza seasonality: lifting the fog. PNAS. 2009;106:3645–6. doi: 10.1073/pnas.0900933106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwan SE, Shaughnessy RJ, Hegarty B, Haverinen-Shaughnessy U, Peccia J. The reestablishment of microbial communities after surface cleaning in schools. J Appl Microbiol. 2018;125:897–906. 10.1111/jam.13898. [DOI] [PubMed]
- 8.Adams R, Miletto M, Taylor J, Bruns T. Dispersal in microbes: fungi in indoor air are dominated by outdoor air and show dispersal limitation at short distances. ISME J. 2013;7:1751–7362.. doi: 10.1038/ismej.2013.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grant C, Hunter CA, Flannigan B, Bravery AF. The moisture requirements of moulds isolated from domestic dwellings. Int Biodeterior. 1989;25:259–84. doi: 10.1016/0265-3036(89)90002-X. [DOI] [Google Scholar]
- 10.Roberts JW, Clifford WS, Glass G, Hummer PG. Reducing dust, lead, dust mites, bacteria, and fungi in carpets by vacuuming. Arch Environ Contam Toxicol. 1999;36:477–84. doi: 10.1007/PL00022756. [DOI] [PubMed] [Google Scholar]
- 11.Hospodsky D, Yamamoto N, Nazaroff WW, Miller D, Gorthala S, Peccia J. Characterizing airborne fungal and bacterial concentrations and emission rates in six occupied children’s classrooms. Indoor Air. 2015;25:641–52. doi: 10.1111/ina.12172. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto N, Bibby K, Qian J, Hospodsky D, Rismani-Yazdi H, Nazaroff W, et al. Particle-size distributions and seasonal diversity of allergenic and pathogenic fungi in outdoor air. ISME J. 2012;6:1801–11. doi: 10.1038/ismej.2012.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC. Guidance for school administrators to help reduce the spread of seasonal influenza in K-12 schools. 2012. http://www.cdc.gov/flu/school/guidance.htm.
- 14.Shama G, Malik DJ. The uses and abuses of rapid bioluminescence-based ATP assays. Int J Hyg Environ Health. 2013;216:115–25. doi: 10.1016/j.ijheh.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 15.Shaughnessy R, Cole EC, Haverinen-Shaughnessy U. ATP as a marker for surface contamination of biological origin in schools and as a potential approach to the measurement of cleaning effectiveness. J Occup Environ Hyg. 2013;10:336–46. doi: 10.1080/15459624.2013.784633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ISSA CLEAN STANDARD K-12 Schools 1014-2013, Measuring the Effectiveness of Cleaning. https://www.issa.com/certification-standards/issa-clean-standards/clean-standard-k-12 (Accessed 4 April 2022).
- 17.Hayes RJ, Bennett S. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol. 1999;28:319–26. doi: 10.1093/ije/28.2.319. [DOI] [PubMed] [Google Scholar]
- 18.Haverinen-Shaughnessy U, Khan S, Boulafentis J, Garcia C, Shaughnessy R. Effects of educational efforts in tribal homes and schools to reduce asthma triggers, symptoms and missed school days. Int J Hyg Environ Health. 2020;228:113513. 10.1016/j.ijheh.2020.113513. [DOI] [PubMed]
- 19.Hayward AC, Fragaszy EB, Bermingham A, Wang L, Copas A, Edmunds WJ, et al. Comparative community burden and severity of seasonal and pandemic influenza: results of the Flu Watch cohort study. Lancet Respiratory Med. 2014;2:445–54. doi: 10.1016/S2213-2600(14)70034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barker J, Vipond IB, Bloomfield SF. Effects of cleaning and disinfection in reducing the spread of Norovirus contamination via environmental surfaces. J Hospital Infect. 2004;58:42–49. doi: 10.1016/j.jhin.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Aboubakr HA, Sharafeldin TA, Goyal SM. Stability of SARS‐CoV‐2 and other coronaviruses in the environment and on common touch surfaces and the influence of climatic conditions: a review. Transbound Emerg Dis. 2021;68:296–312. doi: 10.1111/tbed.13707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee RM, Lessler JL, Rudolph KE, Reich NG, Perl TM, Cummings DAT. Incubation periods of viral gastroenteritis: a systematic review. BMC Infect Dis. 2013;13:446. doi: 10.1186/1471-2334-13-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borras-Santos A, Jacobs JH, Täubel M, Haverinen-Shaughnessy U, Krop E, Huttunen K, et al. Dampness and mould in schools and respiratory symptoms in children: the HITEA study. Occup Environ Med. 2013;70:681–7. doi: 10.1136/oemed-2012-101286. [DOI] [PubMed] [Google Scholar]
- 24.Sandora TJ, Shih M-C, Goldmann DA. Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatrics. 2008;121:e1555–62. doi: 10.1542/peds.2007-2597. [DOI] [PubMed] [Google Scholar]
- 25.Saunders-Hastings P, Crispo JAG, Sikora L, Krewski D. Effectiveness of personal protective measures in reducing pandemic influenza transmission: a systematic review and meta-analysis. Epidemics. 2017;20:1–20. doi: 10.1016/j.epidem.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Haverinen-Shaughnessy U, Moschandreas D, Shaughnessy R. Association between sub-standard classroom ventilation rates and students’ academic achievement. Indoor Air. 2011;21:121–31. doi: 10.1111/j.1600-0668.2010.00686.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The restrictions prohibiting the authors from making the data set publicly available are due to part of the data being obtained from a school district. The readers may contact the corresponding author for data requests.